Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 0, Issue 0
Cor Triatriatum Sinister Combined with Dilated Cardiomyopathy
Mei-lian Cai1,2 and Guo-qiang Zhong2*2Department of Cardiology, The First Affiliated Hospital of Guangxi Medical University, Nanning City, China
Received: 12-Dec-2022, Manuscript No. JCRB-22-19184; Editor assigned: 14-Dec-2022, Pre QC No. JCRB-22-19184 (PQ); Reviewed: 30-Dec-2022, QC No. JCRB-22-19184; Revised: 06-Jan-2023, Manuscript No. JCRB-22-19184 (R); Published: 13-Jan-2023, DOI: 10.35248/2155-9627.22.S12.001
Abstract
Background: Cor Triatriatum Sinister (CTS) is a relatively rare congenital heart disease, and a membrane divides the Left Atrium (LA) into two cavities that communicate through a small opening. It is often associated with other congenital cardiac anomalies; however, it associated with other cardiomyopathy has not been reported.
Patients and method: A 33-year-old female presented with fatigability, facial surface and double lower limb edema for more than 1 week. The patient underwent Electrocardiogram (ECG), Transthoracic Echocardiography (TTE) and cardiac Magnetic Resonance Imaging (MRI), which showed the presence of a membrane in LA, indicated cor triatriatum (complete type), smooth blood flow at the traffic port, and no obvious obstruction to the blood flow. She was diagnosed with Atrial Fibrillation (AF), CTS with Dilated Cardiomyopathy (DCM).
Results: The patient received medical treatments for heart failure. After that, she was treated with AF radiofrequency ablation. After discharge, the clinical manifestation of fatigability, facial surface and double lower limb edema did not recur.
Conclusion: The symptoms of patients with cor triatriatum associated with other heart disease may not be caused by cor triatriatum. We must pay attention to identification.
Keywords
Cor Triatriatum; Cor Triatriatum sinister; Membrane; Congenital cardiovascular anomalies; Dilated cardiomyopathy
Abbreviations
AF: Atrial Fibrillation; ASD: Atrial Septal Defect; CPVA: Common Pulmonary Venous Atresia; CT: Computed Tomography; CTD: Cor Triatriatum Dexter; CTS: Cor Triatriatum Sinister; DCM: Dilated Cardiomyopathy; ECG: Electrocardiogram; EF: Ejection Fraction; LA: Left Atrium; LV: Left Ventricle; MDCT: Multidetector Computed Tomography; MI: Mitral Insufficiency; MRI: Magnetic Resonance Imaging; NYHA: New York Heart Association; PAPVR/TAPVR: Partial or Total Anomalous Pulmonary Venous Return; PAH: Pulmonary Arterial Hypertension; PVs: Pulmonary Veins; TAPVC: Total Anomalous Pulmonary Venous Connection; TEE: Transesophageal Echocardiography; TTE: Transthoracic Echocardiography; IVC: Inferior Vena Cava
Introduction
Cor triatriatum or triatrial heart is a rare anomaly that can either involves the Left Atrium (LA) (Cor Triatriatum Sinister-CTS) or the right atrium (Cor Triatriatum Dexter-CTD). It is characterised by the presence of an abnormal intra-atrial membrane that divides atrium into two chambers [1]. CTS and CTD represent respectively only 0.1%, and 0.025% of all congenital cardiac anomalies [2,3]. It is slightly more common among men than women, with men: women ratio of 1.5:1 [4]. The degree of restriction dictates the age of presentation and the severity of symptoms [5]. Restrictive membrane may result in pulmonary venous hypertension progressing to congestive heart failure. It is very important to diagnose early.
Case Presentation
A 33-year-old female presented with fatigability, facial surface and double lower limb edema for more than 1 week on March 11, 2022. The Electrocardiogram (ECG) and 72 hour dynamic ECG showed rapid Atrial Fibrillation (AF) rhythm, ST segment and the T wave changed, and the V2 lead R wave rises poorly. Transthoracic Echocardiography (TTE) showed a membrane in the LA strong echo across the LA connecting the left atrium lateral wall and the atrial septum. There was a very small fenestration (internal diameter about 13 × 8 mm) in the membrane with velocity of blood flow 0.8 m/second, gradient of 3 mmHg. Accessory atrial chamber receives all Pulmonary Veins (PVs). The LA was divided into the posterior-superior chamber (the transverse diameter 40.8 mm, long diameter 33.0 mm) and the anterior-inferior chamber (the transverse diameter 40.3 mm, long diameter 27.5 mm). TTE results demonstrated: 1. The enlargement of the LA and the Left Verticle (LV) + the overall systollic function of the LV wall significantly weakened (Ejection Fraction (EF) 24.9%) + the excessive local trabecular bulge of the LV muscle, forming crypts (please combine with clinical). 2. The presence of a membrane in LA indicated cor triatriatum (type ⅠA), smooth blood flow at the traffic port, and no obvious obstruction to the blood flow. 3. Mild Mitral Insufficiency (MI). 4. Trace amount of hydropericardium. 5. LV diastolic function limited. Cardiac Magnetic Resonance Imaging (MRI) flat scan + myocardial perfusion dynamic enhancement scan revealed: 1. LV enlargement, consistent with Dilated Cardiomyopathy (DCM); 2. Triatrial heart; 3. Noncompation of partial myocardium of the lower wall of the LV apical segment?N-ProBNP showed 5782.5 pg/ml. Diagnosis: 1. Dilated cardiomyopathy (DCM), LA and LV enlargement, mild MI, New York Heart Association (NYHA) class Ⅱ 2.Congenital heart disease: CTS (type ⅠA), left ventricle crypts. 3.Cardiac arrhythmia: persistent AF. The patient received the treatment according to heart failure and AF. The patient improved and was discharged on March 16, 2022. Thereafter, she received Levosimendan intravenous drip once a month to October (Figure 1).
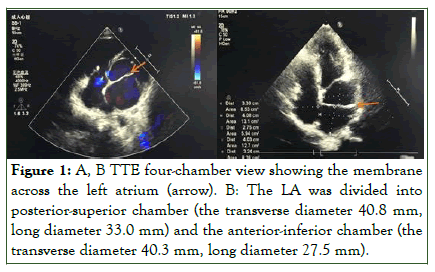
Figure 1: A, B TTE four-chamber view showing the membrane across the left atrium (arrow). B: The LA was divided into posterior-superior chamber (the transverse diameter 40.8 mm, long diameter 33.0 mm) and the anterior-inferior chamber (the transverse diameter 40.3 mm, long diameter 27.5 mm).
The patient was hospitalized in our department on June 20 once more and treated with AF radiofrequency ablation on June 26. The operation went well. Re-examination of the ECG in October indicated that it was sinus rhythm without ST segment and the T wave changed. Re-examination of the TTE indicated that 1.The LV was slightly larger. 2. Three rooms of the left room (complete type). 3. Systolic function of the LV normal (EF 64.9%). N-ProBNP showed normal (66.00 pg/ml). The patient was treated with metoprolol succinate sustained release tablets (47.5 mg, qd), sacubitril valsartan sodium tablets (50 mg, bid), dapagliflozin tablets (10 mg, qd), spironolactone tablets (20 mg, qd). She was taking her medicine regularly. She remained asymptomatic. The patient receives regular outpaitient visits (Figure 2).

Figure 2: A: TTE short-axis view showing LVIDd 59.5 mm, LVIDs 52.6 mm, EF24.9% before treatment (in March). B: TTE four-chamber view showing LVIDd 53.0 mm, LVIDs 34.0 mm, EF 64.9% after treatment (in October).
Results and Discussion
This case was categorized as type ⅠA according to Lucas. Her clinical symptoms were caused by heart failure of DCM. After the correction of heart failure, the patient's EF got normal, LA got normal in size, and LV was obviously improved in size. In this case, CTS combined with DCM is a rare heart disease not previously reported in the literature.
It was the first described that the atrial chamber was divided by an accessory membrane by Church in 1868 [6]. Van Praagh, et al. research on the genetics of the cor triatriatum proposed the hypotheses that cor triatriatum results from entrapment of the left atrial ostium of the common PV by tissue of the right horn of the sinus venosus from which septum primum develops, leading to failure of incorporation of the common PV the LA during the fifth embryonic week [7]. The clinical presentation depends on the degree of obstruction caused by the membrane [8]. The asymptomatic patients were usually found by Health Check-up or some complications such as cerebral infarction or AF.
Cor triatriatum is a rare congenital heart defect in which the left or rarely the right atrium is subdivided into 2 atrial chambers by a tissue membrane [9]. Approximately 83% of patients with cor triatriatum had CTS and 17% had CTD [10,11]. It occurs in 0.1% of children with congenital heart disease. It is male to female ratio of 1:1, and it is commonly associated with other cardiovascular malformations (up to 84% in some series), however, Kim, et al. described a case of acquired cor triatriatum following surgical repair of coronary sinus type of Total Anomalous Pulmonary Venous Connection (TAPVC), which presented 11 years after initial repair of TAPVC [12]. If the obstruction at the level of the membrane is significant, the consequent pulmonary venous obstruction results in pulmonary hypertension and cardiac failure [13]. In the severe form of this condition, patients can present with pulmonary edema, Pulmonary Arterial Hypertension (PAH), respiratory failure, and cardiogenic shock [14-16]. CTS is frequently encountered with other congenital cardiovascular anomalies [17], such as Atrial Septal Defect (ASD), patent left superior caval vein [18], biventricular heart disease, and hypoplastic left heart syndrome [19-21]. It is most frequently associated with ASD [22]. Partial or Total Anomalous Pulmonary Venous Return (PAPVR/TAPVR) is reported as a coexisting disease in 10%-33% of patients with CTS [23].
Common presentations of children include failure to thrive, dyspnoea, cyanosis, or even shock [24]. The most common presenting symptoms of adult are dyspnea, hemoptysis, orthopnea, and chest pain [25]. Patients with isolated CTS and small membrane orifice often present clinically with features similar to mitral stenosis, dyspnoea on exertion, haemoptysis and sometimes arrhythmias and stroke [26]. There are some case reports of adult cor triatriatum presenting as embolic stroke or arterial embolism. Park, et al. described an unusual case of CTS in a 55-year-old woman in asymptomatic who presented with cardio embolic stroke [27]. However, the role of the membrane in thrombosis is controversial, previous study reported that 13% of patients with a cryptogenic stroke had large (>15 mm) membrane [28-34]. Cor triatriatum may be asymptomatic but may also be associated with an increased risk of AF and LA clots [35].
In CTD, persistence of the right valve of sinus venosus which divides the right atrium into two chambers, producing flow obstruction [36]. Most severe cases present with right heart failure, tricuspid valve obstruction with elevated central venous pressure, or a picture of suprahepatic portal hypertension (Budd-Chiari syndrome) due to Inferior Vena Cava (IVC) obstruction [37].
The earlier classification of cor triatriatum was suggested by Loeffler [38] (Table 1). After that, cor triatiatum may be classified into 4 groups, designated as Type I, Type Ⅱ, Type Ⅲ and Type IV [39]. There is a chamber behind and above the LA of Type I and Type Ⅱ. Type I is the first commonest triatrial heart that is one in which all 4 PVs empty into a chamber behind and above the LA. Type Ⅱ is the second commonest triatrial heart that is one in which all the PVs empty into the coronary sinus [39]. Type Ⅲ includes those hearts in which the right supraventricular chamber is divided into two compartments [40-41]. Type Ⅲ is known as CTD. Type IV is included aneurysms of the atria and interatrial septum, and atrial diverticula [42]. At present, some scholars used the modified classification of Lucas for the morphologic classification of cor triatiatum including CTS and CTD [43]. (Table 2). CTS are classified into types A, B and C according to the morphologic classification of Lam et al. [44] (Table 3).
| Class | Description |
|---|---|
| Type 1 | Complete septation, absence of communication between the proximal and the distal chambers, proximal chamber might connect with right atrium or anomalous drainage of the pulmonary vein |
| Type 2 | One or more openings in the septum |
| Type 3 | Proximal chamber communicates widely with the distal chamber |
Table 1: Classification of cor triatriatum according to Loeffler.
| Ⅰ. Accessory atrial chamber receives all pulmonary veins and communicates with the left atrium |
| A. No other connections (classic cor triatriatum) |
| B. Other anomalous connections |
| 1. To the right atrium directly |
| 2. With totally anomalous pulmonary venous connection |
| II. Accessory atrial chamber receives all pulmonary veins and does not communicate with the left atrium |
| A. Anomalous connection to the right atrium directly (cardiac totally anomalous pulmonary venous connection with all pulmonary veins first draining to a venous confluence) |
| B. With totally anomalous pulmonary venous connection (supracardiac or infracardiac totally anomalous pulmonary venous connection) |
| III. Subtotal cor triatriatum |
| A. Accessory atrial chamber receives part of the pulmonary veins and connects to the left atrium |
| 1. Remaining pulmonary veins connect normally |
| 2. Remaining pulmonary veins connect anomalously (partial cor triatriatum with partially anomalous pulmonary venous connection) |
| B. Accessory atrial chamber receives part of the pulmonary veins and connects to the right atrium |
| 1. Remaining pulmonary veins connect normally (partially anomalous pulmonary venous connection with anomalously connected pulmonary veins first draining to a venous confluence) |
| 2. Remaining pulmonary veins connect anomalously (mixed totally anomalous pulmonary venous connection) |
Table 2: Classification of cor triatriatum according to Lucas.
| Class | Description |
|---|---|
| A | Proximal chamber receives all the pulmonary veins; distal chamber contains the left atrial appendage and the mitral valve; There is no atrial septal defect |
| A1 | Atrial septal defect between right atrium and proximal chamber |
| A2 | Atrial septal defect between right atrium and distal chamber |
| B | Pulmonary veins drain into the coronary sinus |
| C | No anatomic connection between the pulmonary |
Table 3: Classification of cor triatriatum according to Lam.
Several techniques have been used to establish the diagnosis, such as TTE, Transesophageal Echocardiography (TEE), catheter angiography, Computed Tomography (CT) and MRI. TTE is the most commonly used method to found cor triatriatum. TEE is frequently needed to precisely define the anatomy of the membrane, and the degree of obstruction caused by this structure [46]. Levin et al. found three-dimensional TEE imaging clearly demonstrated the obliquely oriented membrane, which revealed that the membrane divided the atria into a medial funnel and C-shaped cavity with a large distaloval shape opening and an even larger lateral atrial cavity [47]. However, Seth et al. described that a patient was diagnosed with mitral supravalvular ring on TEE [5]. After cardiac Multidetector Computed Tomography (MDCT) examination, in fact, it was the membrane located proximal to the atrial appendage unlike what is found in supravalvular ring. Yokoyama et al. reported that a 5- hour-old female baby with the rare occasion of cor triatriatum co-existing with Common Pulmonary Venous Atresia (CPVA). CT eventually illustrated residual cor triatriatum [48]. The cardiac MDCT can provides a comprehensive anatomic evaluation of cor triatriatum, and can help the clinician to see a distinct septum in the LA, to evaluate the size and number of fenestrations, and to identify associated congenital cardiovascular anomalies. As the same time, it is more useful for recognising the detailed structure of cor triatriatum and underlying disease in complex heart disease patients [49]. MRI is a no radiation examination. MRI can even more clearly depict the precise morphology of cor triatriatum, demonstrating the relationship between the fibromuscular membrane and the PVs, determining the hemodynamic significance of the obstruction and detecting associated cardiac abnormalities [50]. Cardiac MRI is the gold standard for assessment of ventricular volumes. Hence, diagnosis of the membrane in the RA or LA was imaged using contrast cardiac MRI or MDCT.
Currently, Management includes conservative treatment, percutaneous balloon dilatatio and surgical therapy. But there are no guidelines or recommendations regarding which of the anatomical variations of cor triatriatu are appropriate for percutaneous or surgical treatment. Conservative approach is often implemented in asymptomatic adults [51]. Patient should be followed up for long-term. The case received conservative treatment with larger internal diameter of the membrane orifice without flow obstruction or other cardiac abnormalities. If intervention is warranted, several techniques have been described, including trans catheter disruption of the membrane and surgical resection via a transatrial approach [52].
Percutaneous balloon dilatation of cor triatriatum has also been reported. The first successfully implement percutaneous balloon dilatation of CTS by Kerkar in 1996 [53]. It seems that percutaneous balloon dilatation is a more reasonable treatment modality for type IA and type IIIA1 cor triatriatum. Hasnie, et al reported a case of CTD (type IB1) that resulted in right to left shunting across an ASD and symptomatic hypoxia that was successfully treated with transcatheter balloon angioplasty and percutaneous ASD closure [54]. Percutaneous balloon dilatation can be sued as a bridge for critical patient to elective defifinitive surgery [55]. Tuan, et al. followed up a female patient with CTS receiving percutaneous balloon dilatation for 18 years, and she was asymptomatic in serial cardiopulmonary exercise testing [56]. They believed percutaneous catheter-based balloon dilatation of obstructive membrane for classic CTS without other associated congenital heart diseases was considered sound and feasible. So far, there are 8 reports of successful percutaneous balloon dilatation of cor triatriatum. Four of the patients were children and three were young adults. Only one patient was a middle-aged woman. If membrane calcification is serious, especially around the membrane orifice, it is difficult to achieve the desired effect by percutaneous balloon dilatation to expand the membrane orifice, so surgical treatment is recommemded. If orifice diameter of the membrane is too small, and it can’t sufficient drain pulmonary venous even after percutaneous balloon dilatation, so surgical treatment is also recommemded.
Surgical repair is the definitive modality of treatment for symptomatic patients or associated with congenital heart defects, containing resection of the membrane and correction of the associated congenital heart defects [57-60].
Surgical intervention of cor triatriatum is usually a simple and straightforward procedure. It can be performed safely and effectively with an extremely low risk of recurrence, minimal mortality and morbidity [61]. Lewis et al. performed the first surgical approach in 1956 [62]. The first successful surgical repair of CTS associated with left PAPVR was reported in 1977 by Jennings et al. [63]. Soni, et al. presented the successfully managed cases of two children aged 11 months and three years with homozygous SS, and who underwent cardiopulmonary bypass for double-outlet right ventricle and cor-triatriatum sinistrum, respectively. The latter was also associated with ASD, severe tricuspid valve regurgitation, moderate right ventricle dysfunction, and severe PAH [63]. The study of Nagao et al. had shown that surgical correction offers good early and mid-term outcomes for both cor triatriatum with biventricular and univentricular physiologies [17].
Conclusion
It is rare that cor triatriatum malformation is associated with DCM. The symptoms of patients may be caused by DCM or other heart diseases, not by cor triatriatum. It is crucial important to choose the optimal treatment to patient’s specific condition.
Declarations
Follow-up and outcomes
At approximately the 9-month follow-up, the patient stated that she took the medicine regularly and she was asymptomatic.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
References
- Goel A, Viswamitra S, Reddy BN, Gaduputi J. Computed tomography features of cor triatriatum: An institutional review. Br J Radiol. 2021;94(1119):20201252.
[Crossref] [Google Scholar] [PubMed]
- Wolf WJ. Diagnostic features and pitfalls in the two-dimensional echocardiographic evaluation of a child with cor triatriatum. Pediatr Cardiol. 1986;6(4):211-213.
[Crossref] [Google Scholar] [PubMed]
- Moral S, Ballesteros E, Huguet M, Panaro A, Palet J, Evangelista A. Differential diagnosis and clinical implications of remnants of the right valve of the sinus venosus. J Am Soc Echocardiogr. 2016;29(3):183-194.
[Crossref] [Google Scholar] [PubMed]
- Su CS, Tsai IC, Lin WW, Lee T, Ting CT, Liang KW. Usefulness of multidetector-row computed tomography in evaluating adult cor triatriatum. Tex Heart Inst J. 2008;35(3):349.
[Crossref] [Google Scholar] [PubMed]
- Seth HS, Kulkarni S, Kattana HB. A case of “acquired” cor triatriatum. Indian J Thorac Cardiovasc Surg. 2021;37(5):569-572.
[Crossref] [Google Scholar] [PubMed]
- Church WS. Congenital malformation of heart-abnormal septum in left auricle. Trans Pathol Soc Lond. 1868;19:188-190.
- Van Praagh R, Corsini I. Cor triatriatum: Pathologic anatomy and a consideration of morphogenesis based on 13 postmortem cases and a study of normal development of the pulmonary vein and atrial septum in 83 human embryos. Am Heart J. 1969;78(3):379-405.
[Crossref] [Google Scholar] [PubMed]
- Rao S, Suntharos P, Najm H, Komarlu R. Cor triatriatum dexter with right ventricular hypoplasia: Role of multimodality imaging in decision making. Echocardiography. 2018;35(12):2113-2116.
[Crossref] [Google Scholar] [PubMed]
- Raheja H, Namana V, Moskovits N, Hollander G, Shani J. Cor triatriatum sinistrum. Arq Bras Cardiol. 2018;110:101.
[Crossref] [Google Scholar] [PubMed]
- Ullah W, Sattar Y, Rauf H, Roomi S, ishaq Shah M. A systematic review of a Long-forgotten cause of atrial fibrillation and stroke: Cor triatriatum. Cureus. 2019;11(12).
[Crossref] [Google Scholar] [PubMed]
- Lewis FJ, Varco RL, Taufic M, Niazi SA. Direct vision repair of triatrial heart and total anomalous pulmonary venous drainage. Surg Gynecol Obstet. 1956;102(6):713-720.
[Google Scholar] [PubMed]
- Kim D, Kwon BS, Kim DH, Choi ES, Yun TJ, Park CS. Surgical outcomes of cor triatriatum sinister: A single-center experience. J Chest Surg. 2022;55(2):151.
[Crossref] [Google Scholar] [PubMed]
- Burger C. A rare case of cor triatriatum leading to respiratory failure and shock in an 8-month-old boy. Pediatr Emerg Care. 2019;35(1): 6-8.
[Crossref] [Google Scholar] [PubMed]
- Capecci L, Mainwaring RD, Olson I, Hanley FL. Cor Triatriatum in Association With a Unique Form of Partial Anomalous Pulmonary Venous Connection. World J Pediatr Congenit Heart Surg. 2022;13(1):119-123.
[Crossref] [Google Scholar] [PubMed]
- Lee JO, Park CS. Cor triatriatum associated with total anomalous pulmonary venous connection: A rare but plausible combination. J Chest Surg. 2021;54(2):143.
[Crossref] [Google Scholar] [PubMed]
- Kazanci SY, Emani S, McElhinney DB. Outcome after repair of cor triatriatum. Am J Cardiol. 2012;109(3):412-416.
[Crossref] [Google Scholar] [Pubmed]
- Nagao H, Tanaka T. Mid-term outcomes of cor triatriatum repair: Comparison of biventricular physiology and univentricular physiology. Cardiol Young. 2021;31(2):186-190.
[Crossref] [Google Scholar] [PubMed]
- Naito Y, Harada Y, Uchita S, Takizawa K, Satomi G, Yasukochi S, et al. Successful surgical treatment of hypoplastic left heart syndrome associated with a divided left atrium that was diagnosed intraoperatively. J Thorac Cardiovasc Surg. 2007;133(3):813-815.
[Crossref] [Google Scholar] [PubMed]
- Khan MA, Almoukirish AS, Das K, Galal MO. Hypoplastic left heart syndrome, cor triatriatum and partial anomalous pulmonary venous connection: Imaging of a very rare association. J Saudi Heart Assoc. 2012;24(2):137-140.
[Crossref] [Google Scholar] [PubMed]
- Humpl T, Reineker K, Manlhiot C, Dipchand AI, Coles JG, McCrindle BW. Cor triatriatum sinistrum in childhood. A single institution's experience. Can J Cardiol. 2010;26(7):371-376.
[Crossref] [Google Scholar] [PubMed]
- Krasemann Z, Scheld HH, Tjan TD, Krasemann T. Cor triatriatum. Herz. 2007;32(6):506-510.
[Crossref] [Google Scholar] [PubMed]
- Nassar PN, Hamdan RH. Cor triatriatum sinistrum: Classification and imaging modalities. The Eur Heart J. 2011;1(3):84.
[Crossref] [Google Scholar] [PubMed]
- Spengos K, Gialafos E, Vassilopoulou S. Ischemic stroke as an uncommon complication of cor triatriatum. J Stroke Cerebrovasc Dis. 2008;17(6):436-438.
[Crossref] [Google Scholar] [PubMed]
- Takiya H, Kawai H, Koike S, Uji S, Kojima Y, Watanabe S, et al. A surgical case of cor triatriatum complicated by arterial multiple embolism in adult. Rinsho Kyobu Geka. 1990;10(1):69-71.
[Google Scholar] [PubMed]
- Nishimoto H, Beppu T, Komoribayashi S, Konno H, Tomizuka N, Ogasawara K, et al. A case of multiple cerebral infarction accompanied by a cor triatriatum. Neurosurgery. 2004;32(3):257-260.
[Google Scholar] [PubMed]
- Huang TY, Sung PH. Transesophageal echocardiographic detection of cardiac embolic source in cor triatriatum complicated by aortic saddle emboli. Clin Cardiol. 1997;20(3):294-296.
[Crossref] [Google Scholar] [PubMed]
- Park KJ, Park IK, Sir JJ, Kim HT, Park YI, Tsung PC, et al. Adult cor triatriatum presenting as cardioembolic stroke. J Gen Intern Med. 2009;48(13):1149-1152.
[Crossref] [Google Scholar] [PubMed]
- Amara RS, Lalla R, Jeudy J, Hong SN. Cardioembolic stroke in a young male with cor triatriatum sinister: a case report. Eur Heart J Case Rep. 2020;4(3):1-6.
[Crossref] [Google Scholar] [PubMed]
- Schuchlenz HW, Weihs W, Hackl E, Rehak P. A large Eustachian valve is a confounder of contrast but not of color doppler transesophageal echocardiography in detecting a right-to-left shunt across a patent foramen ovale. Int J Cardiol Heart Vasc. 2006;109(3):375-380.
[Crossref] [Google Scholar] [PubMed]
- Gać P, Martuszewski A, Paluszkiewicz P, Poręba R. Coexistence of cor triatriatum sinister, fibroelastoma and pulmonary veins ostial anatomy variant as incidental findings in coronary computed tomography angiography. Diagnostics. 2022;12(6):1449.
[Crossref] [Google Scholar] [PubMed]
- Rajekar H, Vasishta RK, Chawla YK, Dhiman RK. Noncirrhotic portal hypertension. J Clin Exp Hepatol. 2011;1(2):94-108.
[Crossref] [Google Scholar] [PubMed]
- Loeffler E. Unusual malformation of the left atrium: Pulmonary sinus. Arch pathol. 1949;48:371-376.
[Google Scholar] [PubMed]
- James TN. Classification of triatrial hearts. Anat Rec. 1962;143(1):79-91.
[Crossref] [Google Scholar] [PubMed]
- Andral G. Précis d'anatomie pathologique. Gabon; 1829.
- Preisz H. Beiträge zur Lehre von den angeborenen Herzanomalien. 1890; 7: 245-298.
- Cottier H. Vorhofseptumaneurysmen bei kongenitalen Herzfehlern. Pathobiol. 1955;18(6):1178-83.
[Crossref] [Google Scholar] [PubMed]
- Herlong JR, Jaggers JJ, Ungerleider RM. Congenital heart surgery nomenclature and database project: Pulmonary venous anomalies. Ann Thorac Surg. 2000;69(3):56-69.
[Crossref] [Google Scholar] [PubMed]
- Lam CR, Green E, Drake E. Diagnosis and surgical correction of 2 types of triatrial heart. Surg. 1962;51(1):127-37.
[Google Scholar] [PubMed]
- Saxena P, Burkhart HM, Schaff HV, Daly R, Joyce LD, Dearani JA. Surgical repair of cor triatriatum sinister: The Mayo Clinic 50-year experience. Ann Thorac Surg. 2014;97(5):1659-63.
[Crossref] [Google Scholar] [PubMed]
- Andral G. Précis d'anatomie pathologique. Gabon; 1829.
- Preisz H. Beiträge zur Lehre von den angeborenen Herzanomalien. 1890.
- Cottier H. Vorhofseptumaneurysmen bei kongenitalen Herzfehlern. Schweiz Z Pathol Bakteriol. 1955;18(6):1178-1183.
[Crossref],[Google Scholar],[Pubmed]
- Herlong JR, Jaggers JJ, Ungerleider RM. Congenital heart surgery nomenclature and database project: pulmonary venous anomalies. Ann Thorac Surg. 2000;69(3):56-69.
[Crossref],[Google Scholar],[Pubmed]
- Lam CR, Green E, Drake E. Diagnosis and surgical correction of 2 types of triatrial heart. Surgery. 1962;51(1):127-37.
[Crossref],[Google Scholar],[Pubmed]
- Saxena P, Burkhart HM, Schaff HV, Daly R, Joyce LD, Dearani JA. Surgical repair of cor triatriatum sinister: the Mayo Clinic 50-year experience. Ann Thorac Surg. 2014;97(5):1659-63.
[Crossref],[Google Scholar],[Pubmed]
- Tachibana K, Takagi N, Osawa H, Takamuro M, Yokozawa M, Tomita H, et al. Cor triatriatum and total anomalous pulmonary venous connection to the coronary sinus. J Thorac Cardiovasc Surg. 2007;134(4):1067-1069.
[Crossref] [Google Scholar] [Pubmed]
- Levin DB, Charlton G, Snider R, Roldan CA. Psuedo-cor triatriatum in an elderly patient with dyspnea of exertion: An undescribed condition characterized by 3-dimensional transesophageal echocardiography. J Investig Med High Impact Case Rep. 2021;9:23.
[Crossref] [Google Scholar] [PubMed]
- Yokoyama S, Mitani K, Fukuba R, Tonomura R, Uemura H. Cor triatriatum can coexist with common pulmonary venous atresia. Ann Thorac Surg. 2021;112(5): 337-339.
[Crossref] [Google Scholar] [PubMed]
- Elagha AA, Fuisz AR, Weissman G. Cardiac magnetic resonance imaging can clearly depict the morphology and determine the significance of cor triatriatum. Circulation. 2012;126(12):1511-1513.
[Crossref] [Google Scholar] [PubMed]
- Geva T. Is MRI the preferred method for evaluating right ventricular size and function in patients with congenital heart disease? MRI is the preferred method for evaluating right ventricular size and function in patients with congenital heart disease. Circ Cardiovasc Imaging. 2014;7(1):190-197.
[Crossref] [Google Scholar] [PubMed]
- Li WW, Koolbergen DR, Bouma BJ, Hazekamp MG, de Mol BA, de Winter RJ. Cathether-based interventional strategies for cor triatriatum in the adult–feasibility study through a hybrid approach. BMC Cardiovasc Disord. 2015;15(1):1-6.
[Crossref] [Google Scholar] [PubMed]
- Said SM. Commentary: Cor triatriatum dexter: A tale of 2 horns. JTCVS Tech. 2020;4:259-260.
[Crossref] [Google Scholar] [PubMed]
- Kerkar P, Vora A, Kulkarni H, Narula D, Goyal V, Dalvi B. Percutaneous balloon dilatation of cor triatriatum sinister. Am Heart J. 1996;132(4):888-91.
[Crossref] [Google Scholar] [PubMed]
- Hasnie UA, Prejean SP, Ahmed AN, Ahmed MI, Law MA. Transcatheter balloon dilatation of cor triatriatum dexter with percutaneous atrial septal defect closure. J Cardiol Cases. 2022;25(2):68-71.
[Crossref] [Google Scholar] [PubMed]
- Schiller O, Burns KM, Sinha P, Cummings SD. Cor triatriatum with partial anomalous pulmonary venous return: a rare case of parallel obstruction and successful staged treatment. Pediatr Cardiol. 2012;33(2):363-365.
[Crossref] [Google Scholar] [PubMed]
- Tuan SH, Chen GB, Chen CH, Liou I, Sun SF, Wu SY, et al. Serial cardiopulmonary exercise testing in an asymptomatic young female receiving percutaneous balloon dilatation for cor triatriatum sinistrum at an early age. J Formos Med Assoc. 2021;120(4):1143-1147.
[Crossref] [Google Scholar] [PubMed]
- Huang TC, Lee CL, Lin CC, Tseng CJ, Hsieh KS. Use of Inoue balloon dilatation method for treatment of Cor triatriatum stenosis in a child. Catheter Cardiovasc Interv. 2002;57(2):252-256.
[Crossref] [Google Scholar] [PubMed]
- Schranz D, Jux C, Akintuerk H. Novel catheter‐interventional strategy for intracardiac connecting of total anomalous pulmonary venous return in newborns with hypoplastic left heart‐syndrome prior to hybrid approach. Catheter Cardiovasc Interv. 2013;82(4):564-568.
[Crossref] [Google Scholar] [PubMed]
- Sivakumar K, Satish R, Tailor K, Coelho R. Transcatheter management of subtotal cor triatriatum sinister: a rare anomaly. Pediatr Cardiol. 2008;29(4):812-815.
[Crossref] [Google Scholar] [PubMed]
- Méndez AB, Colchero T, Garcia‐Picart J, Vila M, Subirana MT, Sionis A. Unusual case of new‐onset heart failure due to cor triatriatum sinister. Eur J Heart Fail. 2013;15(2):237-239.
[Crossref] [Google Scholar] [PubMed]
- Bhende VV, Majmudar HP, Sharma TS, Mehta DV, Kumar A, Thacker JP, et al. Successful repair of cor triatriatum sinistrum in childhood: a single-institution experience of two cases. Cureus. 2022;14(4).
[Crossref] [Google Scholar] [PubMed]
- Jennings Jr RB, Innes BJ. Subtotal cor triatriatum with left partial anomalous pulmonary venous return: successful surgical repair in an infant. J Thorac Cardiovasc Surg. 1977;74(3):461-466.
[Crossref] [Google Scholar] [PubMed]
- Soni KA, Bhende VV, Sharma TS, Majmudar HP, Kumar A, Trivedi BY, et al. Perioperative Management of Sickle Cell Disease in Complex Congenital Cardiac Surgery: A Compilation of Two Cases. Cureus. 2022;14(10).
[Crossref] [Google Scholar] [PubMed]
Citation: Cai ML, Zhong GQ (2023) Cor Triatriatum Sinister Combined with Dilated Cardiomyopathy. J Clin Res Bioeth. S12:001.
Copyright: © 2023 Cai ML, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

