Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 20, Issue 10
Comparison of Pre-Adjusted 3D Plating System Employing 3D Printing Verses Conventional 3D Plating in the Management of Mandibular Fractures: A Randomized Controlled Trial
Prajwalit P. Kende, Ashish Sunilkumar Sarda*, Jayant Landge, Maroti Wadewale, Varthangpuii and Suleka Ranganath
Abstract
Objective: The aim of this study is to compare the efficacy of pre-adjusted 3D plating system employing 3D printing with conventional 3D plating in the management of mandibular fractures.
Methods: A randomized, controlled trial was conducted where the study sample (n=20) were randomly divided into two groups with age ranging from 18-45 years. In group 1 (control group), 3D plate was adapted and fixated conventionally to the fracture site while in group 2 (experimental group), pre-bent 3D plate was adapted and fixated to the fracture site. The primary outcomes assessed were number of bends required to adapt 3D plate and duration of fracture fixation. The secondary outcomes assessed were pain during adaptation of 3D plate, postoperative occlusal stability, and reduction in lingual splaying and postoperative complications. CONSORT guidelines have been followed for this Randomised Controlled Trial.
Results: There was a statistically highly significant difference seen for the values between group 1 and group 2 for the number of bends required (p=0.000, p<0.01) and duration of fracture fixation (p=0.001, p<0.01). There was statistically significant difference seen between the values of pain during adaptation of 3D plate (p=0.033, p<0.05). There was no statistically significant difference seen for postoperative occlusal stability, reduction in lingual splay and postoperative complications.
Conclusion: Application of pre-adjusted plates is superior to conventionally applied plates in terms of reducing the number of bends, duration of fracture fixation and pain during adaptation of 3D plate.
Keywords
Mandibular Fracture, Open Reduction, 3D plate, 3D printing, Stereo Lithographic Models.
Introduction
Management of mandibular fracture has evolved from various forms of splinting to circummandibular wiring, extra oral pins and semi rigid fixation with transosseus wiring followed by rigid fixation technique, which has lately given way to semi – rigid fixation with miniplate. [1] To overcome the shortcomings semirigid fixation using miniplates like inability to render 3D stability and need for maxillomandibular fixation, Farmand (1992) [2] developed a new miniplate system, which takes advantage of the bio–geometry to provide stable fixation- “3D plating system”. The 3D plating systems are based on the principle of obtaining support through geometrically stable configuration and its quadrangle geometry assures a good stability in three dimensions of fracture. Also, this plating uses fewer plates and screws as compared to the conventional miniplates, reduces the operation time and overall cost of the treatment. However, due to its configuration, it is needed to bend it in a plane to adapt the fracture site unlike conventional miniplates which are bent in a line. It increases the time and number of bends which can lead to increased discomfort and plate fatigue respectively.
Hull [3] invented 3D printing “stereo lithography” (STL) in the early 1980’s. 3D planning and printing is used to prepare preoperative 3D models, stents, and guides to facilitate surgery, the use of which can drastically reduce the operating room time. King [4] concluded that on-site 3D model fabrication with preoperative plate bending is a timeeffective option to provide predictable reconstructive solutions with an associated decrease in operative time in management of mandibular fractures.
We conducted a randomized controlled trial to compare the efficacy of pre-adjusted 3D plates on surgical models received after 3D printing with conventionally intraoperative applied 3D plates in the management of mandibular fractures.
Materials and Methods
A prospective, randomized controlled clinical trial was carried out in the department of oral and maxillofacial surgery from June 2020 to November 2020 following CONSORT guidelines. A total of 20 patients were selected in the age group from 18-45 years without discrimination based on gender, socioeconomic status, religion, and cast. The study population was divided into control group (group 1) and experimental group (group 2). Patients included were those with no significant medical history, with unilateral and/or bilateral fracture present on symphysis, parasymphysis or angle of mandible region, where vital structures will not cause any interference, and those giving informed consent. Patients excluded were those not willing for participation in the study, having history of any systemic diseases, pregnant and lactating patients, with condylar/subcondylar/coronoid fractures, with severe comminuted fractures, with midfacial fractures and those not willing for open reduction. Preoperatively, cone beam computed tomography (CBCT) scan was taken with mandible. Block randomization was done with the help of software and the random sequence was not revealed to any investigator and was known only to that expert. The procedure of allocation was carried out by an expert, who was not involved in any part of the data collection or surgical procedure, thus maintaining concealment.
Group 1 patients underwent osteosynthesis using conventionally applied 2-mm 3D plate, whereas group 2 patients underwent osteosynthesis using pre-bent 2.0-mm 3D plate. They were informed of the need for a 6- month follow-up. The patients were required to provide informed consent or to state refusal to participate in the study. Patient information was documented on a consent form.
Surgical Procedure
Under all aseptic precautions and under local anesthesia, routine scrubbing and draping was done as per the protocol. Circumlinear vestibular incision was made as per the fracture site. Extraction of tooth in fracture line if indicated was done. Complete mucoperiosteal flap was reflected and the vital structures were identified and preserved. Fracture site was exposed; debrided and sharp bony prominences were trimmed. Functional and anatomic reduction was achieved and intermaxillary fixation (IMF) was done using 26-gauge wire. After establishment of occlusion, in group 1 patients, adaptation and fixation of 2 mm titanium (Ti) 3D plate to the fracture site was done using Ti screws. Whereas, in group 2 using CBCT scan (Figure 1) and 3D printing technology, fabrication of a stereo-lithographic (STL) model was done. The 3D STL model was re-fractured using saw and reduced anatomically with the reference point of inferior border of mandible. A 2 mm 3D plate was adapted over the model preoperatively using plate bender and then sterilized (Figure 2). ORIF was done as discussed in control group (Figure 3). After confirming the pre-injury occlusion and achieving complete haemostasis, the incision site was closed layerwise using 3-0 Vicryl sutures. Following this, patients were prescribed a 5-day course of oral antibiotics. Any further development of occlusal discrepancy was treated by maxillomandibular fixation (MMF) for 7 days. Patients were instructed to maintain a soft diet for 4 weeks.
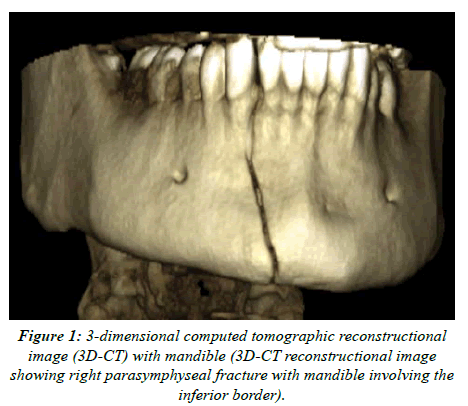
Figure 1:3-dimensional computed tomographic reconstructional image (3D-CT) with mandible (3D-CT reconstructional image showing right parasymphyseal fracture with mandible involving the inferior border).
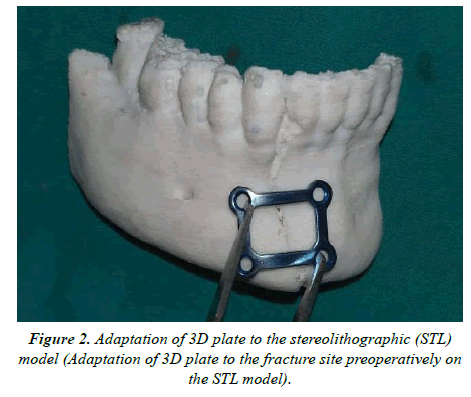
Figure 2:Adaptation of 3D plate to the stereolithographic (STL) model (Adaptation of 3D plate to the fracture site preoperatively on the STL model).
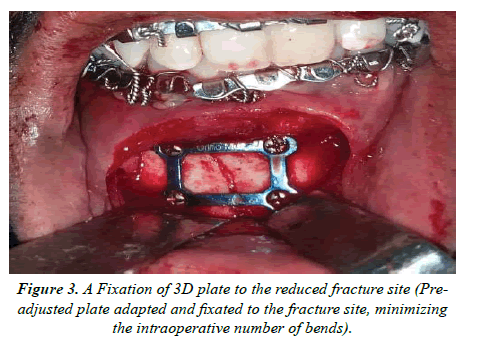
Figure 3:A Fixation of 3D plate to the reduced fracture site (Preadjusted plate adapted and fixated to the fracture site, minimizing the intraoperative number of bends).
Assessment
Primary outcomes assessed were number of bends required for adaptation of 3D plates and time required from adaptation of plate till fixation of last screw in minutes. Secondary outcomes assessed were pain during adaptation of 3D plate measured with visual analog scale (VAS) [5] intraoperatively, postoperative occlusal stability checked 3rd day, 7th day, 3 months and 6 months interval, reduction in lingual splay checked at 3rd day using CBCT and postoperative complications assessed at 7th day, 3 months and 6 months interval. Analysis and measurements were performed by the same assessor twice in order to eliminate the intra-observer error; the mean was then calculated and recorded for further statistical analysis Descriptive statistics like frequencies and percentage for categorical data, mean and standard deviation (SD) for numerical data was depicted. Inter group comparison was done using ‘t’-test and comparison of frequencies of categories of variables with groups was done using chi square test. For all the statistical tests, p<0.05 was considered to be statistically significant.
Results
There were total 20 patients in our study (Figure 4 and Figure 5), with age ranging from 21 years to 44 years with mean age of 28.10 years. No cases were lost to follow up. Total number of male patients was 18 (90%), compared to female patients 2 (10%). Among all 20 patients, 6 (30%) were having left parasymphyses fracture, 8 (40%) were having right parasymphyses fracture, 2 (10%) were having symphyseal fracture, 3 (15%) were having left parasymphyseal and rightangle fracture and 1 (5%) was having left parasymphyses and right body fracture. Single fracture was present in 16 patients while more than one fracture was present in 4 patients. Fall was the leading cause of fracture in 10 (50%) patients followed by road traffic accident in 8 (40%) patients and assault in 2 (10%) patients. 3D plate was applied in 10 (50%) left parasymphyses regions, 8 (40%) right parasymphyses regions and 2 (10%) symphyseal regions. Both, group 1 and 2 were having 9 male patients and 1 female patient each. 3D plate was applied in 9 patients at parasymphyseal region in each group while 1 patient at symphyseal region in each group. There was a statistically non-significant difference seen for the frequencies between the groups (p>0.05). Mean number of fractures in group 1 was 1.3 while in group 2 was 1.1. There was a statistically non-significant difference seen for the values between the groups (p>0.05) for number of fractures.

Figure 4: 3rd day CBCT (axial view) (3rd day CBCT scan was taken to assess the reduction in lingual splay is checked on the axial view, complete reduction in lingual splay can be seen).
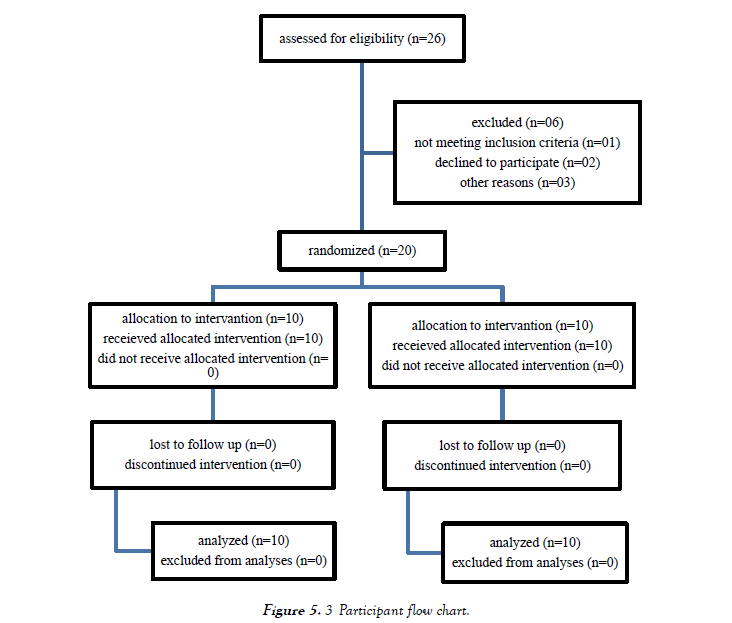
Figure 5: 3 Participant flow chart.
Mean number of bends in group 1 were 5.3, while in group 2 were 3. There was a statistically highly significant difference seen for the values between the groups (p<0.01) for no of bends with higher values in Group 1. Mean operative time required in group 1 was 22.7 minutes; while in group 2 was 15.5 minutes. There was a statistically highly significant difference seen for the values between the groups (p<0.01) for no of bends with higher values in Group 1. Mean value for pain in group 1 was 5.6 and in group 2 were 4.6. There was a statistically significant difference seen for the values between the groups (p<0.05) for Pain (VAS) with higher values in group 1 (Table 1).
| S.No | Parameter | Group 1 (n= 10) | Group 2 (n=10) | ‘p’ value |
|---|---|---|---|---|
| 1 | Number of bends | 5.3 | 3 | 0.000** |
| 2 | Time | 22.7 | 15.5 | 0.001** |
| 3 | Pain | 5.6 | 4.6 | 0.033* |
Table 1. Comparison of frequencies of subjects between groups for number of bends, time and pain. *complications seen immediately during the given phases of DO/ at that given point of time.
Discussion
ORIF is considered as the “gold standard” for the fixation of maxillofacial fractures. As maxillo-mandibular fixation is not needed, there is increased patient comfort, improved speech and oral hygiene, enhanced social interaction, and a decreased number of hospital visits [6-8]. 3D plating systems was developed to render greater stability against torque forces, simultaneous stabilization at both superior and inferior borders of the mandible and less operative time was achieved. Though 3D geometry of this plate offers better bending stability and more resistance to out of plane movement or torque than conventional mini-plates, this plate is difficult to adapt and requires more bending as compared to later. The purposes of this study were to validate our hypothesis that the use of 3D printed models and preoperatively bent 3D plates for management of mandibular fractures would be associated with decreased number of plates bending, operating time, pain and postoperative complications.
Out of 20 patients, 18 patients were male and 2 patients were female, which is similar to that reported in literature. The main cause for mandibular fracture in our study was fall followed by road traffic accident. It was not in accordance with the given literature, [9] in which RTA accounted for most of the mandibular fractures (83.3%). The reduced incidence of fracture with RTA is attributed to increased use of precautionary gears like seat belts and helmets in the recent years. The most common site of the fracture of the mandible was parasymphysis followed by parasymphysis and angle, symphysis, parasymphysis and body.
The mean number of bends in group 1 was 5.30, while in group 2 were 3. There was a statistically highly significant difference (p= 0.00; p<0.01) for the values between the groups for no of bends with higher values in Group 1. The reduced number of bends in group 2 can be attributed to the use of 3D, STL model preoperatively for adaptation of plate, and was in accordance with those given in the literature by King [10]. However, in contrast to his study where he calculated only corrective intraoperative bends, we have calculated the number of bends given intraoperative as well as preoperatively. It is important to minimize the number of bends for adaptation of the plate as it may lead to decreased strength of plate, more fatigue, and stress induced fracture [11]. In group 1 and group 2, the mean score for pain was 5.60 and 4.60 respectively, showing statistically significant difference between their values (p=0.033, p<0.05). This increased value for pain in group 1 can be attributed to increased surgical time causing more discomfort to the patient. The mean time required for plate adaptation and fixation in group 1 was 22.70 minutes that of in group 2 was 15.50 minutes, showing statistically highly significant difference (p=0.001, p<0.01). Our results can be correlated with the study done by Brett J. King. The reduced number of bends given intraoperative can be a major reason for the reduction of time required in group 2.
There was no loss of molar relationship in all the patients in group 1. However, in group 2 there was unilateral loss of molar relationship in two patients. Both the patients were kept on elastic traction. At 7 days follow up, satisfactory occlusion was achieved in one patient and IMF was placed for 1 month. In second patient, there was a complete loss of molar relationship of one side. Occlusal stability assessed in this study was in accordance with that given in literature.12,13 Significant reduction of lingual splay was achieved in all the patients (100%) in contrast to the study done by Rajendra [12-14], he achieved significant reduction of lingual splaying in 72.2% of his cases. There was no any evidence of complications in group 1 visible clinically at the follow up visits. While in group 2, one patient was having transient paraesthesia with left side of lower lip at 7th day and another patient was having deranged occlusion with right side. Transient paraesthesia was treated with vit B supplements. These results are in agreement with those reported in published literature.
Conclusion
In the present study, pre-adapted 3D plates were superior to conventionally adapted 3D plates in terms of reduced operative time, less intraoperative pain, reduction in plate fatigue and lesser overall postoperative complications. Also, assessing a 3D model preoperatively can give operator an idea about the severity of fracture, the anatomy of bone and predefine the location of plate to the fracture location. However, to more correctly define all these parameters, a randomize controlled trial with larger sample size needs to be done. Also, the overall success of 3D plating system for fixation of various maxillofacial fractures needs to be explored. The widespread use of 3D STL models made with 3D printing have become a routine for majority of craniofacial surgeons for orthognathic surgeries, distraction osteogenesis (DO), dental implant surgeries, various reconstructional surgeries, pan facial fractures and so on and still needs to be explored.
REFERENCES
- Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. Journal of Oral and Maxillofacial Surgery. 1978; 6: 14‑21.
- Farmand M. The 3d plating system in maxillofacial surgery. Journal of Oral and Maxillofacial Surgery. 1993; 51: 166‑700.
- Joseph K, Hull C. 3D Printing Role in Oral and Maxillofacial Surgery Current and Future Trends. Advances in Dentistry and Oral Health. 2016; 2: 555-588.
- King BJ, Park EP, Christensen BJ, Danrad R. On-site 3-dimensional printing and preoperative adaptation decrease operative time for mandibular fracture repair. Journal of Oral and Maxillofacial Surgery. 2018; 76: 1950-e1.
- Campbell WI, Lewis S. Visual analogue measurement of pain. The Ulster Medical Journal. 1990; 59: 149-154.
- Snell JA, Dott WA. Internal fixation of certain fractures of the mandible by bone plating. Journal of Plastic, Reconstructive and Aesthetic Surgery. 1969; 43: 281-0e286.
- Hayter JP, Cawood JI. The functional case for miniplates in maxillofacial surgery. International Journal of Oral and Maxillofacial Surgery. 1993; 22: 91-e96.
- Saluja H, Kini Y, Mahindra U, Kharkar V, Rudagi BM. A comparative evaluation of different treatment modalities for parasymphysis fractures: a pilot study. Journal of Oral and Maxillofacial Surgery. 2012; 41: 906-e911.
- Sehgal S, Ramanujam L, Prasad K, Krishnappa R. Three-dimensional v/s standard titanium miniplate fixation in the management of mandibular fractures--a randomized clinical study. Journal of Cranio-Maxillofacial Surgery. 2014; 42: 1292-1299.
- King BJ, Park EP, Christensen BJ, Danrad R. On-Site 3-Dimensional Printing and Preoperative Adaptation Decrease Operative Time for Mandibular Fracture Repair. Journal of Oral and Maxillofacial Surgery. 2018 ; 76: 1950e1-1950e8.
- Martola M, Lindqvist C, Hänninen H, Al-Sukhun J. Fracture of titanium plates used for mandibular reconstruction following ablative tumor surgery. Journal of Biomedical Materials Research. 2007; 80: 345-352.
- Mittal G, Dubbudu RR. Three dimensional titanium miniplates in oral and maxillofacial surgery: a prospective clinical trial. Journal of Oral and Maxillofacial Surgery. 2021; 11: 152e-159.
- Van Den Bergh B, Heymans MW, Duvekot F, Forouzanfar T. Treatment and complications of mandibular fractures: A 10-year analysis. Journal of Cranio-Maxillofacial Surgery. 2012; 40: e108-e111.
- Rajendra P. The Role of 3D Plating System in Mandibular Fractures: A Prospective Study. Journal of Pharmacy and Bioallied Sciences. 2013.
