Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
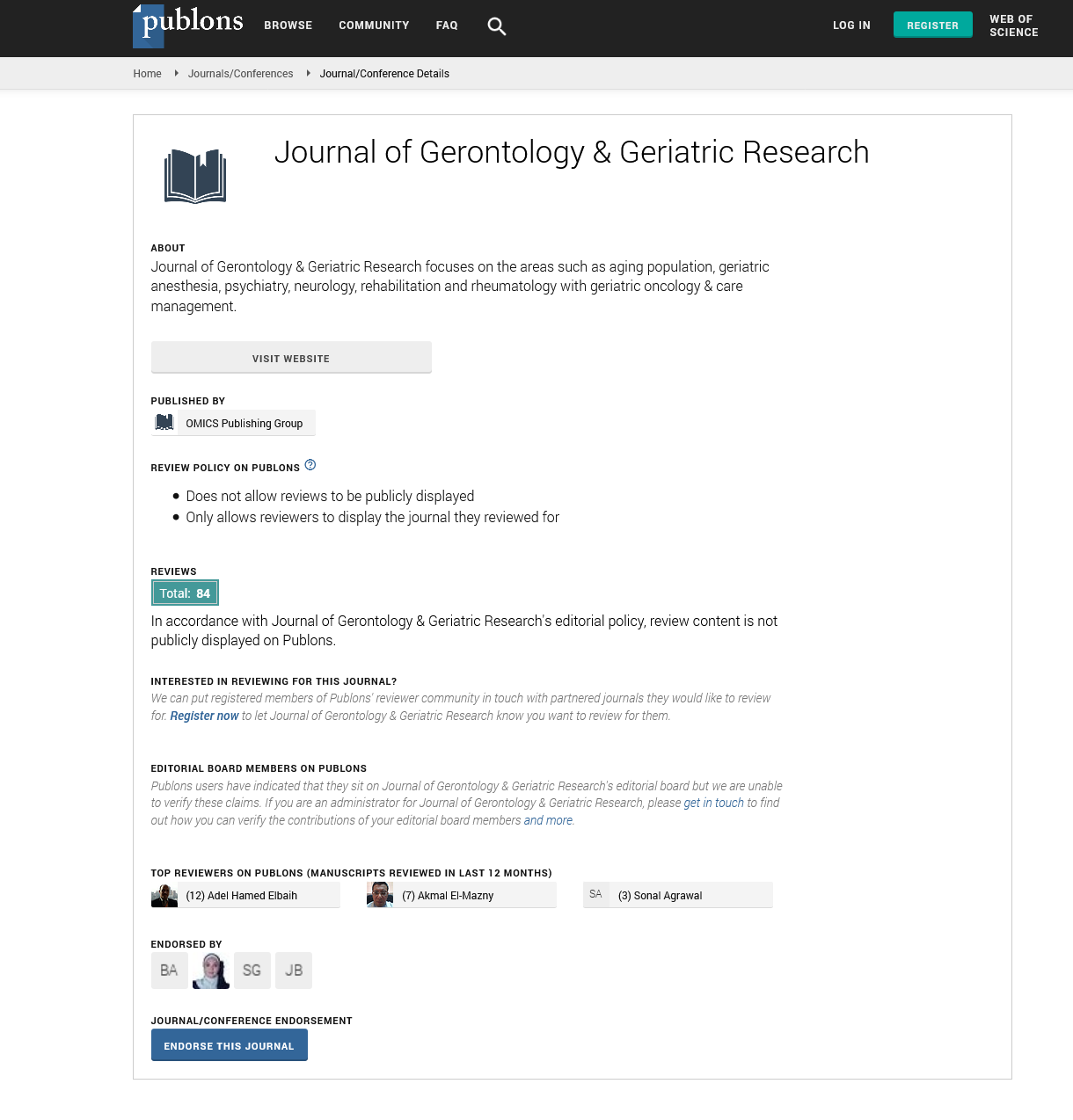
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2023) Volume 12, Issue 4
Comparative Effectiveness of Therapeutic Modalities for Geriatric Depression
Toyin Adewale*Received: 01-Aug-2023, Manuscript No. jggr-23-22786; Editor assigned: 03-Aug-2023, Pre QC No. P-22786; Reviewed: 16-Aug-2023, QC No. Q-22786; Revised: 21-Aug-2023, Manuscript No. R-22786; Published: 28-Aug-2023, DOI: 10.35248/2167-7182.2023.12.687
Abstract
Geriatric depression, a prevalent mental health concern among the elderly population, poses significant challenges to both the affected individuals and the healthcare system as a whole. As the world's population continues to age, understanding and addressing the most effective therapeutic modalities for geriatric depression becomes imperative. This paper delves into the comparative effectiveness of various therapeutic approaches in treating geriatric depression, including psychotherapy, pharmacotherapy, and alternative interventions, while also considering factors such as safety, accessibility, and patient preferences.
Keywords
Geriatric depression; Cognitive-behavioural therapy; Depression
Introduction
Geriatric depression, also known as late-life depression, affects a considerable portion of older adults worldwide. The prevalence of depression in this population varies, but estimates suggest that around 7-10% of older adults experience significant depressive symptoms. Geriatric depression has a profound impact on the individual's quality of life, cognitive functioning, physical health, and overall well-being. It is associated with increased morbidity, mortality, and healthcare utilization, making effective interventions crucial. Psychotherapy, often referred to as talk therapy, encompasses various approaches such as Cognitive-Behavioral Therapy (CBT), Interpersonal Therapy (Ipt), and psychodynamic therapy. These therapies aim to identify and modify maladaptive thought patterns, enhance coping skills, and promote emotional regulation. Psychotherapy offers several advantages for geriatric depression.
Literature Review
CBT is one of the most extensively studied and validated psychotherapeutic modalities for geriatric depression. It focuses on identifying and challenging negative thought patterns and behaviours, leading to more adaptive cognitive and emotional responses. CBT has been shown to be effective in reducing depressive symptoms, improving quality of life, and enhancing overall functioning in older adults. IPT centres on improving interpersonal relationships and communication skills. Given the social isolation that many elderly individuals experience, IPT can be particularly valuable. By addressing issues related to grief, role transitions, and interpersonal conflicts, IPT helps alleviate depressive symptoms and enhance social support networks.
Discussion
Psychodynamic therapy explores unconscious processes and unresolved conflicts that may contribute to depressive symptoms. While research on its effectiveness in geriatric depression is more limited, some studies suggest positive outcomes, especially in cases where unresolved past experiences significantly impact an individual's mental well-being. Pharmacotherapy involves the use of antidepressant medications to alleviate depressive symptoms. While pharmacological interventions have shown efficacy in treating geriatric depression, careful consideration of potential side effects, drug interactions, and individual differences is essential [1].
SSRIs, such as sertraline and fluoxetine, are often considered first-line options due to their relatively favourable side effect profiles and effectiveness. However, response rates can vary among individuals, and older adults may be more susceptible to drug interactions and adverse effects. Serotonin-Norepinephrine Reuptake Inhibitors SNRIs like venlafaxine target serotonin and norepinephrine systems, potentially offering broader benefits. However, similar to SSRIs, caution is required when prescribing to older adults. Medications like bupropion and mirtazapine affect neurotransmitter systems differently and may be considered when other options are ineffective or not well-tolerated.
TCAs have been used for decades but are generally considered second-line due to their greater potential for adverse effects and interactions. Some individuals may benefit from a combination of psychotherapy and pharmacotherapy. The synergy between psychotherapy's cognitive and behavioural strategies and the neurochemical effects of medication can provide comprehensive support for geriatric depression [2].
Geriatric depression often goes undiagnosed and undertreated due to factors such as stigma, overlapping symptoms with medical conditions, and communication barriers. Enhancing awareness among healthcare providers and the public can improve identification and access to appropriate interventions. The field of precision medicine holds promise for tailoring treatments based on an individual's genetic, biological, and psychological characteristics. Personalized treatment plans could optimize outcomes and minimize adverse effects. Collaborative care models that integrate mental health and primary care services can improve access to appropriate interventions for geriatric depression. This approach ensures a comprehensive assessment and management of both mental and physical health. The expansion of telehealth and digital interventions provides opportunities for reaching older adults who may have mobility or transportation limitations. Tele therapy and mobile applications can deliver psychotherapeutic support remotely.
The identification of genetic pathways and specific genes involved in aging opens up the possibility of developing pharmacological interventions to target these pathways. Researchers are actively investigating compounds that can modulate these pathways, such as senolytics that selectively eliminate senescent cells, or drugs that mimic the effects of caloric restriction or activate sirtuins. These interventions aim to slow down the aging process, delay the onset of age-related diseases, and ultimately extend healthy lifespan. While much more research is needed to validate the safety and efficacy of these interventions in humans, the potential is promising [3].
Longitudinal studies tracking the long-term outcomes of different therapeutic modalities are necessary to assess their sustained effectiveness and potential for relapse prevention. Cultural factors, including language, beliefs, and attitudes towards mental health, influence treatment preferences and outcomes. Culturally sensitive approaches are essential for providing effective care. Geriatric depression often coexists with other medical and psychological conditions. Treatment plans should address these comorbidities to ensure comprehensive care. Clinical trials evaluating the effectiveness of therapeutic modalities should include diverse older adult populations, considering factors such as ethnicity, gender, socioeconomic status, and cognitive function. Engaging family members and caregivers in treatment planning and support can enhance treatment adherence and overall wellbeing for older adults [4].
While a significant number of correlated and anti-correlated dinucleotide pairs remained without such an explanation, we discovered that many of the observed correlations between dinucleotide contents could be the severe depression where individuals may lack capacity to make treatment decisions, ethical considerations surrounding decision-making and the use of interventions like ECT warrant careful attention. The comparative effectiveness of therapeutic modalities for geriatric depression is a multifaceted topic that necessitates a comprehensive and individualized approach. Psychotherapy, pharmacotherapy, and alternative interventions each have their strengths and limitations, and the optimal treatment plan depends on factors such as the severity of depression, patient preferences, safety considerations, and access to care. As the field of mental health continues to evolve, ongoing research, advancements in technology and a deeper understanding of the aging population's needs will shape the future landscape of geriatric depression treatment. Ultimately, the goal is to provide holistic, patient-centred care that improves the quality of life for older adults facing the challenges of depression [5].
As the field of longevity and genetics advances, ethical considerations come into play. The prospect of extending human lifespan raises questions about resource allocation, social inequality, and the impact on population dynamics. It is crucial to navigate these ethical considerations thoughtfully and ensure that the benefits of lifespan extension are accessible to all, promoting equitable and inclusive approaches to healthy aging [6].
Conclusion
The comparative effectiveness of therapeutic modalities for geriatric depression is a complex issue that requires a nuanced approach. Psychotherapy, pharmacotherapy, and alternative interventions each offer unique benefits, and the best approach often involves tailoring treatments to individual needs and preferences. A comprehensive understanding of the available options and their associated benefits and risks is essential for healthcare professionals aiming to provide optimal care for geriatric individuals struggling with depression. Additionally, ongoing research and advancements in treatment modalities will continue to shape the landscape of geriatric depression management, ultimately improving the quality of life for older adults around the world.
Acknowledgement
None.
Conflict of Interest
None.
References
- Yoo HH, Nunes-Nogueira VS, Boas PJ, Broderick C. Outpatient vs. inpatient treatment for acute pulmonary embolism. Cochrane Database Syst Rev 2022(5).
- Konstantinides SV. Chronic thromboembolic disease following pulmonary embolism: More work ahead. Eur Respir J 2020; 55(4).
- Højen AA, Søgaard M, Melgaard L, Lane DA, Sørensen EE, Goldhaber SZ, et al. Psychotropic drug use following venous thromboembolism versus diabetes mellitus in adolescence or young adulthood: A Danish nationwide cohort study. BMJ open 2019; 9:026159.
- Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders.
- Wohlfender, F. International online survey to assess current practice in equine anaesthesia. J Equine Vet 2015; 47:65-71.
- Dancker C. Effects of dobutamine, dopamine, phenylephrine and noradrenaline on systemic haemodynamics and intestinal perfusion in isoflurane anaesthetised horses. Equine Vet J 2018; 50:104-10.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Adewale T (2023) Comparative Effectiveness of Therapeutic Modalities for Geriatric Depression. J Gerontol Geriatr Res. 12: 687.
Copyright: © 2023 Adewale T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.