Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 2
COVID-19 Vaccine Hesitancy and Subsequent Uptake among Healthcare Personnel at an Academic Medical Centre in California, 2021
Margot Bellon1, John Shepard2, Janet Wei2, Jorge L Salinas1, Clea Sarnquist1, Saud Khan1, Eric Hadhazy1, Yvonne Maldonado3 and Jennifer B Bollyky3*2Department of Quality, Patient Safety and Clinical Effectiveness, Stanford Health Care, Stanford, CA, United States of America
3Department of Pediatrics, Division of Infectious Diseases, Stanford University School of Medicine, Palo Alto, CA 94304, United States of America
Received: 23-Feb-2023, Manuscript No. JVV-23-19995; Editor assigned: 27-Feb-2023, Pre QC No. JVV-23-19995; Reviewed: 10-Mar-2023, QC No. JVV-23-19995; Revised: 17-Mar-2023, Manuscript No. JVV-23-19995; Published: 27-Mar-2023, DOI: 10.35248/2157-7560.23.14.512
Abstract
Despite widespread availability of COVID-19 vaccines in the United States, 23% of Health Care Personnel (HCP) was unvaccinated as of December, 2021. This study identified characteristics of hospital-based healthcare personnel associated with delaying or declining COVID-19 vaccination. We analyzed surveys from >15,000 hospital-based HCP from a large, university-based healthcare system in December 2020 to understand employee plans for COVID-19 vaccination. We also assessed changing one’s mind about getting vaccinated between December 2020 and March 2021. We found that being female, black, and between ages 18 and 49 was associated with delaying or denying the vaccine. HCPs from counties of high social vulnerability and those with less patient contact also had higher rates of vaccine hesitancy. The HCP sub-groups that express high rates of vaccine hesitancy should be considered in the design of vaccination campaigns for hospital workers.
Keywords
COVID-19 vaccine; Healthcare worker; Healthcare personnel; Vaccine hesitancy
Introduction
Vaccine hesitancy is one of the primary barriers in mitigating COVID-19 morbidity and mortality. Despite widespread availability of COVID-19 vaccines in the United States, 23% of U.S. Healthcare Personnel (HCP) were reportedly still unvaccinated as of December, 2021 [1]. HCP have been a priority population for the study of SARS-CoV-2 infection and vaccination rates during the COVID-19 pandemic given their critical role in patient care and potentially increased exposure to the virus. HCP attitudes toward the COVID-19 vaccine have been shown to vary by gender, race, and geographic location, with women, black, LatinX, and rural HCPs less willing to accept the vaccine. Vaccine acceptance has been shown to be higher with increasing age, education, and income level [2]. HCPs who have declined the COVID-19 vaccine have reported concerns about speed of approval, effectiveness, and safety as the most common reasons for vaccine hesitancy [3].
It has been shown that gender and socioeconomic status interact to influence vaccine hesitancy. For example, women living in poverty were more vaccine-hesitant than women in higher socioeconomic brackets, while poverty and employment status did not affect men’s vaccine hesitancy. However, not having a college education contributed to both women’s and men’s COVID-19 vaccine hesitancy. Overall, those with lower income and less education are less likely to get a COVID-19 vaccination, but other studies found those who lost a job were more likely to accept a COVID-19 vaccine than those who continued to work throughout the pandemic [4,5]. Other research has shown that respondents who feel that the COVID-19 vaccine is unsafe are significantly more likely to be from rural areas and from lower income segments [6]. Furthermore, women are more worried about the safety of the vaccine than men, but men’s hesitancy tends to be driven by lower perceptions of COVID-19 dangers and belief in conspiratorial claims.
To inform specific and effective vaccination campaigns for hospitals, it is important to understand which employees are vaccine-hesitant and why. We surveyed HCPs at a large, university-based healthcare system regarding their vaccine intentions before the vaccine became widely available and hospitals began mandating the COVID-19 vaccine. We compare these vaccination intentions with actual vaccination records to better characterize and plan interventions for vaccine-hesitant HCP. These results can be compared with current findings on vaccine hesitancy and denial among HCP and may reveal how and why patterns in vaccine hesitancy and denial changed over the course of the pandemic.
We hypothesized that age gender, race, job role and socioeconomic status may predict likelihood of delaying or denying the vaccine as well as discordance between HCP vaccine intention and actual vaccine status.
Methodology
This retrospective study was conducted at Stanford Children’s Health (SCH, a 361-bed pediatric acute care hospital), Stanford Health Care Palo Alto (SHC, 613-bed adult acute care hospital in Stanford, CA), and Stanford Health Care-Valley Care (SVC, 207 bed adult acute care hospital in Livermore, CA).
An email invitation was sent to all HCP employed by SCH, SHC and SVC to complete a voluntary survey on their willingness to get the COVID-19 vaccine between December 11, 2020, and January 17, 2021. Survey responses were captured and integrated with the human resource record which contained job role, department, age, gender, race, ethnicity, county of residence, COVID-19 vaccine intention (accept, delay, decline), reasons for vaccine delay or decline, and whether HCP ultimately received at least one dose of any brand of COVID-19 vaccine. All surveys containing an answer to the question about intention to get vaccinated were included in the analysis.
HCP job roles were divided into three patient-care groups according to risk of SARS-CoV-2 exposure based on amount of patient contact inherent to the job role. Frequency of patient contact is a commonly cited explanatory variable for vaccine hesitancy [7-12]. The “High Risk” category included HCP with the most patient contact (nurse practitioners, nurses, patient transport, respiratory therapists, physician assistants, clinical support, medical trainees, housekeeping, physicians and clinical technicians), the “Moderate Risk” group included HCP with less patient contact (lab workers, dieticians, non-clinical support, pharmacy staff), and the “Low Risk” group included HCP with very little relative patient contact (administration, food service, information technology).
The Social Vulnerability Index (SVI), which is associated with the respondent’s county of residence, was used as a proxy for measuring socio-economic status among the participants in the study. The Center for Disease Control uses SVI to help identify communities that may need support before, during, or after disasters based on social factors including income level, access to vehicles, medical care, transportation, nutrition, and housing situation. The “low to moderate” vulnerability category including counties with an SVI range of 0.25-0.50 (e.g., San Francisco county), “moderate to high” vulnerability category including counties with an SVI range of 0.50- 0.75 (e.g., Sacramento county), and high vulnerability category included counties with an SVI range of 0.75-1.0 (e.g., Stanislaus county).
To test our hypothesis, the continuous and categorical variables were compared using parametric or nonparametric methods as appropriate. A chi-square test and Fisher’s exact test were applied to examine the association between vaccine intention subgroup and categorical variables, and two sample t-tests were used for continuous variables. All p-values were two-tailed and an alpha value of 0.05 was considered statistically significant.
Variable selection was performed using variables considered clinically significant based on the literature and selected a priori. In each univariate logistic regression, we checked for interaction between all candidate variables for the multivariate regression. If variables were found colinear based on correlation procedures, only the most clinically relevant variable was included in the multivariate regression. Linearity in the log it was met prior to running the multivariable regression.
For the multivariable analyses, we estimated the Odds Ratio (OR) using logistic regression given the outcomes of interest was binary. For Table 2, “Yes to vaccine”=1, “No to vaccine”=0. For Table 3, concordance with intention vs. actual vaccine status=1; discordance=0. The demographic characteristics of responders were compared with non-responders. The analysis was generated using SAS software (2022) SAS Institute Inc. (Cary, NC, USA).
Results
Of the 29,003 Stanford HCP who received the survey, 15,477 (53%) completed a survey that could be linked to an employee record; 10,097 (66%) of these respondents expressed intent to accept the COVID-19 vaccine, 4,421 (29%) expressed intent to delay the vaccine, and 959 (6%) expressed intent to deny the vaccine (Figure 1). Descriptive statistics of the responders are presented in Table 1 by COVID-19 vaccine intention subgroup: consented to the vaccine, delayed the vaccine, or declined the vaccine.
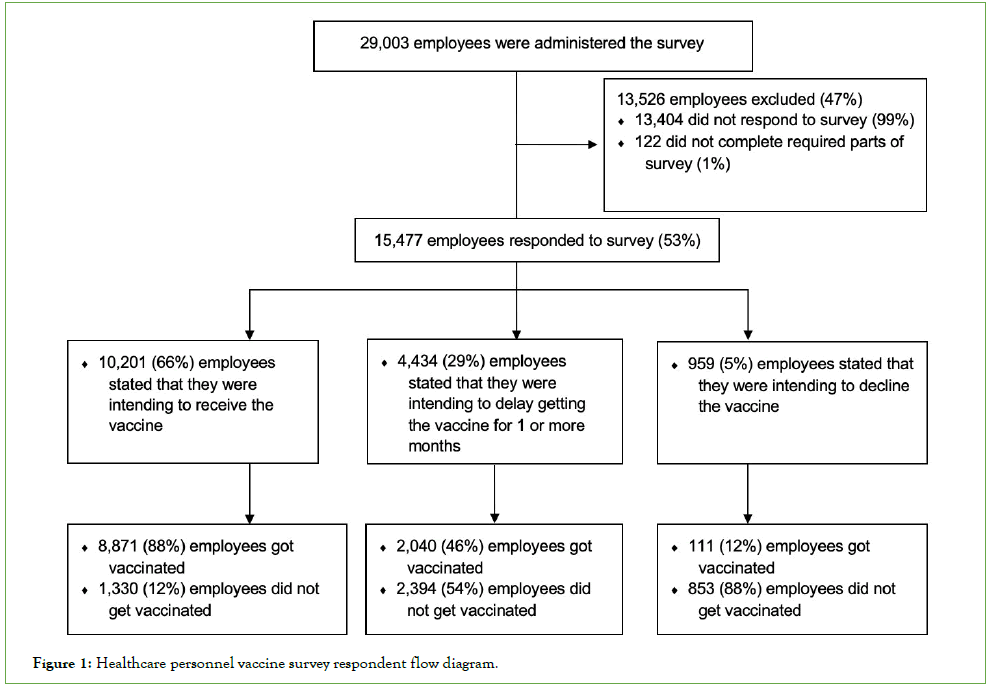
Figure 1: Healthcare personnel vaccine survey respondent flow diagram.
| Received Vaccine (n=10,097) | Delayed | Denied Vaccine (n=959) | ||||||
|---|---|---|---|---|---|---|---|---|
| Vaccine | All | |||||||
| (n=4,421) | (n=15,477) | |||||||
| Age (Mean) | 43 ± 11.5 | 41 ± 10.8 | 41 ± 11 | |||||
| N | % | N | % | N | % | N | ||
| Gender | Female | 6,688 | 63 | 3,240 | 31 | 674 | 6 | 10,602 |
| Male | 3,352 | 70 | 1,159 | 24 | 248 | 5 | 4,759 | |
| Race | Asian | 3,435 | 66 | 1,593 | 31 | 182 | 3 | 5,210 |
| White | 3,143 | 74 | 889 | 21 | 201 | 5 | 4,233 | |
| Two or more races | 278 | 61 | 131 | 29 | 46 | 10 | 455 | |
| Black or African American | 323 | 42 | 332 | 43 | 115 | 15 | 770 | |
| Native Hawaiian or Other Pacific Islander | 98 | 48 | 83 | 41 | 23 | 11 | 204 | |
| American Indian or Alaska Native | 15 | 50 | 13 | 43 | 2 | 7 | 30 | |
| Ethnicity | Hispanic / Latino | 856 | 52 | 647 | 39 | 146 | 9 | 1,649 |
| Non-Hispanic / Latino | 5,678 | 69 | 2,127 | 26 | 377 | 5 | 8,182 | |
| Social Vulnerability Index | ||||||||
| Low to Moderate | 8,146 | 68 | 3,281 | 27 | 575 | 5 | 12,002 | |
| Vulnerability | ||||||||
| Moderate to High Vulnerability | 200 | 71 | 66 | 23 | 17 | 6 | 283 | |
| High Vulnerability | 288 | 50 | 218 | 38 | 70 | 12 | 576 | |
| N/A | 297 | 66 | 110 | 25 | 40 | 9 | 447 | |
| Job Role by Risk of COVID-19 | High Risk | 5,647 | 71 | 1,896 | 24 | 417 | 5 | 7,960 |
| Moderate Risk | 494 | 59 | 283 | 34 | 61 | 7 | 838 | |
| Low Risk | 3,776 | 59 | 2,163 | 34 | 470 | 7 | 6,409 | |
| Other | 180 | 67 | 79 | 29 | 11 | 4 | 270 | |
Table 1: Demographic characteristics of survey respondents by vaccine intention.
As shown in Table 2, female HCP had 61% greater odds of consenting to the vaccine than male HCP (OR=1.61, C.I. 0.68- 3.77). Black or African American employees were 4.4 times more likely to decline the vaccine compared with their white colleagues (95% CI: 3.59-5.48). White and Asian HCP were the least likely to delay the vaccine of all race categories. Compared with healthcare workers in the “high risk” patient care group employees (OR: 1.71, 1.53-1.91), employees who worked as nurses, nurse practitioners, patient transporters, physician assistants, respiratory therapists, clinical support staff, in graduate medical education, or as medical staff. HCP from highly vulnerable counties according to the CDC’s SVI, had significantly higher odds of delaying or denying the vaccine (OR: 1.98, 1.36-2.88) compared with healthcare workers from counties categorized as low to moderately vulnerable by the CDC.
| Effect | Odds Ratio | 95% CI | ||
|---|---|---|---|---|
| Age (years) | 0.98* | 0.98 | 0.99 | |
Gender |
Female | 1.63* | 1.44 | 1.84 |
| Male | 1 | |||
| Race | American Indian or Alaska Native | 2.79* | 1.12 | 7 |
| Asian | 1.55* | 1.38 | 1.74 | |
| Black | 4.44* | 3.59 | 5.48 | |
| Native Hawaiian or Other Pacific Islander | 3.22* | 2.25 | 4.61 | |
| Two or More Races | 1.58* | 1.21 | 2.07 | |
| White | 1 | |||
| Ethnicity | Hispanic/Latino | 0.99 | 0.7 | 1.39 |
| Non-Hispanic / Non-Latino | 1 | |||
|
Patient Care Group |
Low Risk | 1.71* | 1.53 | 1.91 |
| Moderate Risk | 1.52* | 1.18 | 1.96 | |
| Other | 1.89* | 1.2 | 2.96 | |
| High Risk | 1 | |||
| Social Vulnerability Index | High Vulnerability | 2.02 | 1.58 | 2.58 |
| Moderate to High Vulnerability | 0.96 | 0.68 | 1.35 | |
| Other | 1.08 | 0.78 | 1.5 | |
| Low to Moderate Vulnerability | 1 | |||
Note: “Yes to vaccine”=1, “No to vaccine”=0; Point estimates with an * are statistically significant.
Table 2: Probability of delaying or denying the vaccine by demographic variable.
In Table 3, it is shown that black healthcare workers had 5.8 times higher odds (C.I. 4.3-7.7) of showing discordance between vaccination intention and actual vaccination status. This means that black HCP were at higher odds of changing their minds about getting vaccinated compared with white HCP. Since black HCP were more likely to state “vaccine delay/decline” as an original vaccination intention compared with white HCP, we assume that black HCP changed their minds from refusing the vaccine to accepting it by March, 2021. Furthermore, HCP in a “low risk” job role category were 1.9 times more likely (C.I. 1.552.21) to change their minds about getting vaccinated compared with the “high-risk” job role group. HCP from high vulnerability counties were also more likely to change their minds about vaccination compared with healthcare workers of low to moderate vulnerability counties (OR: 2.0, 1.4-2.9).
| Point Estimate | 95% CI | |||
|---|---|---|---|---|
| Age (years) | 1 | 0.82 | 2.23 | |
| Gender | Female | 1.13 | 0.72 | 1.05 |
| Male | 1 | |||
| Race | American Indian or Alaska Native | 1.75 | 0.37 | 8.2 |
| Asian | 1.17 | 0.97 | 1.4 | |
| Black or African American | 5.76* | 4.32 | 7.66 | |
| Native Hawaiian or Other Pacific Islander | 2.88* | 1.72 | 4.82 | |
| Two or more race | 1.12 | 0.66 | 1.92 | |
| White | 1 | |||
| Ethnicity | Hispanic/Latino | 0.68 | 0.38 | 1.25 |
| Non-Hispanic / Latino | 1 | |||
| Patient Care | Low Risk | 1.85* | 1.55 | 2.21 |
| Moderate Risk | 1.25* | 1.81 | 1.94 | |
| Other | 3.71* | 2.05 | 6.7 | |
| High Risk | 1 | |||
| Social Vulnerability Index | High Vulnerability | 1.98* | 1.36 | 2.88 |
| Moderate to High Vulnerability | 1.39 | 0.86 | 2.23 | |
| Other | 2.58* | 1.74 | 3.83 | |
| Low to Moderate Vulnerability | 1 | |||
Note: Concordance with intention vs actual vaccine status=1; discordance=0, Point estimates marked with and asterix (*) are statistically significant.
Table 3: Probability of vaccination status inconsistent with vaccination intention.
The demographic breakdown of responders was similar to non- responders in terms of sex (69% female, 31% male in both groups, p=0.99) and age (p=0.59) (Table 4). However, race, ethnicity, SVI, and job role category differed significantly. Asian HCP made up a greater proportion of responders (48%) than non-responders (41%). The greatest proportion of non-responders were white (48%) vs. non-responders (31%). Healthcare workers in a “high risk” job role made up a larger proportion of the non-responders than the responders, and healthcare workers in the “low risk” group made up a larger proportion of the responder than the non-responder categories (p<0.0001).
| Responders (N = 15,477) |
Non-Responders (N= 13,006) |
p-value | |||||
|---|---|---|---|---|---|---|---|
| Age (Mean) | 42 ± 11.37 | 42 ± 12.51 | 0.59 | ||||
| N | % | N | % | Total N | |||
| Gender | Female | 10,602 | 55 | 8,646 | 45 | 19,248 | 0.99 |
| Male | 4,759 | 55 | 3,882 | 45 | 8,641 | ||
| Race | Asian | 5,210 | 82 | 1,150 | 18 | 6,360 | <.0001 |
| White | 4,233 | 76 | 1,321 | 24 | 5,554 | ||
| Two or more races | 455 | 83 | 90 | 17 | 545 | ||
| Black or African American | 770 | 80 | 197 | 20 | 967 | ||
| Native Hawaiian or Other Pacific Islander | 204 | 85 | 35 | 15 | 239 | ||
| American Indian or Alaska Native | 30 | 75 | 10 | 25 | 40 | ||
| Ethnicity | Hispanic / Latino | 1,649 | 57 | 1,220 | 43 | 2,869 | 0.0044 |
| Non-Hispanic / Latino | 8,182 | 55 | 6,807 | 45 | 14,989 | ||
| Social Vulnerability Index | Low to Moderate Vulnerability | 12,002 | 55 | 9,905 | 45 | 21,907 | <.0001 |
| Moderate to High Vulnerability | 283 | 54 | 244 | 46 | 527 | ||
| High Vulnerability | 576 | 72 | 229 | 28 | 805 | ||
| N/A | 447 | 46 | 533 | 54 | 980 | ||
| Job Role by Risk of COVID-19 | High Risk | 7,960 | 50 | 7,964 | 50 | 15,924 | <.0001 |
| Moderate Risk | 838 | 58 | 618 | 42 | 1,456 | ||
| Low Risk | 6,409 | 71 | 2,625 | 29 | 6,409 | ||
| Other | 270 | 57 | 204 | 43 | 270 | ||
Table 4: Demographic characteristics of survey responders vs. non-responders.
Limitations
This survey was administered to individuals who work in California Bay Area healthcare facilities, and these results may not be generalizable to another geographical context because of differences in demographic composition. Furthermore, the questionnaire only asked about sex and not gender, which limits conclusions we can draw on how different gender identities may affect vaccination intention. Finally, as seen by the statistically significant p-values (<0.05) in Table 1 demonstrating demographic differences in the make-up of the responder and non-responder groups, responder bias was present in our analysis, which limits the generalizability of our results. In future analyses, adjustment for responder bias and intentional efforts to ensure a representative sample of survey respondents would strengthen the study.
Discussion and Conclusion
We examined HCP vaccination intention before COVID-19 vaccines became widely administered among healthcare workers. Our findings were similar to those reported in the literature with 65% of responders intending to receive the vaccine. HCP most likely to delay or decline the vaccine in this study were Black/ African American, in low-risk job roles, and from high vulnerability counties. These results confirm existing literature that shows that the prevalence of COVID-19 vaccine hesitancy is highest among Black/African Americans and in individuals with lower household income. It has been shown that racial discrimination is a predictor of vaccine hesitancy, which may explain the higher level of hesitancy among racial minority groups and demonstrates that vaccination campaigns should be sensitive to individuals’ past experiences of racial discrimination.
Additionally, our results demonstrated that healthcare personnel who do not interface directly with patients are at higher risk for vaccine hesitancy, confirming existing literature on the topic. This may be a result of higher education among healthcare personnel with more patient-facing responsibilities, or higher perceived risk of contracting COVID-19 in patient-facing job roles.
Interestingly, the population characteristics of the employees in our analysis who changed their minds from their original vaccination intention were similar to the population characteristics of those who originally delayed or denied the vaccine. Between January 31st and March 7th 2022, Asian, Hispanic, and Black participants had larger increases in vaccination rates compared to white people, confirming that people from demographic groups that are more highly associated with vaccine hesitancy are open to changing their minds with time; more widespread and targeted vaccine messaging likely contributes to this trend. This suggests that vaccination campaigns need to be more thoughtfully tailored to communities of color early in public health crises.
It is essential to understand vaccination patterns and address disparities in vaccine uptake because low vaccination rates are not only a risk to the individual and community but affect the likelihood of another spike in COVID-19 cases and the emergence of another novel variant. Furthermore, because healthcare workers play an important role in advising patients and communities, it is critical that their vaccination rates be high because of their positions as societal role-models. Future vaccination campaigns in hospitals should consider the HCP populations with a high probability of avoiding vaccination and design vaccine messaging that is specific to these groups.
Implications for Health Promotion
Future vaccination campaigns in hospitals should consider the HCP populations with a high probability of avoiding vaccination and design vaccine messaging that is specific to these groups.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. All authors attest they meet the ICMJE criteria for authorship.
References
- How many health care workers are unvaccinated? Here’s why it’s so hard to say. Advisory Board. 2022.
- Morales DX, Beltran TF, Morales SA. Gender, socioeconomic status, and COVID‐19 vaccine hesitancy in the US: an intersectionality approach. Sociol Health Illn. 2022;44(6):953-971.
[Crossref] [Google Scholar] [PubMed]
- Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9(2):119.
[Crossref] [Google Scholar] [PubMed]
- Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, et al. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med. 2021;272:113638..
[Crossref] [Google Scholar] [PubMed]
- Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775-779.
[Crossref] [Google Scholar] [PubMed]
- Kricorian K, Civen R, Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother. 2022;18(1):1950504..
[Crossref] [Google Scholar] [PubMed]
- Paris C, Bénézit F, Geslin M, Polard E, Baldeyrou M, Turmel V, et al. COVID-19 vaccine hesitancy among healthcare workers. Infect Dis Now. 2021;51(5):484-487.
- Kose S, Mandiracioglu A, Sahin S, Kaynar T, Karbus O, Ozbel Y. Vaccine hesitancy of the COVID‐19 by health care personnel. Int J Clin Pract. 2021;75(5):e13917.
- Kwok KO, Li KK, Wei WI, Tang A, Wong SY, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114:103854.
- Willis DE, Andersen JA, Bryant‐Moore K, Selig JP, Long CR, Felix HC, et al. COVID‐19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin Transl Sci. 2021;14(6):2200-2207.
[Crossref] [Google Scholar] [PubMed]
- Savoia E, Piltch-Loeb R, Goldberg B, Miller-Idriss C, Hughes B, Montrond A, et al. Predictors of COVID-19 vaccine hesitancy: socio-demographics, co-morbidity, and past experience of racial discrimination. Vaccines. 2021;9(7):767.
[Crossref] [Google Scholar] [PubMed]
- Ndugga N, Hill L, Artiga S, Haldar S. Latest data on COVID-19 vaccinations by race/ethnicity. Kais Family Found. 2021.
Citation: Bellon M, Shepard J, Wei J, Salinas JL, Sarnquist C, Khan S, et al (2023) COVID-19 Vaccine Hesitancy and Subsequent Uptake among Healthcare Personnel at an Academic Medical Centre in California, 2021 . J Vaccines Vaccin. 14:512.
Copyright: © 2023 Bellon M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

