Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 2
Covid-19 in the elderly: Insight into Symptomatology.
Ayad Rasheed1, Anmar Alharganee2* and Laith Kamel1,32Department of Oncology, Nottingham University Hospital/QMC, Baghdad Medical City Complex, Iraq
Bournville and Northfield PCN, Birmingham, UK
Received: 02-Jan-2021 Published: 24-Jan-2021, DOI: 10.35248/2329-891X.2021.9.272
Abstract
Introduction: Ever since the end of 2019, the SARS-Cov2 virus started to emerge in Wuhan/ China and theories suggested a possible zoonotic transmission to human beings. Older people were considered to be the most afflicted by Covid-19 pandemic worldwide. Serious measures had been taken to mitigate the contagiousness of this virus especially in this age group, most of whom, presented with atypical symptoms.
Methods: In this study we retrospectively studied the symptomatology of the disease in 79 subjects within the same care-home within a three-month period, (March-June 2020).
Results: Within the total number of participants we were able to confirm the diagnosis of Covid-19 in 40 patients. Symptoms were mainly cough, shortness of breath and fatigue. Surprisingly, the rise in temperature was only a presenting symptom in few patients. However, many patients presented with tiredness, myalgia and worsening confusion as well as cough, which were the main presenting symptoms in the cohort.
Conclusion and recommendations: Research is still trying to figure out the variation of symptoms between age groups especially the low temperature rates in the geriatric age groups. This could be explained by the dormancy of interleukins in older patients due to the physiological process of ageing. Mortality rates were predictably high secondary to the plethora of comorbidities in older patients. It is empirical for health care professionals to consider the non- classical presenting symptoms of Covid-19 in elderlies. More public health awareness is needed to help patients, relatives and carers to recognize the disease early, despite the lack of typical symptoms.
Keywords
SARS CoV-2; COVID-19; Infection; Symptomatology
Introduction
COVID-19 is a respiratory illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2). The novel CoronavirusDisease2019 (COVID-19) first emerged as an outbreak in the province of Hubei, China, in December 2019, which is thought to have originated from an animal host with eventual spread to humans. Since then the virus spread all over the world. The World Health Organisation (WHO) declared the outbreak as a pandemic on March 11, 2020 [1]. COVID-19 became a global pandemic in a matter of months, affecting over 100 countries and totaling 824,559 infections and 40,673 deaths worldwide as of March 31, 2020 [2].
Coronaviruses constitute a large family of viruses known to infect both humans and animals. Bats have been implicated as vectors in the largest variety of coronaviruses. The human coronaviruses can be sub classified into alpha and beta coronaviruses.
Clinical manifestations of coronavirus infections are typically respiratory and enteric, although some present with neurologic manifestations. COVID-19 is thought to have an incubation period of approximately 2 weeks, with most infected individuals becoming symptomatic 5 days after exposure. Illness severity ranges from mild to critical and fatal. Approximately 80% of cases are asymptomatic or have mild symptoms, 15% have severe illness, and 5% have critical illness. Due to testing availability and limitations, the true case fatality rate (CFR) with COVID-19 is difficult to determine, but it is believed to range from 1–3% based on existing data from different countries [3].
Since the beginning of the pandemic, we are still learning about the virus and our knowledge is still developing. There are several studies with new findings emerging almost on daily basis. The general understanding that has been promoted by public health organisations across the globe is that COVID-19 presents with persistent fever, dyspnoea and dry cough [4]. Later on, loss of smell and taste sensation was add to the presenting symptoms. Unfortunately, this was not entirely accurate and at times, potentially misleading in the elderly age groups. Those main presenting symptoms were quite often absent or less prominent in that group.
The disease progresses from asymptomatic incubation period to mild presenting symptoms in the first few days with the possibility of developing more serious symptoms related to Pneumonia or ARDS (Acute Respiratory Distress Syndrome) from day 7 onward. Those with only mild symptoms are likely to recover within 1-2 weeks [5].
Methodology
The study followed up 79 residents of a single care home during a three-month period, between March-June 2020. It collected data retrospectively from the care home patients who had positive COVID-19 swabs. The data included patients’ age, sex, ethnicity, comorbidities, presenting symptoms, hospitalisation episodes and outcomes. Then presenting symptoms and final outcome were analysed. Patients’ anonymity was preserved throughout.
Results
The results derived from 40 patients who were positive for COVID-19 at some point during the study period. The classical symptoms of Cough, Shortness of Breath (SOB) and persistent high temp were only present in 4 patients (10%) only, while 6 patients (15%) were completely asymptomatic. Another interesting finding was that no one in the study reported loss of taste or smell sensation (Table 1).
| Demographics | Number of patients | Deaths | |
|---|---|---|---|
| (MR) | |||
| Age group | 61-70 | 1 | 0 |
| 71-80 | 4 | 0 | |
| 81-90 | 24 | 8 (33%) | |
| 91-100 | 10 | 6 (60%) | |
| 101-110 | 1 | 0 | |
| Gender | Male | 14 (35% | 4 (28%) |
| Female | 26 (65%) | 10 (38%) | |
| Comorbidities | <3 | 6 | 1 |
| >3 | 34 | 13 | |
Table 1: Patients' demographics.
Only 50% of the patients developed cough, 42% had SOB and 27% had high temperature. On the other hand, fatigue and myalgia were as common as cough, in 50% of the patients, and 32% had worsening confusion. Loss of appetite and reduced oral intake were also reported in several patients (Table 2).
| Cough | Temp | SOB | Confusion | GI | Fatigue & | |
|---|---|---|---|---|---|---|
| symptoms | Myalgia | |||||
| Yes (%) | 20 (50%) | 11 (27%) | 17 (42%) | 13 (32%) | 5 (12%) | 20 (50%) |
| No (%) | 20 (50%) | 29 (73%) | 23 (58%) | 27 (68%) | 35 (88%) | 20 (50%) |
Table 2: Socio-demographic characteristics of adult HIV patients attended Dessie town ART clinics, 2018.
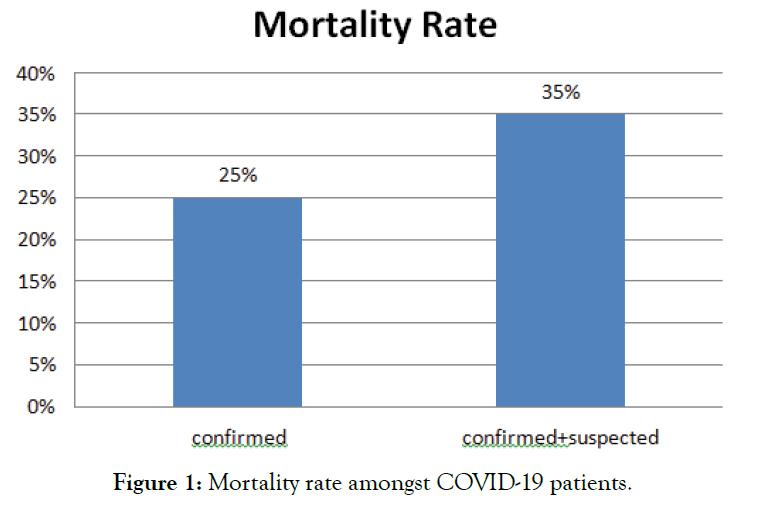
Mortality Rate (MR) was higher than the COVID-19 general population mortality rate (Figure 1).
Figure 1: Mortality rate amongst COVID-19 patients.
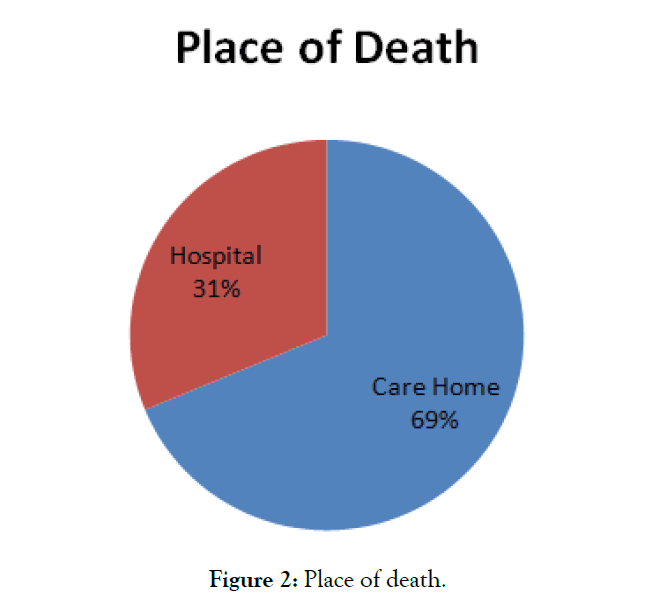
It was 25% for confirmed COVID-19 cases. This was attributed to the extreme age group in our cohort. 35 patients (88%) were aged above 80 years old. Moreover, most of the cohort suffered from significant multiple comorbidities that are usually associated with this age group (Figure 2).
Figure 2: Place of death.
Discussion
Following the pandemic, the whole health system across the globe went through drastic remodeling. Health care systems and professionals categorically agreed on shifting towards remote consulting using phone and video calls or other methods of contact.
Health care systems were entirely reliant on the available guidelines and screening tools, which clearly highlighted the triad of fever, cough and SOB as the main presenting symptoms and also as the main indicators for disease severity, to decide on further management. Later on anosmia was added to that triad [6].
The general consensus, from the beginning of the pandemic, was that elderly patients were at much higher risk to get the infection and to get more severe illness with more serious outcomes. Observations from the CDC asserted that adults aged above 65 may develop atypical symptoms. Immobility and delirium were the main observed symptoms within nursing and care home facilities. Body temperature might be lower than expected in younger adults. Those findings can be explained by the lack of response of endogenous cytokines to infections due to the physiological process of aging [7-9].
The elderly population also differs in their disease progression. Mild or non-specific symptoms could take a longer course and could go either way at any time. Lower threshold is required to be able to diagnose the disease, manage and predict its progression pattern [10,11].
Conclusions
This pandemic has witnessed massive increase in health budgets all over the world. Big part of that expenditure was on health promotion campaigns to raise public awareness of the virus, how to prevent it and how to recognize its symptoms. However, there was no clear message to promote early recognition of COVID-19 illness in the elderly. Older patients, their families and carers failed to recognize the non-classical symptoms. If anything they may have been misled by the health promotion campaigns which caused false reassurance and delayed seeking medical help.
Moreover, this could have created a diagnostic hurdle to health care professionals dealing with those patients. Finally, COVID-19 testing was, and still is in many countries, limited to patients showing classical symptoms, therefore elderly patients with increased tiredness, or worsening confusion would unlikely be offered the test.
It is imperative that all clinicians need to raise the level of awareness about atypical Covid-19 symptoms in the elderly as recommended by the British Society of Geriatrics. They should consider early testing and early escalation, especially for those with coexisting comorbidities. The early detection of geriatric Covid carriers will improve their clinical outcome and also decrease the figures of community transmission through their care givers.
Ethical Approval
Not applicable.
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- World Health Organization. Coronavirus Disease (COVID-19)-Events As They Happen. Geneva. 2020.
- McIntosh K. Coronaviruses. Up To Date. 2020;20:851-859.
- Yeoh CB, Lee KJ, Reith EF, Mapes R, Fischer GW, Tollinche LE. COVID-19 in the cancer patient. Anesthesia Analgesia. 2020;131:16-23.
- Trisha G, Choon-Huat KG, Josip C. Covid-19: A remote assessment in primary care pediatric blood cancer. BMJ. 2020;368:m1182.
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). 2020.
- https://www.bmj.com/content/bmj/suppl/2020/03/24/bmj.m1182.DC1/gret055914.fi.pdf
- Norman D. Fever in the Elderly. Clin Infect Dis. 2000;31:148-151.
- Jung YJ, Yoon JL, Kim HS, Lee AY, Kim MY, Cho JJ. Atypical clinical presentation of geriatric syndrome in elderly patients with pneumonia or coronary artery disease. Ann Geri Med Res. 2017;21:158-163.
- Holroyd-Leduc J, Gandell D, Miller A, Petrov D. COVID-19 in older adults. Reg Geri Toronto. 2020;20:1-9.
- D'Adamo H, Yoshikawa T, Ouslander J. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J Am Ger Soc. 2020;68:912-917.
- Solanki T. Atypical Covid-19 presentations in older people-The need for continued vigilance. Brit Ger Soc. 2020.
Citation: Rasheed A, Alharganee A, Kamel L (2021) Covid-19 in the elderly: Insight into Symptomatology. J Trop Dis 9:272. doi: 10.35248/2329-891X.2021.9.272
Copyright: 2021 Rasheed A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.