Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 5
Diagnosis and Treatment of Silent Coronary Ischemia May Reduce Adverse Cardiac Events and Improve Long-Term Survival of Patients Undergoing Lower-Extremity Revascularization
Dainis Krievins1,2*, Edgars Zellans1,2, Gustavs Latkovskis1,2 and Christopher Zarins32Department of Medicine, University of Latvia, Riga, Latvia
3HeartFlow,Inc. Redwood City, California, USA
Received: 06-Aug-2021 Published: 07-Sep-2021, DOI: 10.35248/2329-6925.21.9.426
Abstract
Background: Patients with Peripheral Artery Disease (PAD) undergoing lower-extremity revascularization are at increased risk of death and Myocardial Infarction (MI) due to co-existing Coronary Artery Disease (CAD) which is often unrecognized due to absence of chest pain symptoms. A new cardiac diagnostic test, coronary CT-derived Fractional Flow Reserve (FFRCT), can identify patients with unsuspected (silent) coronary ischemia. We sought to determine whether pre-operative diagnosis of silent coronary ischemia using FFRCT can facilitate multidisciplinary care to reduce post-operative death and MI and improve survival of PAD patients.
Methods: Symptomatic PAD patients with no cardiac history or symptoms were enrolled in a prospective, open-label study of coronary CTA and FFRCT testing before lower-extremity revascularization and were compared to historic control patients with standard pre-operative cardiac evaluation and care. Lesion-specific coronary ischemia was defined as FFRCT ≤ 0.80 distal to a coronary stenosis. Endpoints included Cardiovascular (CV) death, MI and allcause death through 1 year follow up.
Results: Baseline characteristics of the CTA-FFRCT (n=135) and Control (n=135) groups were similar with regard to age (66 ± 8 years), gender, co-morbidities and indication for surgery (>80% for CLTI). CTA-FFRCT evaluation revealed unsuspected (silent) coronary ischemia in 68% of patients and 40% of patients had elective post-operative coronary revascularization (PCI in 47, CABG in 7). The status of coronary ischemia was unknown in Control patients and none had elective coronary revascularization. At one year, CTA-FFRCT had fewer CV deaths (0.7% vs. 5.9%, p=0.04) and MIs (2.2% vs. 8.1%, p=0.03) and improved survival (99.3% vs. 94.1%, p=0.02) compared to Control.
Conclusion: Pre-operative diagnosis of silent coronary ischemia in patients undergoing lower-extremity revascularization surgery can identify high-risk patients and facilitate multi-disciplinary patient care with selective post-operative coronary revascularization. This strategy reduced post-operative death and MI and improved one-year survival compared to standard care.
Keywords
Lower-extremity revascularization; Silent coronary ischemia; Coronary CT-derived fractional flow reserve; Coronary revascularization; Long-term survival
Introduction
Patients with symptomatic Peripheral Arterial Disease (PAD) have poor long-term survival due to co-existing Coronary Artery Disease (CAD) which is often unsuspected due to patients’ inability to walk and absence of chest pain symptoms [1]. Current guidelines recommend no pre-operative cardiac testing of PAD patients without cardiac symptoms since pre-operative coronary revascularization has not been shown to improve longterm survival [2]. Thus, despite strong evidence that symptomatic PAD is a consistent and powerful independent predictor of peri-operative cardiac events and mortality, patients with no cardiac symptoms usually undergo peripheral vascular surgery with no knowledge of the extent and functional significance of CAD, leaving them at high risk for early and late cardiac events [3]. The mortality rate following lower-extremity revascularization is > 20% at one year and > 50% at five years which is higher than for symptomatic CAD and most cancers [3,4]. Moreover, this high mortality has not changed over the past 30 years despite significant improvements in medical and interventional therapy [5].
A new non-invasive cardiac diagnostic modality, coronary CTderived Fractional Flow Reserve (FFRCT ) can identify patients with hemodynamically significant, ischemia-producing coronary stenosis. FFRCT analysis utilizes anatomic information provided by standard coronary CT Angiography (CTA) imaging with mathematical modeling of coronary blood flow to compute Fractional Flow Reserve (FFR) values throughout the coronary tree. Prospective clinical trials have shown good correlation of computed FFRCT to invasively measured FFR with accurate identification of patients with ischemia-producing coronary stenosis [6]. The clinical usefulness of FFRCT in patients presenting with symptoms of CAD is well documented and FFRCT analysis has been used to evaluate more than 75,000 patients with suspected CAD in Europe, US, Canada and Japan. However, the usefulness of FFRCT in patients presenting with symptoms of PAD needing surgery is unknown [7].
In 2017 we embarked on a prospective study of systematic preoperative evaluation of PAD patients using CTA and FFRCT to determine the prevalence of hemodynamically significant coronary artery stenosis in patients with no symptoms of CAD and to assess the usefulness of this information in patient management [8]. This article will highlight the findings of this study with a focus on the first peer-reviewed publication to show that pre-operative diagnosis of silent coronary ischemia using FFRCT with selective post-operative coronary revascularization may reduce death and myocardial infarction and improve survival of PAD patients following lower-extremity revascularization compared to control patients receiving current standard-of-care [9].
Materials and Methods
Pre-operative evaluation of PAD patients using CTA and FFRct
Patients with symptomatic lower-extremity PAD and no cardiac symptoms who were admitted to the hospital and cleared for elective revascularization surgery were enrolled in a prospective, institutional ethics committee approved study of pre-operative coronary CTA imaging with FFRCT analysis. After signing informed consent, standard coronary CTA imaging was performed in 135 patients with beta blockade for heart rate control and sublingual nitroglycerin for coronary vasodilation. CTA image datasets were sent via a secure web-based interface for off-site computational analysis of FFRCT (Heart Flow, Inc., Redwood City, CA). Results were returned within 24 hours and were available to treating physicians for patient management decisions.
Coronary CTA imaging revealed ≥ 50% stenosis in 70% of patients. Despite extensive coronary calcification (median Agatston score 905, IQR 390-1674, total range 0-4810), FFRCT analysis was successful in 93% of patients. In 9 patients FFRCT analysis could not be performed because of poor CTA image quality or due to excessive cardiac motion or image misregistration artifacts. Lesion-specific coronary ischemia (FFRCT ≤ 0.80) was present in 2 of 3 patients (68%) with severe ischemia (FFRCT ≤ 0.75) in more than half of patients (53%). Multivessel ischemia was present in 38% with left main ischemia in 7%.
Management of PAD patients with silent coronary ischemia
Results of protocol directed FFRCT analysis identified high-risk patients with unsuspected (silent) coronary ischemia but did not result in cancelation of scheduled lower-extremity revascularization in the majority of patients (96%). Limb-salvage surgery was performed in accord with current guidelines, driven by the pressing clinical need of critical limb ischemia in 86% of patients. Revascularization procedures were performed with cardiac anesthesia, continuous intra-operative monitoring and post-operative intensive care. There were no peri-operative deaths and all patients received optimal medical therapy following surgery. One patient had a MI on day 3 following aorto-femoral bypass and had successful emergency Percutaneous Coronary Intervention (PCI) with uneventful oneyear outcome. After recovery from surgery, patients with FFRCT evidence of significant silent coronary ischemia were selected for coronary angiography. Elective coronary revascularization was performed in 54 patients (63% of patients with silent ischemia, 40% of entire group) with percutaneous coronary intervention (PCI) in 47 patients and coronary artery bypass grafting (CABG) in 7 patients.
Control group of PAD patients receiving standard care
A group of 135 consecutive patients with no cardiac history or symptoms who underwent elective lower extremity revascularization surgery during the year immediately preceding initiation of the prospective study served as Controls. All patients met the inclusion and exclusion criteria of the prospective study and had undergone standard guidelinedirected pre-operative cardiac evaluation and post-operative care. The indication for surgery was CLTI in 82% of patients and revascularization was performed by the same team of experienced vascular surgeons, anesthesiologists, medical staff and critical care specialists as in the prospective study. All patients received optimal medical therapy following surgery and no patient had elective post-operative coronary angiography or coronary revascularization.
Comparison of CTA-FFRCT to control
The CTA-FFRCT and Control groups were well-balanced regarding baseline characteristics with no statistically significant differences in age (66 ± 8 years), gender, comorbidities, preoperative ankle-brachial index or type of surgery performed. The one-year outcome of the two groups was compared using the following endpoints: Cardiovascular (CV) death, Myocardial Infarction (MI) and all-cause death (survival).
One year outcome
Cumulative results at one year revealed that patients in the CTA-FFRCT group had fewer CV deaths (0.7% vs. 5.9%, 0.04), fewer MIs (2.2% vs. 8.1%, p=0.03) and improved survival (99% vs. 94%, p=0.02) compared to the Control group. Cumulative survival of the two groups at one-year (Kaplan-Meier estimates) is shown in Figure 1.
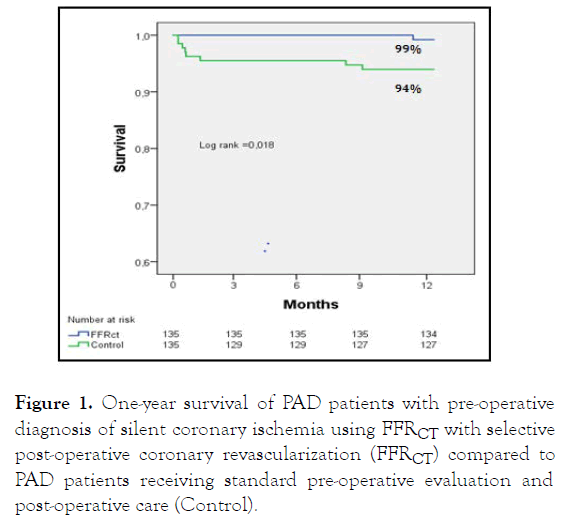
Figure 1: One-year survival of PAD patients with pre-operative diagnosis of silent coronary ischemia using FFRCT with selective post-operative coronary revascularization (FFRCT) compared to PAD patients receiving standard pre-operative evaluation and post-operative care (Control).
Results and Discussion
This study was the first to show the potential benefit of systematic pre-operative evaluation of PAD patients needing lower-extremity revascularization using coronary CTA and FFRCT analysis. This non-invasive assessment identified patients with asymptomatic (silent) ischemia-producing coronary stenosis who are at high risk for adverse cardiac events and premature death. While this did not result in cancellation of necessary limb-salvage surgery, results of FFRCT analysis allowed risk stratification of patients and facilitated multidisciplinary Vascular Team care with early cardiology involvement as recommended by guidelines [2]. This resulted in a significant reduction in CV death, MI and improved one year survival compared with historical controls with standard pre-operative cardiac evaluation and care. This improvement in outcome may have been due to an intensified focus on intra-operative and post-operative medical care or to selective post-operative coronary revascularization of patients with silent coronary ischemia, or a combination of the two. It seems reasonable to expect that if coronary revascularization was a significant contributing factor, then the benefit should become increasingly apparent with longer patient follow-up. In a recent report of 111 patients with CLTI and no known CAD, diagnosis of silent coronary ischemia using FFRCT with selective post-operative coronary revascularization resulted in improved two-year survival compared to 120 concurrent CLTI patients receiving standard peri-operative cardiac care (92% vs. 80%, p=0.02) [10].
This study is limited by the fact that it is a single-center, nonrandomized study in a real-world setting and has the potential for selection bias. While the results of this study are promising, they are not generalizable and should be considered hypothesis generating. Adequately powered, prospective, multicenter controlled trials are needed to define the role of CTA-FFRCT in the evaluation and treatment of patients with PAD.
Conclusion
PAD patients undergoing elective lower-extremity revascularization have a high prevalence (68%) of unsuspected (silent) coronary ischemia. Pre-operative diagnosis of silent coronary ischemia using coronary CTA and FFRCT can facilitate multidisciplinary patient care with selective post-operative coronary revascularization. This strategy reduced post-operative death and MI and improved survival compared to PAD patients receiving standard pre-operative evaluation and care. If confirmed by future studies, this strategy may improve long-term survival of patients with peripheral vascular disease.
REFERENCES
- Fridh EB, Andersson M, Thuresson M, Sigvant B, Kragsterman B, Johansson S, et al. Amputation rates, mortality, and pre-operative comorbidities in patients revascularised for intermittent claudication or critical limb ischaemia: A population based study. Eur J Vasc Endovasc Surg. 2017;54(4):480-486.
- Aboyans V, Ricco JB, Bartelink MEL, Bjorck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European society for vascular surgery (ESVS). Eur J Vasc Endovasc Surg. 2018;55:305-368.
- Beaulieu RJ, Sutzko DC, Albright J, Jeruzal E, Osborne NH, Henke PK. Association of high mortality with postoperative myocardial infarction after major vascular surgery despite use of evidence-based therapies. JAMA Surg. 2020;155(2):131-137.
- Mustapha JA, Katzen BT, Neville RF, Lookstein RA, Zeller T, Miller LE, et al. Disease burden and clinical outcomes following initial diagnosis of critical limb ischemia in the medicare population. JACC Cardiovasc Interv. 2018;11(10):1011-1012.
- Sigvant B, Kragsterman B, Falkenberg M, Hasvold P, Johansson S, Thuresson M, et al. Contemporary cardiovascular risk and secondary preventive drug treatment patterns in peripheral artery disease patients undergoing revascularization. J Vasc Surg. 2016;64(4):1009-1017.
- Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol. 2014;63(12):1145-1155.
- Nørgaard BL, Terkelsen CJ, Mathiassen ON, Grove EL, Bøtker HE, Parner E, et al. Coronary CT angiographic and flow reserve-guided management of patients with stable ischemic heart disease. J Am Coll Cardiol. 2018;72(18):2123-1234.
- Krievins D, Zellans E, Erglis A, Zvaigzne L, Lacis A, JÄ?gere S, et al. High prevalence of asymptomatic ischemia-producing coronary stenosis in patients with critical limb ischemia. Vasc Dis Manag. 2018;15(9):E96-E101.
- Krievins D, Zellans E, Latkovskis G, Erglis A, Zvaigzne L, Kumsars I, et al. Pre-operative diagnosis of silent coronary ischaemia may reduce post-operative death and myocardial infarction and improve survival of patients undergoing lower extremity surgical revascularisation. Eur J Vasc Endovasc Surg. 2020;60(3):411-420.
- Krievins D, Zellans E, Latkovskis G, Kumsars I, Jegere S, Rumba R, et al. Diagnosis of silent coronary ischemia with selective coronary revascularization might improve 2-year survival of patients with critical limb-threatening ischemia. J Vasc Surg. 2021.
Citation: Krievins D, Zellans E, Latkovskis G, Zarins C (2021) Diagnosis and Treatment of Silent Coronary Ischemia May Reduce Adverse Cardiac Events and Improve Long-Term Survival of Patients Undergoing Lower-Extremity Revascularization. J Vasc Med Surg. 9:426.
Copyright: © 2021 Krievins D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

