Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 0, Issue 0
Cavernous Hemangioma (Vascular Tumour) of Submandibular Salivary Gland in an Adult: A Rare Incidence
Pankaj Goyal1*, Kishan Kumawat1, Gajendra Nath Gupta2 and Nidhi P. Chanchlani22Department of Pathology, Reliable Diagnostic centre, Jaipur, Rajasthan, India
Received: 18-Jun-2023, Manuscript No. JVMS-23-21898; Editor assigned: 20-Jun-2023, Pre QC No. JVMS-23-21898 (PQ); Reviewed: 04-Jul-2023, QC No. JVMS-23-21898; Revised: 11-Jul-2023, Manuscript No. JVMS-23-21898 (R); Published: 21-Jul-2023, DOI: 10.35248/2329-6925.23.S16.516
Abstract
Because cavernous hemangiomas of the Sub-Mandibular Gland (SMG) are uncommon, there are few clinicoradiologic pathognomonic characteristics on which to base a diagnosis. Hemangioma diagnosis prior to surgery is therefore unusual. The distinguishing clinical characteristic of cavernous hemangiomas involving the SMG is a fluctuant swelling that is unrelated to dietary intake. Similar signs and symptoms can be seen in both sialolithiasis and chronic sialadenitis. On a Computed Tomography (CT) scan, cavernous hemangiomas appear as cystic or enhancing lesions, either with or without calcification; however, this is not a pathognomonic finding for diagnosis. Typically, spontaneous regression does not occur in cavernous hemangiomas. So, surgical excision is the choice of treatment. We present an adult in this case report who underwent successful surgical excision for a cavernous hemangioma of the submandibular gland.
Keywords
Cavernous hemangioma; Adult; Submandibular salivary gland; CT scan; Surgical excision
Introduction
During infancy and early childhood, hemangiomas are the most prevalent tumours discovered in the major salivary glands [1]. But they rarely affect adults’ major salivary glands, and submandibular involvement is particularly uncommon [2]. The symptoms of submandibular hemangioma are frequently confused with those of submandibular sialadenitis due to their anatomic location. Furthermore, hemangiomas in the submandibular gland are frequently misdiagnosed by radiologists as mucoceles or sialadenitis with calculi [3]. The rarity of hemangiomas involving the submandibular gland and their peculiar presentation make it typical for preoperative diagnoses to be incorrect and for treatment regimens to be inappropriate. When submandibular gland hemangiomas do develop, they typically take the form of an asymptomatic cystic mass that frequently extends beyond the ramus of the mandible. On palpation, some of these tumours feel firm while others seem spongy. The diagnosis is established through clinical examination and radiologic analysis. The preferred method of treatment is surgical excision. Here, we present a rare instance of a cavernous hemangioma that affected an adult’s submandibular gland.
Case Presentation
Thirty-five years old female patient attended our Apollo ENT hospital, Jodhpur, Rajasthan, for left sided neck swelling since four to five years. This swelling progressed gradually and attained present size. She had no history of any addiction. There was no history of odynophagia, dysphagia, fever, or changes in voice. She was treated medically by family doctor but did not get relief. There was a history of incision and drainage in view of suspicion of abscess two years back. On clinical examination, there was a 3.5 × 2 cm swelling at the left submandibular region with scar over it (Figure 1). It was soft, cystic, fluctuant and non-tender. There was no dilated vein or sinuses over the swelling. Skin over swelling was pinchable. Bimanual palpation there was no intraoral extension. A Computed Tomography (CT) scan revealed 4.2 cm × 4.5 cm calcification foci inside the larger left submandibular gland with modest enhancement (Figure 2A, B and C). The patient underwent fine-needle aspiration, but the results of the cytological analysis were not diagnostic since the specimen had an excessive amount of red blood cells. General anaesthesia was used for the patient’s left Sub- Mandibular Gland (SMG) excision after the patient’s condition was conveyed to them and their consent was obtained. At the level of 2 cm below the angle of the jaw, a neck skin crease incision on the left side was made. The subplatysmal flap was raised. The marginal mandibular nerve was precisely located and protected. Facial vessels were identified and ligated. Intraoperatively, the SMG was detached from the surrounding mylohyoid muscle (Figure 3 and Figure 4). The lingual and hypoglossal nerves were spared. The SMG duct was identified and ligated (Figure 5). The main surgical specimen was removed completely and sent for histopathology. After attaining hemostasis, the surgical incision was closed in layers. After a successful extubation, the patient was transferred to the recovery room. The intravenous antibiotic was given for next two days. Histopathology report revealed it as large dilated bloodfilled sinus like spaces with thick walls of fibromuscular tissue lined, by flat endothelial cells. The sinus like muscular spaces inter connect with each other. Overall histomorphology is consistent with cavernous (venous) hemangioma. Patient was doing well with no recurrence during one year regular follow up.
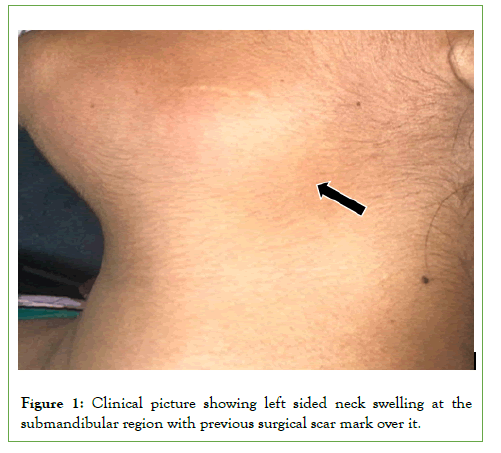
Figure 1:Clinical picture showing left sided neck swelling at the submandibular region with previous surgical scar mark over it.
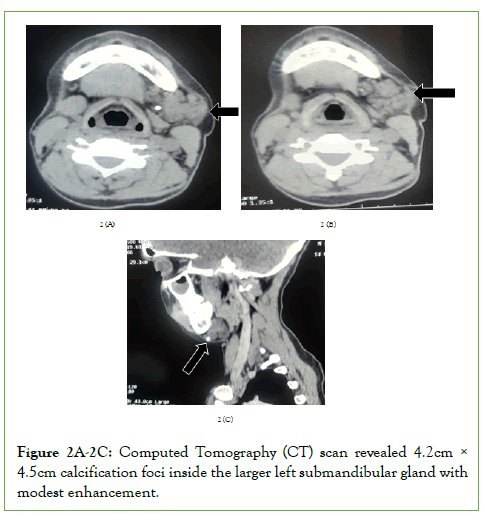
Figure 2A-2C: Computed Tomography (CT) scan revealed 4.2cm Ã? 4.5cm calcification foci inside the larger left submandibular gland with modest enhancement.
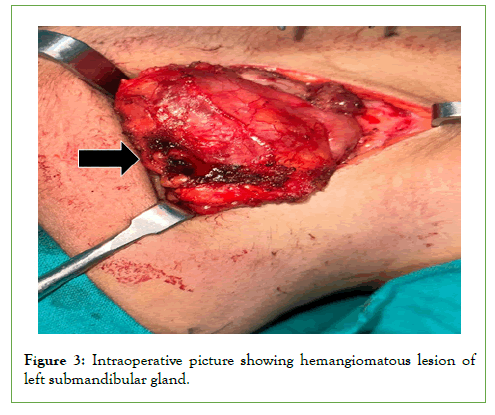
Figure 3: Intraoperative picture showing hemangiomatous lesion of left submandibular gland.
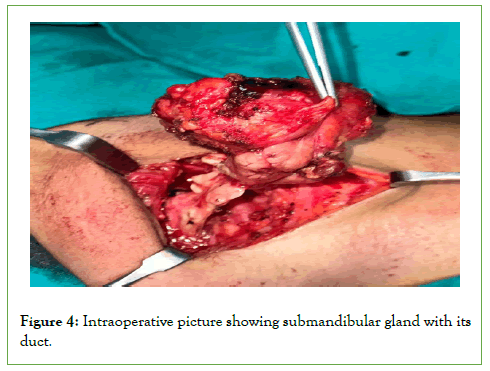
Figure 4: Intraoperative picture showing submandibular gland with its duct.
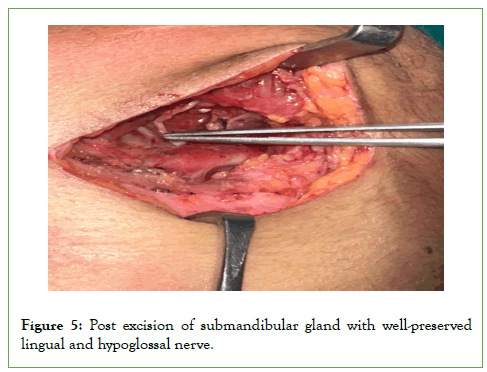
Figure 5: Post excision of submandibular gland with well-preserved lingual and hypoglossal nerve.
Results and Discussion
Vascular tumors arising in the major salivary glands are almost always hemangiomatous, rarely malignant, and most common in the parotid glands of newborns and infants [4-6]. Adults seldom develop hemangiomas involving the major salivary glands, and when they do, they tend to affect the parotid gland more frequently (87.5%) than the submandibular gland (12%) (Figure 6) [1]. The majority of submandibular gland hemangiomas show as an asymptomatic cystic mass when they do arise.
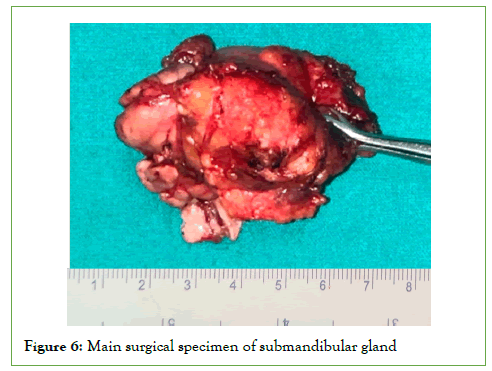
Figure 6: Main surgical specimen of submandibular gland.
There are two types of hemangiomas: Capillary and cavernous. The cavernous form is characterized by dilated, thin-walled, blood-filled vascular areas that are lined by noticeably flattened endothelial cells (Figure 7A, B and C). The vessels may be set up in a loosely lobular pattern or in a random, dispersed pattern. Occasionally, adventitial fibrosis causes the walls to thicken, and the stroma may contain inflammatory cells that are dispersed throughout the tissue [7]. The vascular findings in our patient’s pathologic report were big, dilated, blood-filled arteries lining lobular-shaped flattened endothelium.
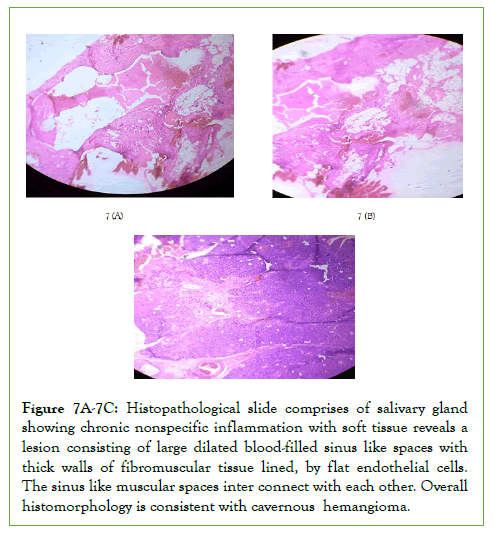
Figure 7A-7C: Histopathological slide comprises of salivary gland showing chronic nonspecific inflammation with soft tissue reveals a lesion consisting of large dilated blood-filled sinus like spaces with thick walls of fibromuscular tissue lined, by flat endothelial cells. The sinus like muscular spaces inter connect with each other. Overall histomorphology is consistent with cavernous hemangioma.
The average patient with a hemangioma is 10 years old, and around 90% of all hemangiomas develop within the first three decades of life; however, cavernous hemangiomas, like the one in this example, often develop in older kids and adults [7,8]. 20 individuals with cavernous hemangiomas of the parotid gland were evaluated by Nagao, et al. in their study [9]. They discovered that the average age was 26 years old (with a range of 4 months to 50 years). This result was supported by our patient’s age.
Hemangiomas can develop from the gland itself, or they can develop as a result of subcutaneous blood vessels invading the gland structure [10]. Hemangiomas in the submandibular gland are uncommon, making it challenging to detect them when there are no cutaneous changes on the surface.
Hemangiomas in the submandibular gland develop later in life than those in the parotid gland and are twice as common in women as in men because they are affected by circulating hormones [3]. Our patient’s sex was consistent with these findings.
It is crucial to confirm a diagnosis through clinical evaluation and radiologic studies. The lack of any diagnostic hints makes submandibular gland hemangiomas particularly challenging to diagnose. The clinical characteristics of hemangiomas in the submandibular gland have not, as far as we are aware, been the subject of any studies.
In an effort to characterize the radiologic characteristics connected to cavernous hemangiomas affecting the submandibular gland, several groups have made their efforts. Magnetic resonance imaging, according to Odabasi et al, can display focal heterogeneities that signify areas of thrombosis, fibrosis, or calcification [11].
Some people contend that the existence of a colour Doppler signal in a hyperechoic mass with a heterogeneous echo structure on sonography indicates the presence of a hemangioma [12]. Cho, et al. proposed that calcified nodules on CT scans are pathognomonic for the diagnosis of cavernous hemangioma [13].
Due to modifications in blood flow dynamics within the hemangioma, calcification happens after thrombus and phlebolith development [1]. To rule out sialadenitis with sialoliths and other benign or malignant tumours, differential diagnoses of cystic or enhancing lesions in the submandibular triangle with or without calcification are required. Other benign or malignant tumours do not present with fluctuant swelling, whereas sialadenitis with sialoliths can cause submandibular gland swelling related to food consumption. As previously stated, cavernous hemangiomas have a tendency to fluctuate in size and their swelling is not related to food intake.
Sometimes it can be difficult to tell a second branchial cleft cyst from a plunging ranula in the submandibular area. In order to distinguish between the two, a careful evaluation of the cystic mass’s position in respect to the sub-mandibular gland may be beneficial [14]. If a vascular lesion is seen on imaging but fineneedle aspiration is inconclusive, a hemangioma should be considered in the differential diagnosis. It is difficult to diagnose a cavernous hemangioma with fine-needle aspiration cytology. Most cavernous hemangiomas need to be treated since they have a tendency to be more severe and poorly defined than capillary and juvenile hemangiomas and don’t resolve easily. The most effective treatment is complete surgical excision. The literature also lists vascular ligation, cryosurgery, sclerosing injections, and laser ablation as additional therapy options.
Conclusion
Cavernous hemangiomas rarely occur in the submandibular region. Doctors frequently misdiagnose it as sialolithiasis due to the clinical and radiologic characteristics. A swelling in the submandibular region should be evaluated for cavernous hemangiomas with phleboliths. The most effective treatment is complete surgical excision.
Compliance with ethical standards
The procedure performed in this case report was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This study is not funded by any resources.
Conflict of Interest
The author’s declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.
Ethical Approval
The study was published with the written consent of the patient.
References
- Chuang CC, Lin HC, Huang CW. Submandibular cavernous hemangiomas with multiple phleboliths masquerading as sialolithiasis. J Chin Med Assoc. 2005;68(9):441-443.
[Crossref] [Google Scholar] [Pub Med]
- Elâ?Hakim IE, Elâ?Khashab MM. Cavernous haemangioma of the submandibular salivary gland. Int J Oral Maxillofac Surg. 1999;28(1):58-59.
[Crossref] [Google Scholar] [Pub Med]
- Cho JH, Nam IC, Park JO, Kim MS, Sun DI. Clinical and radiologic features of submandibular triangle hemangioma. J Craniofac Surg. 2012;23(4):1067-1070.
[Crossref] [Google Scholar] [Pub Med]
- Kauffman SL, Stout AP. Tumors of the major salivary glands in children. Cancer. 1963;16(10):1317-1331.
[Crossref] [Google Scholar] [Pub Med]
- Goldman RL, Perzik SL. Infantile hemangioma of the parotid gland: A clinicopathological study of 15 cases. Arch Otolaryngol. 1969;90(5):605-608.
[Crossref] [Google Scholar] [Pub Med]
- Williams HB. Hemangiomas of the parotid gland in children. Plast Reconstr Surg. 1975;56(1):29-34.
[Crossref] [Google Scholar] [Pub Med]
- McMenamin M, Quinn A, Barry H, Sleeman D, Wilson G, Toner M. Cavernous hemangioma in the submandibular gland masquerading as sialadenitis: Case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(2):146-148.
[Crossref] [Google Scholar] [Pub Med]
- Stratiev A. Hemangioma of the submandibular gland. Stomatologiia (Sofiia). 1973;55(6):464-467.
- Nagao K, Matsuzaki O, Shigematsu H, Kaneko T, Katoh T, Kitamura T. Histopathologic studies of benign infantile hemangioendothelioma of the parotid gland. Cancer. 1980;46(10):2250-2256.
[Crossref] [Google Scholar] [Pub Med]
- El-Khashab MM, El-Kafrawy AH, El-Shalaby N. Hemangiomas of the parotid gland. Egypt Dent J. 1972;18(2):189-200.
- Kumar S, Gupta AK, Bakshi J. Submandibular gland hemangioma: Clinicopathologic features and a review of the literature. Ear Nose Throat J. 2010;89(11):E14-E17.
[Crossref] [Google Scholar] [Pub Med]
- Odabasi AO, Metin KK, Mutlu C, Basak S, Erpek G. Intramuscular hemangioma of the masseter muscle. Eur Arch Otorhinolaryngol. 1999;256:366-339.
[Crossref] [Google Scholar] [Pub Med]
- Yang WT, Ahuja A, Metreweli C. Sonographic features of head and neck hemangiomas and vascular malformations: Review of 23 patients. J Ultrasound Med. 1997;16(1):39-44.
[Crossref] [Google Scholar] [Pub Med]
- Ozturk M, Sari F, Erdogan S, Mutlu F. Submandibular cystic cavernous hemangioma: An unusual presentation. J Craniofac Surg. 2013;24(5):1856-1857.
Citation: Goyal P, Kumawat K, Gupta GN, Chanchlani NP (2023) Cavernous Hemangioma (Vascular Tumour) of Submandibular Salivary Gland in an Adult: A Rare Incidence. J Vasc Surg. S16:516.
Copyright: © 2023 Goyal P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

