Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 5, Issue 1
Congenital Glaucoma Epidemiological, Clinical and Therapeutic Aspects: About 414 Eyes
Mehdi Khamayli*, Sara Idmane, Loubna El Maaloum, Bouchra Allali, Asmaa El Kettani and Khalid ZaghloulReceived: 17-Feb-2020 Published: 09-Mar-2020, DOI: 10.35248/2684-1622.20.5.132
Abstract
Congenital glaucoma is a rare and severe pathology because it is potentially blinding. The aim of this study is to analyze the epidemiological, clinical and therapeutic aspects of this pathology in the pediatric ophthalmology department of Casablanca, Morocco. We conducted a retrospective descriptive study of all children admitted into our department from January 2002 until January 2018 for primary congenital glaucoma. The data collected concerned anamnestic and clinical parameters, management and evolution. 414 eyes belonging to 226 patients were included. The average age of diagnosis was 8.4 months, a sex ratio of 1.3, consanguinity at 61.9% with 14.2% of similar cases in the family, the mode of consultation was 85.5% done by the observation of an abnormal eye by the parents. The most common reason for consultation was megalocornea in 52%, the CG was bilateral at 82.7%, associated with a general pathology of 4.4%, the initial average IOP was of 18.2 mmHg The treatment time compared with the first consultation was 21 days on average, the most commonly used treatment was trabeculectomy associated with 5-FU at 97%, with a total success of 60.5%, partial success at 21.4% with or without hypotonic medical treatment. Surgical treatment should be instituted as soon as possible. In the absence of a well-defined consensus, the choice of the surgical method should be made taking into account the experience of the surgeon, and the age and the particularities of each patient.
Keywords
Cloning, Stem cells, Treatment, Moral problems
Introduction
Congenital Glaucoma (CG) is an ocular hypertonia that occurs at birth. It is a rare disease, present from the first days or during the first three years of life. It is severe, and potentially blinding, and constitutes a diagnostic and therapeutic emergency. Ocular hypertonia is the consequence of an abnormality of the iridocorneal angle and the anterior segment, manifested by trabeculodysgenesis with obstruction of the normal flow of the aqueous humor. It is a hereditary disease in 75% of cases, which is transmitted through the autosomal recessive mode. One of the genes is identified: it is the cytochrome oxidase CYP1B1 gene located on the long arm of chromosome 2 [1]. The warning signs are dominated by the triad photophobia, watering and megalocornea. In the past, the disease was desperate and provided a large number of blind children (between 2 and 15%) depending on the country [2]. The prognosis has evolved more favorably thanks to early surgery. However, there are no formal recommendations concerning the management of this condition and there are major differences between the healthcare teams.
Methods
This is a retrospective descriptive and analytical study including 414 eyes of children with congenital glaucoma confirmed by clinical ophthalmologic examination and monitored at the Pediatric Ophthalmology Department of the Hospital 20 August 1953 of CHU in Rochd of Casablanca, spread over a period of 16 years between January 2001 and January 2017
Exclusion criteria
Eliminated from our study are;
Children initially operated in another hospital structure.
Secondary glaucoma
Juvenile glaucoma
Children lost to follow up
The studied variables were: age at diagnosis, gender, geographical origin, medical history, deadline, mode and reason for consultation, unilateral or bilateral glaucoma, corneal diameter, the aspect of the cornea, preoperative IOP, cup-disc ratio, axial length, postoperative IOP, syndrome glaucoma. The criteria for success after trabeculectomy were 14 mm Hg under Fluothane®, with or without supplementary medical treatment. These data have been reported on a data sheet.
The data was logged using the SPSS software version 23.0.
Results
Epidemiological results
Our series includes 414 eyes in 226 children.
Age: The age at diagnosis varied from 2 days to 4 years, with an average of 8.4 months. The disease was discovered in the first six months of life in 328 cases (77.5%).
Gender: In our series, there is a slight male predominance. The sex ratio was 1.3.
Geographical origin: The urban origin was found in 80% of the cases, compared to 20% coming from the rural environment.
Consanguinity: Inbreeding was found in 140 children, that is 61.9% of the children. In 79% of cases, this was first-degree inbreeding.
Heredity: The presence of a family history of glaucoma was found in 32 patients, i.e. 14.2%
No genetic studies have been performed.
Pregnancy course: (Table 1)
| Pregnancy with incidents | 6 children |
|---|---|
| Pre eclampsia | 1 |
| Gestational hypertension | 2 |
| Materno-foetal infection | 2 |
| Hydramnios | 1 |
| Abnormal Childbirth | 12 children |
| C section | 7 |
| Perinatal asphyxia | 2 |
| Premature rupture of membranes | 1 |
Table 1: Pregnancy and childbirth (incidents).
Pregnancy with incidents: 6 children
Abnormal childbirth: 12 children
The timeline of consultation: The timeline between finding the ocular abnormality and physician consultation ranged from 1 day to 4 years, with an average of 7.4 months
Method of consultation: 192 children (85.5%) were brought for medical treatment due to parents noticing an "abnormal" eye. 22 children (9.7%) were referred by the pediatrician, in most cases in the neonatal period. 7 children (3.1%) were randomly diagnosed following a screening campaign, or following systematic consultation of members of a family at risk. 2 cases (0.9%) were suspected by the gynecologist in the neonatal period. 3 children (1.3%) were referred by the general practitioner (Figure 1).
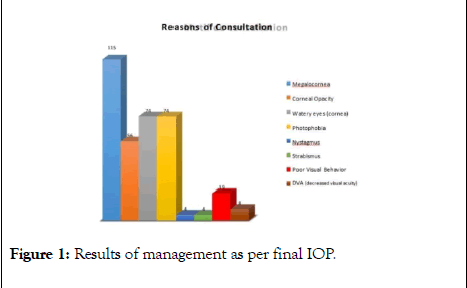
Figure 1: Results of management as per final IOP.
Reason for consultation: In our series the most common reason for consultation was megalocornea in 115 children (52%). Watering and photophobia were found in 74 children (33%). Corneal opacity was a reason for consultation in 56 children (24%). Nystagmus and strabismus were a reason in 4 children (1.7%). The decrease in visual acuity (DVA) was found in 8 children (3.5%).
Clinical results
Laterality
The damage was bilateral in 187 children (82.7%)
Unilateral in 39 children (17.3%)
Examination of the cornea: (Table 2)
The average horizontal corneal diameter was 13.59 mm [11-18 mm].
The cornea was abnormal in 372 (89.9%) of the eyes.
The iris: (Table 2)
The iris was abnormal in 13.3% of cases or in 55 eyes.
Examination of the anterior chamber: The anterior chamber was deep in 54.2% of the children.
Examination of the Crystalline Lens: (Table 2)
| Abnormalities | Abnormalities | Number of eyes | Eyes percentage |
|---|---|---|---|
| C | Megalocornea | 311 | (75,3%) |
| O | Opacity | 60 | (14,5%) |
| R | Dystrophy | 135 | (32,6%) |
| N | Haab stria | 204 | (49,3%) |
| E | Edema | 127 | (30,8%) |
| A | Corectopia | 23 | (5,5%) |
| P | Iridodonesis | 6 | (1,4%) |
| U | Aniridia | 12 | -3% |
| P | Iris Atrophies | 6 | (1,4%) |
| I | Pupillary membranes | 2 | (0,5%) |
| L | Iris Coloboma | 6 | (1,5%) |
| CR | Cataract | 9 | (2,1%) |
| IS | Ectopia | 2 | (0,5%) |
| TA | Iris deposits | 4 | -1% |
| LL | Dislocation | 4 | -1% |
Table 2: Distribution of abnormalities (corneal, pupillary and crystalline) as per number of eyes.
19 eyes had an abnormal crystalline lens (4.6%)
The axial length: The axial length was between 36 and 19 mm for an average of 22.75 mm
Intraocular pressure (IOP): The average initial IOP under GA was 18.2 mmHg [11-36 mmHg]
The papilla: The fundus of eye was disturbed in 16.7% of the cases. The papillary excavation was >3/10 in 67.3%
The papilla was normal in 0.9% of the eyes.
Syndrome Glaucoma: (Table 3)
| Number of eyes | Percentage | |
|---|---|---|
| Total success | 250 | 60,5% |
| Partial success | 89 | 21,4% |
| Failure | 75 | 18,1% |
Table 3: Results of management as per final IOP.
The CG was syndromic at 4.4%, in 10 cases.
Therapeutic results
The average deadline between the first consultation and surgical management was 21 days on average (Table 3).
The average deadline to the management of the second eye was 1 week in the bilateral CG.
414 eyes were operated, 402 eyes by trabeculectomy and 10 eyes by sclerectom.
5FU was used at 93.4% and 6.6% for Mitomycin.
The intervention was considered a total therapeutic success if the final IOP is less than 12 mmHg under general anesthesia.
The success is partial if IOP is maintained below 12 mmHg with the addition of hypotonic drugs.
The therapeutic result is considered a failure if the IOP is greater than or equal to 12 mmHg with a hypotonic treatment.
39.5% reported postoperative ocular hypertonia requiring medical treatment including 18.9% monotherapy, 18.1% bitherapy and 3.5% tri-therapy.
73 eyes, that is 18.1% showed therapeutic failure requiring surgical recovery.
Discussion
Epidemiology
Frequency: Congenital glaucoma is a rare disorder that represents 0.01-0.04% of cases of total blindness, according to most authors [3], however, the prevalence at birth varies throughout the world; In France, for example, it is estimated at 1 case per 10,000 to 15,000 births [4]. In the Indian state of Andhra Pradesh, the prevalence is 1/3300, where the disease accounts for about 4.2% of cases of childhood blindness [5]. 0.10% in Senegal [6] and 0.26% in Tunisia [7]. This can be explained by the high rate of consanguineous marriages in Africa.
Despite considerable therapeutic progress, the CHU of Casablanca alone records 40 to 50 new cases each year [8]. Congenital glaucoma remains a blinding disease; in fact children with congenital glaucoma represent 2 to 15% of the population with visual impairment [9] and 2 to 18% of these children have bilateral congenital glaucoma [10].
Age at diagnosis: For ZECH [8] in Lyon, diagnosis occurs very often shortly after birth, in the first week after delivery in 39% of cases. In 80% of cases, diagnosis is made before the age of 1 month.
The condition was diagnosed in the first year of life in 85.2% of cases, as reported by NACEF [7] in Tunis and SAFEDE [11] in Abidjan. In our series, the average age of diagnosis was 8.4 months.
A delay in diagnosis is thus observed in the African context. This could be explained not only by parents' ignorance of the first warning signs of the disease, but also by their mentality of often consulting traditional healer’s firstzz.
Gender: There was a male predominance in 56.6% versus 43.4% of girls with a sex ratio of 1.3. This is found in the literature, often estimated at two thirds of boys [12].
Consanguinity: In terms of consanguinity, it is recognized that CG is a more common pathology in inbred populations. It is therefore not surprising to find a rate of 61.9% in our study.
Heredity: The hereditary nature of congenital glaucoma is found in 32 children, that is 14,2% of the cases of our series, this corroborates with the studies carried out in the Maghreb and the Middle East.
The clinic
Type of damage: The damage is bilateral in 82.7% of the children of our series; this result is in line with those of the studies on congenital glaucoma in general. In fact, the reported bilateral damage rate ranged from 70% to 80%.
Corneal diameters: According to Hilal, the corneal diameter measured after general anesthesia varied between 11 mm and 18 mm with an average of 14.05 ± 1.8 mm.
In the Tixier series the average corneal diameter at the time of operation ranged from 13 mm to 18 mm with an average of 14.3 mm.
In our series, the average corneal diameter (13.59 mm) is larger compared to the literature. Indeed, ocular distension is a normal consequence of the diagnostic and therapeutic delay of most of our patients.
Intraocular pressure: In the literature IOP varied between 24 and 36 mmHg according to Denis, Elssayad and El-Raggal, Hila, Essuman and Mohcine found an average ocular tone at admission prior to surgery of 21.6 mmHg, 26.9 mmHg, 30.6 mmHg, 30.3 mmHg and 28 mmHg respectively
Examination of the papilla: For Tixier the cup-disc ratio ranged from 1/10 to 8/10 (average 4.6/10). In our study, fundus examination found pathological papillary excavation in 67, 3% of cases with an average C/D ratio of 4.5/10 ranging from (2/10 to 9/10), otherwise the fundus was disturbed in 16.7% of the cases (very important corneal edema, corneal opacity).
Therapeutic care
The criteria of total success are fulfilled in 60.5% of the cases and partial success in 21.4%. NACEF [4] in Tunisia reported a success rate of 64.2% after postoperative monitoring for one year. These relatively unsatisfactory results could be explained by the delay in the diagnosis of our patients. As for the postoperative functional result, it is difficult to assess due to the young age of the patients.
Conclusion
Congenital glaucoma is a rare, severe and potentially blinding disease, constituting a diagnostic and therapeutic emergency. Surgical treatment should be instituted as soon as possible, in the absence of a well-defined consensus, the choice of the surgical method should be made taking into account the experience of the surgeon and the age and particularities of each patient. In all cases, glaucomatous eyes remain fragile eyes, subject to many complications. Amblyopia is almost constant, hence the importance of raising awareness among fellow pediatrician and especially genetic counseling in families at risk.
REFERENCES
- Roche O, Kaplan J Congenital and megalocorneal glaucoma. J Med Childhood. 1996;5:43-48.
- DetrY-morel M Congenital glaucoma. Bull Soc Belgian Ophthalmol. 2001;281:49-58.
- Mandal AK, Chakrabarti D Update on congenital glaucoma. Indian J Ophthalmol. 2011;59(7):148.
- Demailly P, Dhermy P Les glaucomes congénitaux. Encycl Med Chir Ophthalmology,1981;212(80):1-15.
- Khaw PT What is the best primary surgical treatment for the infantile glaucomas? Br J Ophthalmol. 1996;80(6):495.
- Seye C, BA E, Ndiaye MR, Ndoye NB, Ndiaye PA, Wade A Le glaucome congénital. Dakar Méd.1994;1:87-93.
- ROCHE O, KAPLAN J Glaucome congénital et mégalocornée. J Med Enfance. 1996;5:43-48.
- Lahbil D, Hamdani M, Rais L, Elkettani A, Laouissi N, Zaghloul K et al. Modified trabeculectomy for the treatment of congenital glaucoma. J Soc Mar Ophtalmol. 2003;15(16):26.
- Dureau P Congenital glaucoma and trabeculodysgenesis: Clinical and genetic aspects. French Journal of Ophthalmology. 2006;29(2):198-215.
- Detry-Morel M, Feron E Trabeculectomy in the treatment of congenital glaucoma: expérience rétrospective à moyen et long terme. Bulletin of the Belgian Ophthalmological Society. 1996;262:143-51.
- Safede K, Koffi KV, Kouassi FX, Keita C, yoffou AL, Yago D, et al. Glaucome congenital: Clinical and therapeutic aspects of 42 cases collected in the ophthalmology department of the Cocody University Hospital in Abidjan.
- Renaudin AN Congenital glaucoma surgery. Thesis for obtaining a doctorate in medicine Angers-France. 2001.
Citation: Khamayli M, Idmane S, El Maaloum L, Allali B, El Kettani A, Zaghloul K (2020) Congenital Glaucoma Epidemiological, Clinical and Therapeutic Aspects: About 414 Eyes. J Eye Dis Disord 5: 132 DOI: 10.35248/2684-1622.20.5.132
Copyright: © 2020 Khamayli M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
