Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 0, Issue 0
Determinants of Exclusive Breastfeeding Practice in Southern Ethiopia
Birkinesh Ermancho1, Tilahun Ermeko2*, Abate Lette2 and Abraham Tamirat32Department of Public Health, Madda Walabu University, Bale Goba, Ethiopia
3Department of Health, Behavior and Society, Jimma University, Jimma, Ethiopia
Received: 13-Sep-2021 Published: 04-Oct-2021, DOI: 10.35248/2090-7214.21.s9.002
Abstract
Exclusive breastfeeding for the first six months of life followed by optimal complementary feeding are critical public health measures for reducing and preventing morbidity and mortality in young children since breastfeeding supports infants’ immune systems and helps protect them from chronic illnesses later in life. However, rate of exclusive breastfeeding practice is very low especially in developing countries. The aim of this study was to evaluate the practice of mothers towards exclusive breastfeeding and identifying determinants of exclusive breastfeeding practice among mothers with index infant to six months.
A community based cross sectional study design was carried out from august to September, 2017. Face to face interview was conducted using pretested and structured questioner to collect data from mothers of index infant from 0 to 6 months of age. Forty five key informants were selected purposively from range of backgrounds for indepth interview on exclusive breastfeeding knowledge, perceptions and practices. The data was entered to Epi-data version 3.1 and exported to Statistical Packages for Social Sciences (SPSS) version 21.0 for analysis. A total of 591 respondents participated in the survey.
Only 88 (14.9%) of infants were exclusively breastfed. The majority 344 (58.2%) of the respondents hadn’t sufficient knowledge about exclusive breastfeeding, and only 222 (37.6%) of participants had positive attitude to exclusive breastfeeding. Initiation of breastfeeding within an hour after delivery was practiced by only a few mothers 194 (32.8%). Prelacteal feeds were given to above half of the infants 314 (53.1%). Sufficient knowledge and positive attitude towards exclusive breastfeeding, antenatal care ≥4 attendance, infant’s age (0-60 days), early initiation of breast feeding, and avoiding traditional prelacteal feeds can significantly raise the odds of exclusive breastfeeding practice.
Keywords
Exclusive breastfeeding; Infant’s health; Initiation time; Mothers; Prelacteal feeds; Knowledge; Attitude; Practice
Introduction
Breast feeding is an integral part of the reproductive process with important implications for the health of the mother and baby; it is a unique way of providing ideal food for the healthy growth and development of infants. Exclusive breastfeeding (EBF) means infant is given its entire nutrient from human breast milk and receives no even water, other liquids, tea, herbal preparations or any complementary foods during the first six months of life with the exception of vitamins, mineral supplements or medicines [1- 3]. Thereafter, infants should receive nutritionally adequate and safe complementary foods while continued breast feeding up to two years of age and beyond. Exclusive breast feeding for the first six months of life followed by optimal complementary feeding are critical public health measures for reducing and preventing morbidity and mortality in young children since breastfeeding supports infants’ immune systems and helps protect them from chronic conditions later in life such as obesity, diharria, respiratory infection, diabetes and heart diseases [4-6].
Formula feeding during the period of EBF increases the health risks to both the baby and mother. It raises the risk of death from diarrhea and incidence of acute respiratory tract infections in infants [7]. In addition, mothers also receive benefits from EBF as it helps to keep space between children, provide mother infant bondage, cardiovascular diseases, decreased risk for iron deficiency anemia, endometrial cancer, less risk of osteoporosis, decrease obesity, it is cost-effective, and reduce the risk of ovarian and breast cancers [8]. The family and society as a whole would also benefits by decreasing medical costs as sick care visits, prescriptions and hospitalizations, reduced environmental burden for the disposal of bottles and formula cans, reduced energy demands for the production and transportation of artificial feeding products [9].
Diminutions in child mortality are related with improved coverage of effective interventions to prevent or treat the most important causes of child death, especially timely initiation, exclusive breast feeding up to 6 months and ideal complementary feeding later, avoiding prelacteal feeds, essential immunizations, vitamin A supplementation, birth spacing, improve hygiene and sanitation, disease prevention and treatment [10]. According to WHO 2012 report 6.9 million under five children were died globally in 2011, an estimated 1 million lives could have been saved by exclusive breastfeeding [11]. Exclusive breastfeeding stands out as the least expensive and most effective intervention for child survival [12]. However, in developing countries, only 37% of children less than 6 months of age are exclusively breastfed (USAID 2017). Due to low quality of child health services, poor socio-economic conditions, and low level of maternal education and inadequate dietary intake, early childhood morbidity and mortality in several Sub-Saharan African countries have been unacceptably high. About 24% of children less than 5 years were reported to be moderately or severely underweight in sub-Saharan Africa. In eastern and southern Africa, the situation is almost alike, with 23% of under-fives being moderately or severely underweight [13,14].
Mothers’ employment, length of maternity leave, inadequate knowledge on breast feeding, negative attitude towards EBF, late initiation of breast feeding, prelacteal feeding, absence of ANC follow up, lack of social support and absence of self confidence in breast feeding are factors related with exclusive breastfeeding [15,16]. Different researches have shown that mothers with poor knowledge of EBF exhibit negative attitude about EBF and these accounts for the low rate of the practice. The key to successful breastfeeding is information, education and communication systems aimed at behavior change. Health information and education greatly influenced mothers’ knowledge, attitude and practice towards EBF (USAID 2017). Even though mothers can get information from different sources, the role of the health care professionals are significant in providing women with the information they need to make them accept and practice EBF [17,18].
In Ethiopia less than five years children mortality has dropped half from 166 deaths as of 1000 live births in 2000 to 88 deaths per 1000 live births in 2011. Likewise, the percentage of malnutrition in less than five years children has also dropped significantly in the previous ten years. For example, the rate of stunting dropped from 58% in 2000 to 44% in 2011 and the ratio of underweight has again reduced from 41% in 2000 to 29% in 2011 [19]. Even though inspiring results in the reduction of under-five morbidity and mortality, the rate of timely initiation of breastfeeding, reduction of prelacteal feeding and exclusive breast feeding practices have still less improved specially among rural communities of Ethiopia in the past decade. Therefore, the present study was designed to evaluate the practice of mothers towards exclusive breastfeeding and identifying its determinants in southern Ethiopia.
Materials and Methods
Study setting and sample
A community based cross sectional study was conducted from August to September 2017 in the rural community of Anlemo district, southern Ethiopia. According to the last census (Central Statistical Authority 2007), projection for 2017 the district has a total population of 89,319 with 2,879 children’s under one, 7,422 under three, 13,945 under five and 3,090 mothers at fertility age. Five health centers and 27 health posts are giving service to the community in the district. Fifty healthcare staffs are engaged in the health centers and 54 female health extension workers are also allocated to implement the health extension program at the community level.
Both quantitative and qualitative methods were used to collect data through face to face interview of mothers of index infant from 0 to 6 months age. Forty five key informants were selected purposively from range of backgrounds for in-depth interview on exclusively breastfeeding perceptions and practices.
The sample size was determined by using a single population proportion formula, ((zα/2)2 ×p (1-p)/d2) by considering the proportion of exclusive breastfeeding 50%, with a margin of error of 5% at the 95% confidence level, a design effect of 1.5 and adding 5% non-response rate, the final sample size was calculated to 605.
The multi-stage sampling method was used to select the study participants. In the first stage, 8 kebeles were randomly selected by lottery method from 27 rural kebeles in the district. Then, the sample was proportionally allocated to the selected kebeles. In the second stage, households with mothers having infants from 0-6 months were selected systematically (Kth) interval from health extension registration book. The next respondents were identified systematically forwards by adding cumulatively (Kth) intervals to the first randomly selected participant. We have randomly selected one mother if there were more than one eligible child with different mothers.
Research aims and current study
The quantitative data were collected using structured questionnaire, and the in-depth interview guide for qualitative data was developed after reviewing different literature [10-12]. A structured questionnaire was used to collect data on the sociodemographic characteristics, maternal and child characteristics, knowledge on breastfeeding, traditional beliefs and practices about infant feeding. In-depth interview guide was also used to create explanations of women’s knowledge, attitude and practices related to infant feeding. The main target of the in-depth interview was to capture mothers’ first-hand knowledge, attitude and practices about EBF. The questionnaire was prepared in English and translated to local language “Hadiyisa” and retranslated to English language by different independent language experts to confirm the reliability and content of translation. Eight diploma Nurses for data collection and two Bachelor of Science nurses were recruited for supervisors.
Two days training was given; this mainly dealt with the purpose of the study, handling ethical issues during data collection, and the technique of data collection using the prepared questionnaires, field methods, inclusion–exclusion criteria and record keeping. Pre-testing was carried out on 5% of the sample population prior to actual data collection in a rural kebele having similar status to the study community, and corrections were made to the questionnaire based on the pretest findings. Sixteen five-point Liker scale items, from “strongly disagree” to “strongly agree” were used to assess women's knowledge and attitude to breastfeeding , containing respondents’ knowledge and attitude to infants health, mother's health, cost effectiveness and effects on material relationship. The original Likert scale item was converted to a numeric scale (that means, 1, 2, 3, 4 and 5), with a higher score shows a higher participant's agreement with the item tested. The entire knowledge and attitude scores have been computed and indiscriminately classified at 2 levels: sufficient knowledge and positive attitude (score of 30.0 “75% of the total score of 40” and above) and insufficient knowledge and negative attitude (score less than 30.0) [20]. The computed variable has the mean 20.93 and a standard deviation of 4.551 for knowledge score and the attitude score has mean 23.99 and a standard deviation of 3.142. The Cronbach’s alpha confirmed internal consistency of the item, which was put at 0.997 for knowledge, and 0.977 for attitude items.
Data analysis
The completed questionnaires were coded and entered in to Epidata version 3.1 and exported to Statistical Packages for Social Sciences (SPSS) version 21.0 for analysis. The Likert scale items were re coded in to dichotomous variables to run binary logistic regression analysis. Frequency distribution, mean, standard deviation and percentage calculations were employed for most of the variables. Bivariate and multivariate logistic regressions analyses with 95% confidence interval (CI) were performed to test the statistical significance relationship between variables. First, crude odds ratios and 95% confidence intervals of each factor was done by using bivariate logistic regression to identify candidate variables for the multivariable model. Then, variables with P-value less than 0.25 in the bivariate analysis were selected for multivariable logistic regression. Finally, variables only P-value of less than 0.05 in multivariable analysis were taken as significance and included in the final model.
The qualitative data was analyzed by coding or tagging, organizing, probing, and comparing of the ideas. On the end of the discussion, participants were asked to provide records on final narrative. Once data are tagged or coded by theme, we sought the patterns among the themes. This might means understanding what kinds of people or conditions led to certain themes [21]. Responses were categorized under the themes and subthemes using an open coding system and the results were presented by narrative in triangulated with the quantitative outcomes by wellsaid verbatim of the study participants as illustrations.
Operational definitions
Attitude: Attitude was measured by asking 8 five point likert scale items. The total score has been computed and classified at 2 levels: Those who answer 75% and above were considered as positive attitude and below 75% were considered negative attitude [21].
Exclusive breastfeeding: Defined as infant is given its whole nutrient from human breast milk only and takes no even water, other liquids, tea, herbal preparations or any complementary foods for the first six months of life with the exception of vitamins, mineral supplements or medicines if indicated [22].
Early initiation: For this study it is defined as according to word health organization (WHO) recommendations the proportion of children put to the breast within the first hour of birth and ensures the infant receives colostrum [23,24].
Knowledge: Knowledge was measured by asking 8 five point likert scale questions. The total score has been computed and classified at 2 levels: Those who answer 75% and above were considered as sufficient knowledge and below 75% were considered insufficient knowledge [25].
Prelacteal feeds: Non-breast milk foods or any liquid or solid food given to infants before breastfeeding is initiated [26].
Traditional practice: It is the way of doing something that has existed for a long time in a particular group of societies as a religious or cultural belief [27,28].
Results
Socio demographic characteristics
A total of 591 mothers participated in this study, making the response rate of 97.7%. Four in ten (40.8%) of the participants were aged 26-35 years of age. About one-third (37.4%) of the respondents had children aged 60-120 days. The majority 469 (79.3%) of the participants were married. More than half (55.2%) of the respondents were Christian followers. Concerning educational level the majority 240 (40.6%) of the participants were illiterate. Three hundred thirty three (56.3%) of mothers were house wife. Forty four percent of respondents had husbands who completed elementary school. Two-thirds (65.8%) of participants had one to two children. Around 248 (42.0%) of mothers had at least 4 ANC visits. About half of the respondents (53.5%) of deliveries conducted in the home. The majority 475 (80.4%) of mothers had normal vaginal delivery (Table 1).
| Variables | Number | Percent |
|---|---|---|
| Mother’s age (in years) | ||
| ≤25 | 176 | 29.8 |
| 26-35 | 241 | 40.8 |
| >35 | 174 | 29.4 |
| Infants age (in days) | ||
| 0-60 | 179 | 30.3 |
| 61-120 | 221 | 37.4 |
| 121-180 | 191 | 32.3 |
| Marital Status | ||
| Married | 469 | 79.3 |
| Divorce | 73 | 12.4 |
| Widow | 49 | 8.3 |
| Religion | ||
| Christian | 326 | 55.2 |
| Muslim | 211 | 35.7 |
| Others | 54 | 9.1 |
| Educational Level | ||
| Illiterate | 240 | 40.6 |
| Elementary | 209 | 35.4 |
| Secondary and above | 142 | 24 |
| Occupation (mother’s) | ||
| Farmer | 135 | 22.8 |
| House wife | 333 | 56.3 |
| Governmental | 59 | 10 |
| Merchant | 64 | 10.9 |
| Husband’s educational level | ||
| Illiterate | 139 | 23.5 |
| Elementary | 261 | 44.2 |
| Secondary and above | 191 | 32.3 |
| Infant’s birth order | ||
| 1 to 2 | 389 | 65.8 |
| ≥ 3 | 202 | 34.2 |
| ANC attendance | ||
| No | 100 | 16.9 |
| 243 | 41.1 | |
| ≥ 4 | 248 | 42 |
| Place of delivery | ||
| Home delivery | 316 | 53.5 |
| Institutional delivery | 275 | 46.5 |
| Mode of delivery | ||
| Normal vaginal delivery | 475 | 80.4 |
| Caesarian section | 116 | 19.6 |
Table 1: Socio demographic characteristic of mothers in Anlemo district, Southern Ethiopia, 2017.
Knowledge and attitude of mothers to EBF
More than half (55.8%) of the mothers agreed that breast gives the baby all the needed nutrients during the first six months of life. One thirds (37.2%) of the respondents agreed that EBF infants have fewer diarrheas and BF helps for quicker recovery during illness. About half (54.3%) of the mothers disagreed that formula fed babies are more intelligent than breastfed babies. Regarding the attitude of mothers the majority (65.5%) agreed with EBF leads to child malnourishment. Above half (58.3%) disagreed that BF is stressful and boring to mothers (Table 2).
| Knowledge and attitude items | N | % | N | % | N | % | N | % | N | % |
|---|---|---|---|---|---|---|---|---|---|---|
| Knowledge | ||||||||||
| BF gives the baby all the needed nutrients during the first six months of life | 113 | 19.1 | 217 | 36.7 | 10 | 1.7 | 105 | 17.8 | 146 | 24.7 |
| EBF infants have fewer diarrheas and BF helps for quicker recovery during illness | 75 | 12.7 | 145 | 24.5 | 23 | 3.9 | 195 | 33 | 153 | 25.9 |
| Formula fed babies are more intelligent than breastfed babies | 108 | 18.3 | 129 | 21.8 | 33 | 5.6 | 170 | 28.8 | 151 | 25.5 |
| BF does not protect the mother against ovarian and breast cancer | 161 | 27.2 | 216 | 36.5 | - | - | 148 | 25 | 66 | 11.2 |
| BF does not protect the mother against postpartum hemorrhage | 112 | 18.9 | 188 | 31.8 | 42 | 7.1 | 164 | 27.7 | 85 | 14.4 |
| BF helps mothers to lose weight | 128 | 21.6 | 201 | 34 | 9 | 1.5 | 142 | 24 | 111 | 18.8 |
| BF reduce infant mortality due to common childhood illness | 200 | 33.8 | 217 | 36.7 | 38 | 6.4 | 83 | 14 | 53 | 9 |
| EBF is needed up to 6 month | 135 | 22.8 | 263 | 44.5 | - | - | 137 | 23.2 | 56 | 9.5 |
| Attitude | ||||||||||
| BF is stressful and boring to mothers | 68 | 11.5 | 167 | 28.2 | 11 | 1.9 | 181 | 30.6 | 164 | 27.7 |
| BF causes pains in the nipple | 118 | 20 | 188 | 31.8 | 31 | 5.2 | 159 | 26.9 | 95 | 16.1 |
| EBF leads to child malnourishment | 130 | 22 | 257 | 43.5 | - | - | 138 | 23.3 | 66 | 11.2 |
| EBF reduces family expenses | 167 | 28.2 | 205 | 34.7 | - | - | 105 | 17.7 | 114 | 19.3 |
| EBF makes infants uncomfortable | 93 | 15.7 | 140 | 23.7 | 7 | 1.2 | 215 | 36.4 | 136 | 23 |
| EBF makes the child very healthy | 153 | 25.9 | 176 | 29.8 | 2 | 0.3 | 150 | 25.4 | 110 | 18.6 |
| Prelacteal feed helps the baby | 95 | 16.1 | 148 | 25 | 31 | 5.2 | 159 | 26.9 | 158 | 26.7 |
| Colostrum is bad for infants health | 114 | 19.3 | 203 | 34.3 | 1 | 0.2 | 139 | 23.5 | 134 | 22.7 |
SA: strongly agree, A: agree, N: neutral, DA: disagree, SD: strongly disagree
Table 2: Knowledge and attitude towards exclusive breast feeding among mothers in Anlemo district, Southern Ethiopia, 2017.
Regarding the overall knowledge and attitude of mothers, the majority 344 (58.2%) of the participants hadn’t sufficient knowledge about EBF, and only 222 (37.6%) of mothers had positive attitude to practicing EBF confidently (Figures 1 and 2)
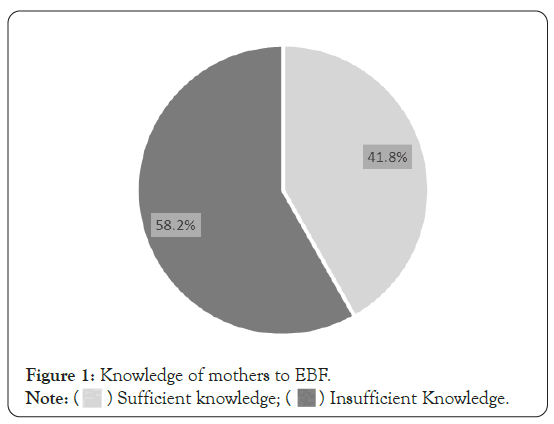
Figure 1: Knowledge of mothers to EBF.
Note: (  ) Sufficient knowledge; (
) Sufficient knowledge; ( ) Insufficient Knowledge.
) Insufficient Knowledge.
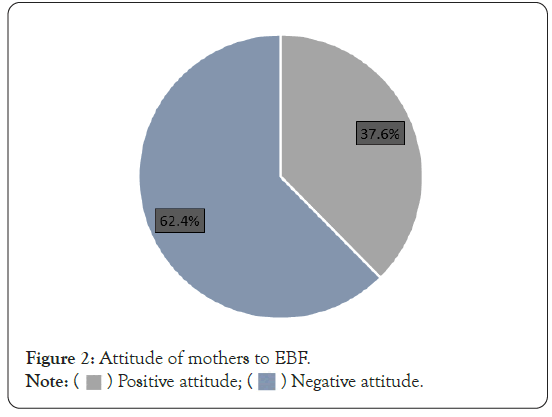
Figure 2: Attitude of mothers to EBF.
Note: (  ) Positive attitude; (
) Positive attitude; ( ) Negative attitude.
) Negative attitude.
Practice of mothers to exclusive breastfeeding
The majority 366 (61.9%) of respondents were educated about EBF. Among this Figure around half (50.8%) of them had heard from health professionals. However, only 186 (36.7%) of them knew correct meaning of EBF. Among the total participants, 256 (43.3%) of them believe that EBF is giving the baby breast milk and clean water for the first six months. The majority 395 (66.8%) of mothers hadn’t planned to EBF before birth. Only 88 (14.9%) of the mothers exclusively breast fed. About forty five percent of those who exclusively breastfed had children aged 0 to 60 days. The majority 397 (67.2%) of the mothers didn’t initiate breast feeding in the first hour of delivery. About half of the respondents, 314 (53.1%) of the respondents offered prelacteal feeds, and their traditions was the main reported cause 197 (62.7%).
One hundred ninety three (32.6%) of the mothers were developed breast problem. However, the majority 104 (53.9%) of them didn’t stop breast feeding during the breast problem. About 382 (64.6%) of the babies have ever been sick. Among the sick, 265 (69.4%) of them didn’t continue breast feeding. Regarding feeding frequency, the majority 256 (43.3%) of the respondents fed their baby less than 6 to 8 times per day. About 266 (45.0%) of less than five years children fed approximately for less than 20-30 min length of time for each BF. Only 108 (18.3%) of the mothers had regular feeding intervals whether a baby seems hungry or not (Table 3).
| Variables | Frequency | Percent |
|---|---|---|
| Have you ever heard about EBF? | ||
| Yes | 366 | 61.9 |
| No | 161 | 27.2 |
| I don’t know | 64 | 10.8 |
| If yes, where did you first learn about EBF, n=366? | ||
| Health professionals | 186 | 50.8 |
| Mass media | 53 | 14.5 |
| Friends or family | 127 | 34.7 |
| What is the meaning of EBF? | ||
| Giving the baby breast milk alone for six months | 217 | 36.7 |
| Giving the baby breast milk and infant formula | 94 | 15.9 |
| Giving the baby breast milk and clean water | 256 | 43.3 |
| Others | 24 | 4.1 |
| Have you planned EBF? | ||
| Yes | 196 | 33.2 |
| No | 395 | 66.8 |
| Did you EBF your child? | ||
| Yes | 88 | 14.9 |
| No | 503 | 85.1 |
| EBF by age (n=88) | ||
| 0-60 days | 40 | 45.4 |
| 61-120 days | 27 | 30.7 |
| 121-180 days | 21 | 23.9 |
| Did you initiate breastfeeding in the 1st hour of delivery? | ||
| Yes | 194 | 32.8 |
| No | 397 | 67.2 |
| If no, why (n=397)? | ||
| Clostridium is not good | 91 | 22.9 |
| Nipples pain | 108 | 27.2 |
| Breast milk did not flow on time | 119 | 30 |
| Baby was sick or sleep | 79 | 19.9 |
| Did you offer prelacteal feeds? | ||
| Yes | 314 | 53.1 |
| No | 277 | 46.9 |
| If yes, why (n=314)? | ||
| It is our tradition | 197 | 62.7 |
| It is good for the infant | 117 | 37.3 |
| What was given (n=314)? | ||
| Butter | 172 | 54.8 |
| Water | 127 | 40.4 |
| Other | 15 | 4.8 |
| Did you develop breast problems? | ||
| Yes | 193 | 32.6 |
| No | 398 | 67.3 |
| Did you stop breastfeeding during the breast problem (n=193)? | ||
| Yes | 89 | 46.1 |
| No | 104 | 53.9 |
| Has your child ever been sick? | ||
| Yes | 382 | 64.6 |
| No | 209 | 35.4 |
| Did you continue to BF even when the baby was sick (n=382)? | ||
| Yes | 117 | 30.6 |
| No | 265 | 69.4 |
| If you are BF, how many times do you feed your baby per day? | ||
| <6–8 times | 256 | 43.3 |
| ≥ 6–8 times | 179 | 30.3 |
| I didn’t remember | 156 | 26.4 |
| What is the estimated length of time for each BF? | ||
| <20-30 min | 266 | 45 |
| ≥ 20-30 min | 174 | 29.4 |
| I didn’t remember | 151 | 25.5 |
| When do you feed your baby? | ||
| When baby seems to be hungry or crying | 367 | 62.1 |
| At regular intervals whether baby seems hungry or not | 108 | 18.3 |
| When the breasts engorge | 116 | 19.6 |
BF: Breastfeeding, EBF: Exclusive Breast Feeding
Table 3: Mother’s practice towards exclusive breast feeding in Anlemo district, Southern Ethiopia, 2017.
Factors associated with exclusive breast feeding practice
Age of infants [AOR: 0.41, 9% CI: (0.15, 0.91)], Knowledge of mothers towards EBF [AOR: 2.04, 95% CI: (1.65,7.07)], ANC attendance [AOR: 5.74, 95% CI: (1.88,9.12)], attitude of mothers [AOR: 4.41, 95 % CI: (2.98,9.43)], initiation time of BF [AOR: 0.39, 95% CI: (0.12,0.84)], and prelacteal feeds [AOR: 3.50, 95% CI: (1.43,9.76)], were statistically significant variables in the multivariable logistic regression analyses (Table 4).
| Variables | EBF | OR(95% C.I) | |||
|---|---|---|---|---|---|
| Yes | No | COR, (95% C.I) | AOR, (95% C.I) | ||
| Age of infants (in days) | |||||
| 0-60 | 59 | 120 | 1 | 1 | |
| 61-120 | 18 | 203 | 0.59(0.16,0.83) | 0.53 (0.16,7.89) | |
| 121-180 | 11 | 180 | 0.52(0.18,0.97) | 0.41(0.15,0.91) | |
| Knowledge towards EBF | |||||
| Insufficient | 13 | 331 | 1 | 1 | |
| Sufficient | 75 | 173 | 2.88(1.13,11.60) | 2.04(1.65,7.07) | |
| ANC follow up | |||||
| No | 2 | 98 | 1 | 1 | |
| 1 to 3 | 32 | 211 | 1.99(1.22,5.67) | 2.44(0.79,4.61) | |
| ≥ 4 | 54 | 194 | 5.96(1.11,6.90) | 5.74(1.88,9.12) | |
| Attitude to EBF | |||||
| Negative | 9 | 360 | 1 | 1 | |
| Positive | 79 | 143 | 4.57(2.15,11.60) | 4.41(2.98,9.43) | |
| Early initiation | |||||
| Yes | 55 | 139 | 1 | 1 | |
| No | 33 | 364 | 0.37(0.10,0.76) | 0.39(0.12,0.84) | |
| Pre-Lacteal feeds | |||||
| Given | 20 | 294 | 1 | 1 | |
| Not given | 68 | 209 | 3.65(1.05,9.65) | 3.50(1.43,9.76) | |
Table 4: Factors associated with EBF practice, using multivariable logistic regression model, Anlemo district, Southern Ethiopia, 2017.
Discussion
In this study only 88 (14.9%) of mothers have practiced exclusive breastfeeding. This study was comparable with the study done in Hong Kong, 13.4% (Leung et al. 2006), In the United States, 13.3% (Ali 2014), in Mosul City, 15.0%, and the Nigeria Demographic and Health Survey (NDHS) in 2013 reported an exclusive breastfeeding rate of 17.0%. This finding was higher than the study conducted in different areas. Lower percent of exclusive breastfeeding practice were reported from mothers attending primary health care center in Saudi Arabia (7.3%), and much smaller proportions were listed from other regions of Saudi Arabia: in Riyadh only (0.8%) of children were exclusively breastfed for the first four to six months, and the amount increases to (1.7%) among babies at the age of six months in Jeddah (Ali 2014; Mahmoud et al. 2014). In rural area of Uttaranchal only (5.1%) of children were exclusively breastfed for the first six months, and in Orissa (8.6%) of respondents continued exclusive breast feeding up to six months of life. In the city of Feira de Santana, Brazil only (6.5%) of exclusive breastfeeding prevalence was stated (Vieira, Silva, and Vieira 2003). In Dhaka Slums, Sholeye reported (5.0%) of exclusive breastfeeding rate at six months of age while in the first month of life much higher mothers practiced it (53.0%). Another finding showed a prevalence of (3.3%) at six months of age among the first-time Chinese mothers whereas the proportion increased to (34.2%) at four months of age [29]. Much higher prevalence were reported from different regions, in Kumasi Metropolis, Ghana (48.0%) [30], in Calabar municipal, in Nigeria urban mothers (24%), in Egypt (68.0%) (Mahmoud et al. 2014), in Malaysia (44.1%), and around fifty percent was reported in Kwango district, Democratic Republic of the Congo [31]. These differences could be due to the variation in beliefs, traditions, and awareness towards child feeding among regions regarding EBF practice, the level of development in relation to education, health information dissemination and communication.
According to word health organization recommendation breastfeeding should be initiated within one hour of delivery. However, in this study only 194 (32.8%) of mothers’ commenced breastfeeding within an hour, and prelacteal feeds were practiced by 314 (53.1%) of participants. Different studies showed that late initiation of breastfeeding and giving prelacteal feed may be due to mother’s illiteracy, home delivery, wrong beliefs, lack of knowledge towards infant feeding, less milk secretion, fractured or inverted nipples, fear of previous nipple pain, mother too tired to feed; and baby was sleeping or sick. The most important reasons mentioned in the present study were family beliefs and traditions 197 (62.7%), some perceived that breast unable to secret milk on time 119 (30.0%), nipples pain 108 (27.2%), believed that clostridium isn’t good for infants 91 (22.9%), baby was sick or sleep 79 (19.9%), and some of them believe that prelacteal feed is good for infants 117 (37.3%).
This finding was supported by qualitative result as four house wives and two farmer mothers stated “….we didn’t remember the exact initiation time after delivery, but we didn’t initiate breast milk immediately after delivery because we were tired and the baby was also sleep”. And a 29 age merchant mother reported “….I was delayed to initiate breast feeding because we were busy with different activities such as cleaning the baby, cutting umbilical cord, and clothing him”. In addition, three government employee mothers reported “….we deferred to start breastfeeding since we were fear of nipple pain, and we perceived that breast milk start to flow by itself without be sucked by the baby.”
In the study area it’s very common beliefs that, child takes prelacteal feed like butter and water for his/her healthy life. This indicates that population of rural areas of Anlemo district believe more in traditions. Butter 172 (54.8%), and water 127 (40.4%) were the most popular prelacteal feeds used in the community. This finding was also supported by qualitative result as a 37 years merchant and 45 years government employee mothers reported “…some of we mothers in our kebele are giving very fresh butter to our newborn immediately after birth in addition we drop pure water in to his or her mouth with our fingers. These things make the child very healthy because it will wash and clean him from different dirty fluids inside him and it can also prepare the baby to suck the breast well.” In addition a 26 age health extension worker reported “…most of mothers were informed from us (health extension workers) and from 1 to 5 group leaders, so they already know the risk of giving prelacteal feeds, but some mothers practiced it especially when they delivered in their home with traditional birth attendance because they believe with their traditions.”
Mothers’ with infant age 121-180 days were 60% less likely practice exclusive breastfeeding compared to those who have baby of age 0-60 days. This result was comparable with different findings [32,33]. This finding also supported by qualitative result as a 40 year farmer mother reported “….we weren’t feeding our infants exclusively breast milk after 2 or 3 months because it can’t enough to him and even before graduating one month we gave fresh butter and clean water make him healthy by avoiding abdominal cramp and dryness during defecation.” And two house wives stated that “…it is impossible to feed only breast milk up to six months as we informed from health workers because our breast milk will reduce its milk production after three or four months but to the opposite the baby needs more food than before, so he crying, and open his mouth when we eat….” In addition a 32 years old farmer mother and two governmental worker mothers reported “…we couldn’t continue exclusive breast feeding after two months, we practiced complimentary feeding such as cow milk, even at one month of life to encourage and acclimate him to take foods later on.”
Another important finding of this study was that, the odds of exclusive breast feeding practice among mothers with sufficient knowledge and positive attitude were 2.0, 4.4 times more practiced exclusive breast feeding compared to their counterparts respectively. This result was in line with different studies. In Ethiopia, mothers with high knowledge of breastfeeding had more than 3 times higher odds of EBF compared with mothers with low knowledge of breastfeeding [34], and in Tanzania, mothers with “good” breastfeeding knowledge had more than 2 times higher odds of EBF compared with those with poor knowledge (USAID 2017). Chinofunga and Matiashe (2013, showed that maternal negative attitude caused interruption to exclusive breastfeeding among Vungu, Zimbabwe mothers. Therefore, the more the positive attitude towards EBF may indicate the more she is likely to practice exclusive breastfeeding [35].
Mothers who attend ANC 4 and above were 5.7 times more likely practice EBF compared with mothers who didn’t attend ANC or mothers had ANC 1-3 attendance. Different studies found a positive association between ANC attendance and EBF practice since ANC provides an opportunity to counsel women on EBF. It is the most appropriate time to inform and help mothers to plan and decide EBF before birth. In Nigeria, a study found that women who attend any ANC visit were 2.0 times more likely to practice EBF than those who didn’t attend, and in Kenya, women attending four or more ANC visits had 4.0 times more likelihood of practicing EBF than women who attended fewer than four ANC visits.
This study also identified that, late initiation and prelacteal feeding significantly reduced the odds of exclusive breast feeding practice. Mothers who didn’t initiate breast feeding within an hour after birth were 60% less practice EBF compared with their counterparts. This might be due to the fact that mothers had good awareness about early initiation and also they had good awareness about EBF. Besides, early initiation of breastfeeding is more common among children whose mothers were assisted at delivery by a health professional than among children delivered at home and so, they might get professional counsels. Mothers who didn’t give prelacteal feeding were 3.5 more practice EBF than mothers gave prelacteal feed. The reason for this could be mothers who have practiced prelactal feeding might be less knowledgeable about the time frame of initiating breast feeding and period of EBF, they might not be attend ANC and counseled abut EBF and also they might be delivered at their home by traditional birth attendants. This finding was agreed with different studies.
Conclusion
In conclusion, this study reported low rate of exclusive breast feeding practice compared with other findings in Ethiopia. Exclusive breast feeding practice may be enhanced by advancing mothers’ knowledge and attitude through education and counseling about benefits of exclusive breast feeding especially during ANC session, and by avoiding late initiation and traditional prelacteal feeding practices among the rural community.
Acknowledgements
We are grateful to Jimma University for supporting this study. We are also very grateful to mothers and data collectors to undertake this study.
Author’s Contributions
BE, AL, AT and TE developed the concept and method, collects data and drafts the manuscript, analyzed and interprets the data.
Funding
This study had not specific fund.
REFERENCES
- Agho KE, Dibley MJ, Odiase JI, Ogbonmwan SM, Sunday MO. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth. 2011;11(1):1-8.
- Akinyinka MR, Olatona FA, Oluwole EO. Breastfeeding knowledge and practices among mothers of children under 2 years of age living in a military barrack in southwest Nigeria. Int J MCH AIDS. 2016;5(1):1.
- Al-Hially Y. Assessment of mothersâ?? knowledge about breast-feeding and determining predictors. Tikrit Med J. 2010;16(2):77-83.
- Alemayehu T, Haidar J, Habte D. Determinants of exclusive breastfeeding practices in Ethiopia. Ethiop J Health Dev. 2009;23(1):13-18
- Ali ANA. â??Research article knowledge, attitude and practice regarding exclusive breastfeeding among mothers attending primary health care centers in Abha city.â? Int J Med Sci Public Health. 2014;3(11):11-13.
- TIa TA, WMb WM, Bb MI. Factors predicting early discontinuation of exclusive breastfeeding among women in Kelantan, Malaysia. Health Environ J. 2013;4(1):42-54.
- United States Agency for International Development (2016). â??MCSP Nutrition Brief Addressing Barriers to Exclusive Breastfeedingâ?¯: Evidence and Program Considerations for Low and Middle-Income Countries, 2017.â? no. USAID 2016:0-5.
- Chinofunga D, Matiashe I. Assessment of hindrances to exclusive breastfeeding among mothers in vungu. J Emerg Trends Educ Res Policy Stud. 2013;4(3): 547-52.
- Danso J. Examining the practice of exclusive breastfeeding among professional working mothers in kumasi metropolis of Ghana. Int J Nur. 2014;1(1):11-24.
- Dhakal S, Lee TH, Nam EW. Exclusive breastfeeding practice and its association among mothers of under 5 children in kwango District, DR Congo. Int J Environ Res Public Health 2017;14(5):455.
- Ekanem IA . â??Attitude of working mothers to exclusive breastfeeding in calabar municipality ,cross river state , Nigeria.â? J Food Res. 2012;1(2):71-75.
- Gaikwad L. â??Breastfeeding practices in an urban slum of western Indiaâ?¯: A cross-sectional study.â? Int Multidiscip Res J. 2014;1(7):65-69.
- Ethiopian Health and Nutrition Research Institute (EHNRI) (213). Assessment of status of infant and young child feeding (IYCF) practice, policy and programs: Achievements and Gaps, in Ethiopia.
- Kever RT, Dathini H, Martins SD, Inna AK, Habu H, Saidu MA, et al. knowledge of exclusive breastfeeding and proposed infant feeding pattern of post-natal mothers in Maiduguri. Nigeria. 2014;3(5):66-71.
- Leung EYL, Au KYA, Cheng SSW, Kok SY, Lui HK. Practice of breastfeeding and factors that affect breastfeeding in Hong Kong. Hong Kong Med J. 2006;12(6):432-436.
- Liben ML, Abel GW, Nejimu BZ, Afework M. â??Factors associated with prelacteal feeding in afar regional state , northeastern Ethiopiaâ?¯: A cross sectional study. Int J ResGranthaalayah. 2017;5(7):116-127.
- Mahmoud NA, Megahed NM, Essam MM, Marouf OB, Hussein EK, Mohamed KH, et al. Assessment of knowledge and practice of proper breastfeeding among mothers attending-El-Shohada primary health care units, Ismailia City. IJHS. 2014;2(1):70-78.
- Mbwana HA, Cath C, Pamela VH. â??Exclusive breastfeedingâ?¯: mothersâ?? awareness and healthcare providersâ?? practices during antenatal visits in mvomero , Tanzania.â? Int J Nutr Metab. 2013;5(1):40-49.
- Newby R, Wendy B, Robert SW, and Peter S. â??And beliefs predict antenatal intention.â? Breastfeed Med. 2014;9(5):266-272.
- Abebe B, Wondu G, Fekadu B. â??Exclusive breastfeeding knowledge of hiv positive mothers and associated factors in selected health.â? Univers J Food Nutr Sci. 2014;2(3):37-44.
- Premlata M, Hooja N, Bansal A, Salvi A, Makkar P. â??Knowledge , attitude and practice of breast feeding at a tertiary care centre in rajasthan.â? Scholars Acad J Biosci. 2014;2(10):714-718.
- Rahman N, Nikmah UD, Siti IF, Via O. â??Factors related to exclusive breastfeeding among mothers in the city of palu, central sulawesi, Indonesia.â? Mal J Nutr. 2017;23(2):175-189.
- Regassa N. Infant and child feeding practices among farming communities in Southern Ethiopia. Kontakt. 2014;16(4):215-222.
- Sanusi RA, Leshi OO, Agada UN. â??Motherâ??s knowledge and practice of breastfeeding and complementary feeding in enugu state, Nigeria.â? J Nurs Midwifery Res. 2016;5(1):21-29.
- Shaili V, Sharma P, Kandpal SD, Semwal J, Srivastava A, Nautiyal V. â??Original article a community based study on breastfeeding practices in a rural area of Uttarakhand.â? Natl J Community Med. 2012;3(2):283-287.
- Sholeye OO, Olayinka AA, Albert AS. â??Exclusive breastfeeding and its associated factors among mothers in sagamu , southwest nigeria.â? J Health Sci. 2015;5(2):25-31.
- Sitko NJ. â??Designing a qualitative research projectâ?¯: Data collection and methods Interactive Model of Research Design.â?2013.
- Tewabe T, Mandesh A, Gualu T, Alem G, Mekuria G, Zeleke H. Exclusive breastfeeding practice and associated factors among mothers in motta town, east gojjam zone, amhara regional state, ethiopia, 2015: a cross-sectional study. Int Breastfeed J. 2016;12(1):1-7.
- Vieira GO, Silva LR, Vieira TD. Child feeding and diarrhea morbidity. J Pediatr. 2003;79(5):449-454.
- Wan H, Tiansawad S, Yimyam S, Sriaporn P. Factors predicting exclusive breastfeeding among the first time Chinese mothers. Pac Rim Int J Nurs Res. 2015;19(1):32-44.
- World Health Organization (WHO) (2003). Global strategy on infant and young child feeding. Geneva, World Health Organization.
- Central Statistical Authority (CSA) (2007). Summary and statistical report of the 2007 population and housing census results. Addis Ababa, Ethiopia.
- Yeneabast T, Belachew T, Haile M. Determinants of cessation of exclusive breastfeeding in ankesha guagusa woreda, awi zone, northwest Ethiopia: A cross-sectional study. BMC Pregnancy Childbirth. 2014;14(1):1-2.
- Egata G, Berhane Y, Worku A. Predictors of non-exclusive breastfeeding at 6 months among rural mothers in east Ethiopia: A community-based analytical cross-sectional study. Int Breastfeed J. 2013;8(1):1-8.
- Ugboaja JO, Berthrand NO, Igwegbe AO, Obi-Nwosu AL. Barriers to postnatal care and exclusive breastfeeding among urbanwomen in southeastern Nigeria. Niger Med J. 2013;54(1):45.
Citation: Ermancho B, Ermeko T, Lette A, Tamirat A (2021) Determinants of Exclusive Breastfeeding Practice in Southern Ethiopia. Clinics Mother Child Health. S9:002.
Copyright: © 2021 Ermancho B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

