Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
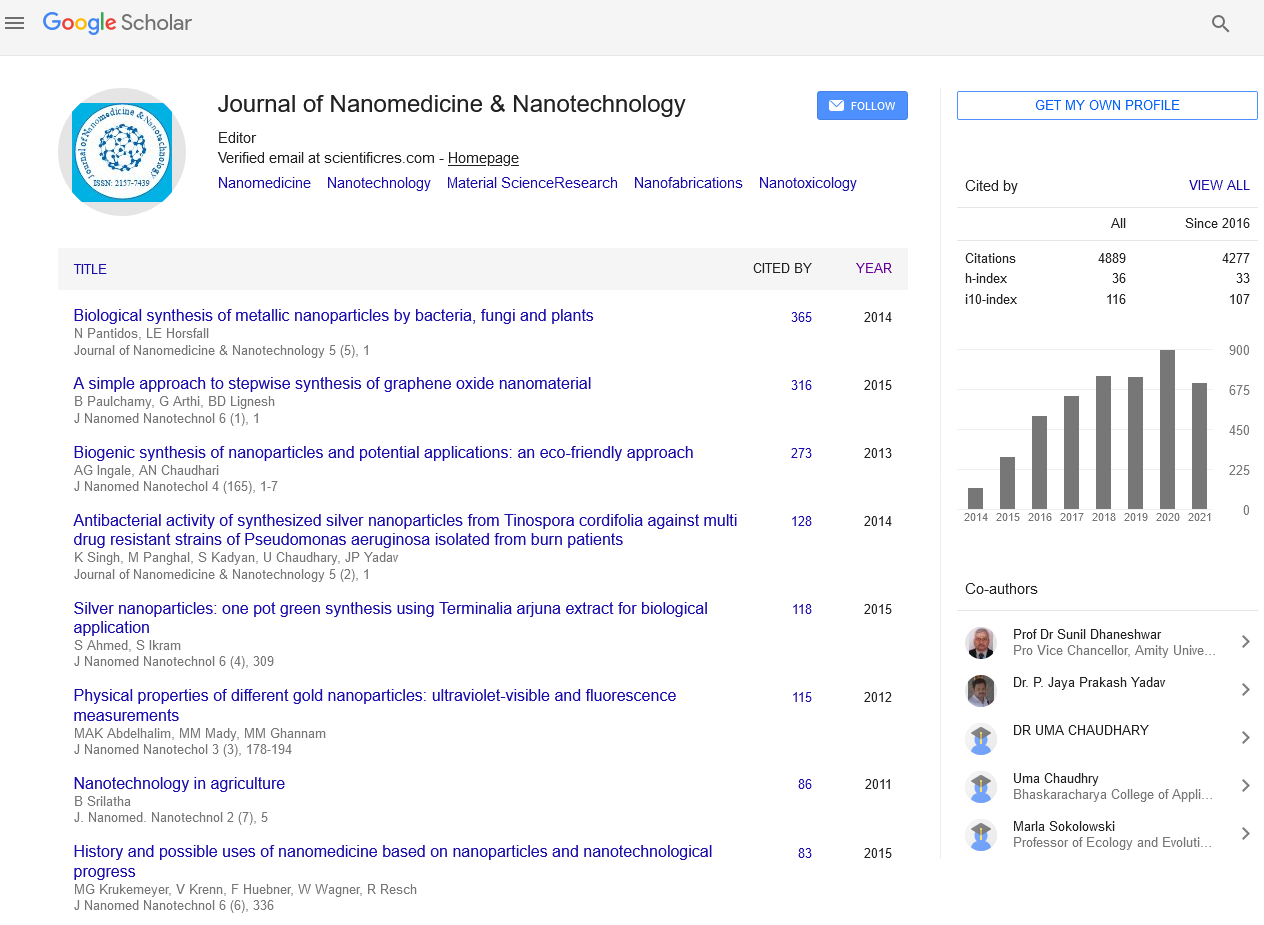
Mini Review - (2022) Volume 13, Issue 9
Determine Tumor Site-Dependent Transport Properties Delivery of Nanotherapeutics and Their Efficacy
Pranav Shende*Received: 03-Sep-2022, Manuscript No. jnmnt-22-18125; Editor assigned: 06-Sep-2022, Pre QC No. jnmnt-22-18125; Reviewed: 20-Sep-2022, QC No. jnmnt-22-18125; Revised: 23-Sep-2022, Manuscript No. jnmnt-22-18125; Published: 30-Sep-2022, DOI: 10.35248/2157-7439.22.13.638.
Abstract
Therapeutic effectiveness of anticancer medicines delivered systemically may be hampered by insufficient distribution of the medications to tumours. Can create therapeutic resistance based on drug delivery. PEGylated liposomal doxorubicin (PLD), for example, uses an increased permeability and retention effect to preferentially accumulate in tumours. Their clinical results and anticancer effects, however, vary widely amongst tumour types and are minimal. We looked into whether the tumour site affected the quantity and effectiveness of PLD delivered to tumours. We created mouse breast models with orthotopic primary tumours or liver metastases. Utilising 4 T1 cells for cancer PLD effectively treated cancers that developed in primary mammary tissue. but not in the liver, locations. We discovered that variations in treatment effectiveness were not caused by the intrinsic biological defence mechanisms in cancer cells but rather were linked to variations in transport characteristics that depended on the tumour site, such as the amount of PLD delivered, blood vessel function, relative vascular permeability, and mechanical pressure in tumours. As a result, site-dependent transport features in tumours can be employed as phenotypic surrogate markers for tumour drug delivery and therapeutic effectiveness.
Keywords
Heterogeneous; Genetic; Epigenetic; Transcription
Introduction
Heterogeneous reactions of cancers at various places to anticancer therapies that are systemically delivered have long been known in clinical settings. The exact causes of this site-specific heterogeneity are yet unknown, while resistance mechanisms based on the levels of genetic, epigenetic, and transcription factor in cancer cells have been investigated [1]. Cancer cells can also affect the growth and operation of tumor-associated blood arteries and the extracellular matrix as a result of cross-talk between cancer cells and the host microenvironment, which in turn affects the various transport properties within the tumours. Drug delivery might be hampered and therapeutic success can be impacted by the variability of these transport features in tumours [2]. Inadequate medication delivery to tumours below the concentration necessary to cause cytotoxicity in cancer cells generates even for agents, "transport-based therapeutic resistance" having demonstrated effectiveness in vitro against cancer cell lines Nanotherapeutics like doxorubicin in pegylated liposomal form (PLD), which are heavy-duty transport vans with broad systemic using the improved permeability and retention impact, pharmacokinetic profiles, and improve medication delivery within tumours [3]. However, PLD's therapeutic effectiveness varies and has not considerably outperformed other anticancer treatments. Standard chemotherapy regimens in individuals with advanced breast cancer. According to this clinical evidence, PLD delivery to metastatic breast cancers is insufficient and inconsistent. Therefore, to better understand the mechanisms underlying the variety of tumour responses to PLD, it is crucial to ascertain the transport properties of malignancies [4]. Using syngeneic mouse tumour models, we have previously demonstrated the tumour type dependent differences in the transport characteristics of subcutaneous tumours, the amount of PLD delivery, and the therapeutic efficacy of lung and breast cancers. In this research, we discovered that syngeneic mice PLD efficiency varied depending on tumour site. Breast cancer models with primary tumours and liver metastases. We discovered that the variations can be ascribed to the PLD delivery and transport characteristics at each tumour site. As a result, site-dependent transport features in tumours can serve as phenotypic surrogates for therapeutic responses [5].
Material and Methods
Cell Culture
From and were used to obtain the 4 T1 murine breast cancer cell line exhibited by ATCC (Manassas, VA). The cells were grown in a complete minimal essential medium containing 10% foetal bovine serum and a penicillin-streptomycin cocktail
Mice
Aged 5-7 weeks, female BALB/c mice were purchased from Laboratory Charles River (Wilmington, MA). The rodents were kept in Houston Methodist Research Institute animal facilities that have received approval from the American Association for Accreditation of Laboratory Animals.
Establishment of Primary Tumor
1 x 10 5 4 T1 cells in 100 L are required to create the primary tumour. The mouse mammary fat pad was injected with phosphatebuffered saline. Another group of mice were given an injection of 4 T1 cells (1 10 5/100 L) into the spleen body, followed by splenectomy, to create experimental liver metastases. The portal vein allows the cells injected into the spleen to spread to the liver. The Institutional Animal Care and Use Committee of the Houston Methodist Research Institute gave its approval to each protocol [6].
Therapy and Necropsy
Nine days after being injected with tumour cells, mice harbouring Infusions of PBS (n = 5) or 8 mg/kg PLD were administered intravenously to patients with primary tumours or liver metastases. Formula Scientific's DoxovesTM-Liposomal Doxorubicin HCl (n = 5) Inc., Palo Alto, California. Afterward, mice that had tumours were six days after therapy, sacrificed. For upcoming analyses, primary tumours or livers were removed, frozen, and kept at 80 °C. The following techniques were used to assess the therapeutic effectiveness of PLD against tumour growth: (1) the size of the primary tumour was measured, and tumour volume (V) was calculated using the formula V = 1/2 (length width 2), and (2) the size of liver metastases was calculated from twodimensional tumour measurements (the sum of the longest diameter and its longest perpendicular diameter for each tumour). On an immunofluorescence image that was obtained using image software [7] [8]. When tomato lectin is injected intravenously, it causes labelling of operative blood vessels. Another group of tumor-bearing mice (Day15, n = 5/tumour site) were treated with tomato lectin dyed with 488 Daylight. (100 g/100 l) was injected. The inferior vena cava was cut, the left ventricle was injected with 10 mL PBS and 10 mL of 4% paraformaldehyde, and tumours were removed five minutes after the injection.
Immunofluorescence Imaging of Tumor Cell Proliferation
In 4% paraformaldehyde in PBS, frozen sections were fixed. For the slices were blocked with blocking solution 0.3% Triton X, 5% horse sera, and 1% goat sera in PBS before Ki67 labelling to image cell proliferation. After adding Alexa Fluor® 488 anti-rabbit IgG to the blocking solution, anti-Ki67 antibody (ab15580) from Abcam, Cambridge, MA, was added. A TUNEL assay was carried out in accordance with the manufacturer's instructions to assess cell apoptosis. All pictures were taken with an A1 Nikon microscope [9].
PLD Delivery to Primary Tumors and Liver Metastases
Mice with primary liver metastases or tumours were intravenously given. PLD was administered as previously mentioned (n = 5/each site) to assess PLD delivery to tumours. In the past, we examined PLD kinetics in 4 T1 tumours and discovered that the t max was 24 hours after intravenous injection. In the present investigation, mice were slaughtered 24 h after injection, and primary tumours or livers were collected for immunofluorescence imaging [10]. Using the wide-field imaging system Image press Micro, frozen sections were labelled with DAPI and PLD accumulation into the tumour was assessed by imaging the ruby red fluorescence of at the excitation and emission wavelengths of doxorubicin (DOX), both 488 and 590 nanometers [11].
Discussion
Understanding the functions that tumour site-dependent the effectiveness of PLD therapy is influenced by medication delivery and transport qualities. In order to determine the effects of PLD on tumour cell growth and apoptosis, we first used a pharmacodynamics technique. This method was employed to identify tumour cells in which PLD was administered in high enough amounts to cause cytotoxicity. We assessed PLD delivery to the tumours using imaging anthracycline immunofluorescence to ascertain the cause of the variations in pharmacodynamics [12]. We discovered significant disparities in the levels of doxorubicin given to tumours at different sites. These findings imply that while creating novel therapies and evaluating their effectiveness in in vivo tumour models, research must now consider tumour locations. PLD buildup was examined in the prior study's mice with 4 T1 brain metastases. Fascinatingly, 4 T1 PLD accumulated tumours in the brain, and PLD injection dramatically increased the survival of the mice with tumours. We also discovered that 4 T1 liver metastases were consistently insensitive to PLD. Regardless of systemic therapy with PLD or control PBS, the average size of liver metastases in this trial rose from 250 mm to 500 mm in 4 days.
Conclusion
Additionally, we examined the administration and therapeutic effectiveness of PLD using the 3LL tumour type, which is a mouse lung cancer that grows subcutaneously or in the brain. Regardless of tumour site, PLD did not accumulate 3LL tumours, and it did not prolong the lives of mice with 3LL tumours. While PLD demonstrated a considerable anti-tumor effect in primary tumour models, it was unable to stop the progression of lung metastasis. Found that much increased 64Cu labelled liposome accumulation into several mouse tumour models was related with anti-tumor activity following administration of various liposomal medications. Lee et al. demonstrated in a clinical investigation that higher tumour Patients with metastatic breast cancer who had 64Cu tagged liposomal doxorubicin in their bodies had better treatment outcomes. These findings imply that a biomarker strategy for tailoring nanoparticle-based therapies can be established using the nanoparticle imaging approach now used in clinics.
REFERENCES
- Magnuson BA, Jonaitis TS, Card JW. A brief review of the occurrence, use, and safety of food-related nanomaterials. J Food Sci. 2011; 76(6):126-133.
- Hayat T, Qayyum S, Imtiaz M, Alsaedi A. Impact of Cattaneo-Christov Heat Flux in Jeffrey Fluid Flow with Homogeneous-Heterogeneous Reactions. PLoS One. 2016; 11(2):0148662.
- Chang XL, Yang ST, Xing G. Molecular toxicity of nanomaterials. J Biomed Nanotechnol. 2014; 10(10):28-51.
- Alsaadi FE, Hayat T, Khan SA, Alsaadi FE, Khan MI. Investigation of physical aspects of cubic autocatalytic chemically reactive flow of second grade nanomaterial with entropy optimization. Comput Methods Programs Biomed. 2020; 183: 105061.
- Lai DY. Approach to using mechanism-based structure activity relationship (SAR) analysis to assess human health hazard potential of nanomaterials. Food Chem Toxicol. 2015; 85:120-126.
- Rhee JW, Wu JC. Advances in nanotechnology for the management of coronary artery disease. Trends Cardiovasc Med. 2013; 23(2):39-45.
- Balkany TJ, Whitley M, Shapira Y, Angeli SI, Brown K, Eter E, et al. The temporalis pocket technique for cochlear implantation: an anatomic and clinical study. Otol Neurotol. 2009; 30(7):903-907.
- Karimi M, Zare H, Bakhshian Nik A, Yazdani N, Hamrang M, et al. Nanotechnology in diagnosis and treatment of coronary artery disease. Nanomedicine Lond. 2016; 11(5):513-30.
- Martins RL, Rabelo ÉM, Tomazi R, Santos LL, Brandão LB, et al. Development of nano-emulsions based on Ayapana triplinervis essential oil for the control of Aedes aegypti larvae. PLoS One. 2021; 16(7):254-325.
- Ziemys A, Yokoi K, Kai M, Liu YT, Kojic M, Simic V, et al. Progression-dependent transport heterogeneity of breast cancer liver metastases as a factor in therapeutic resistance. J Control Release. 2018; 291:99-105.
- Yokoi K, Tanei T, Godin B, van de Ven AL, Hanibuchi M, Matsunoki A, et al. Serum biomarkers for personalization of nanotherapeutics-based therapy in different tumor and organ microenvironments. Cancer Lett. 2014; 345(1):48-55.
- Cui J, Li C, Guo W, Li Y, Wang C, Zhang L, et al. Direct comparison of two pegylated liposomal doxorubicin formulations: is AUC predictive for toxicity and efficacy?. J Control Release. 2007 Apr 2; 118(2):204-215.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Shende P (2022) Determine Tumor Site-Dependent Transport Properties Delivery of Nanotherapeutics and Their Efficacy. J Nanomed Nanotech. 13: 638
Copyright: ©2022 Shende P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.