Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
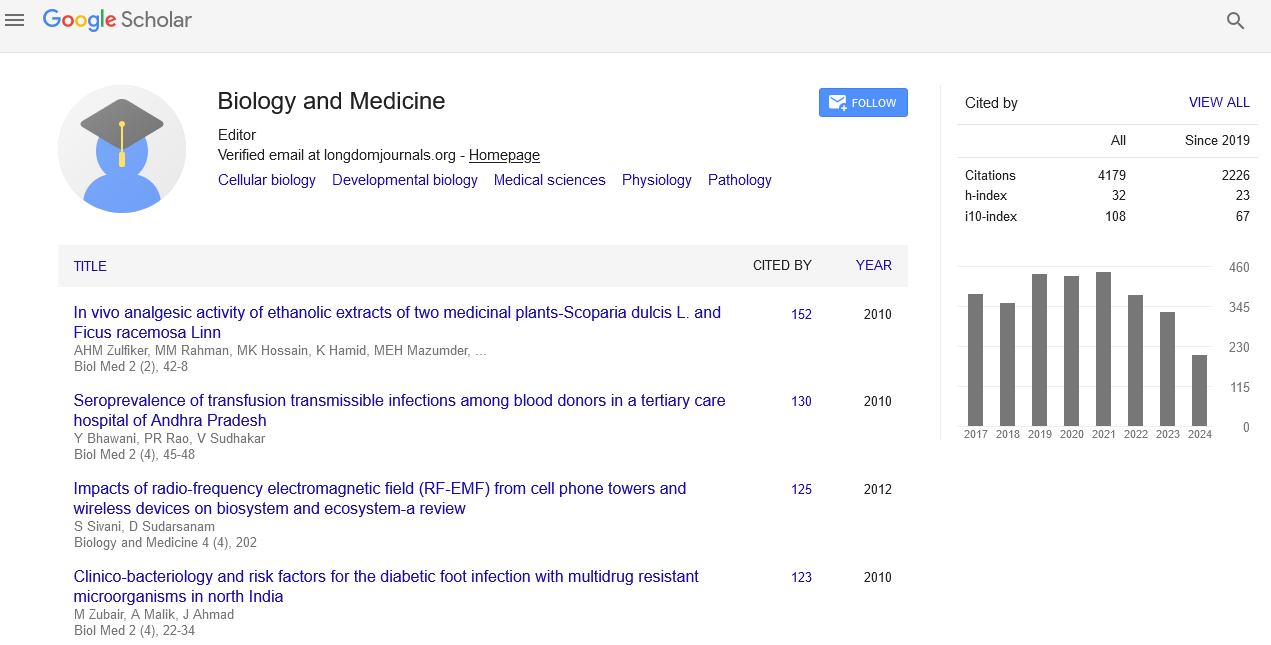
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 14, Issue 11
Causes, Symptoms and Diagnosis of Intestinal Ischemia
Muluken Gizaw*Received: 20-Oct-2022, Manuscript No. BLM-22-18733; Editor assigned: 24-Oct-2022, Pre QC No. BLM-22-18733(PQ); Reviewed: 07-Nov-2022, QC No. BLM-22-18733; Revised: 14-Nov-2022, Manuscript No. BLM-22-18733(R); Published: 21-Nov-2022, DOI: 10.35248/0974-8369.22.14.519
Description
Intestinal ischemia describes a variety of conditions that occur when blood flow in a person to intestine decreases. Ischemia can be due to a fully or partially blocked blood vessel, usually an artery or low blood pressure leading to an overall reduced blood flow. Intestinal ischemia can affect small intestine, large intestine (colon) or both. The decreased blood flow doesn't provide enough oxygen for the cells in a person’s digestive system. Intestinal ischemia is a serious condition that can cause severe pain and make it difficult for a person’s intestine to work properly. In severe cases, loss of blood flow to the intestines can damage intestinal tissue and even sometimes leads to death.
Small intestinal ischemia (also called mesenteric ischemia) is a group of potentially life-threatening disorder that reduces blood flow to the superior mesenteric artery intestine includes duodenum, jejunum, ileum, etc. Symptoms range from mild to severe, depending up on the cause. If a person have severe stomach pain, early diagnosis and treatment are essential for the best possible results in the recovery of digestive function.
Intestinal ischemia can be classified into superior mesenteric artery intestinal ischemia, commonly known as mesenteric ischemia, and colonic ischemia, commonly known as Large intestine ischemia. Intestinal ischemia occurs when intestinal blood flow is reduced by at least 75% over a period of 12 hours or more. Abdominal pain is the most common symptom in people with intestinal ischemia. Intestinal ischemia can affect the superior mesenteric artery or large intestine and can occur for any reason, resulting in reduced blood flow to the intestine. This is a rare condition, but it has a high mortality rate.
The intestine is mainly supplied by two major arteries, including the superior and inferior mesenteric arteries. The superior mesentery supplies the blood to intestine from the lower duodenum to colon. The inferior mesenteric artery supplies the blood from large intestine to the colon is susceptible to ischemia, including the flexure of the splenic flexure (Griffith's point) and the recto sigmoid junction (Sudek's point). These are also known as "watersheds" and refer to the areas within the colon between the two major arteries that supply blood to the colon. The splenic flexure is the area between the superior and inferior mesenteric arteries, and the sigmoid rectum is the area between the two major arteries that supply the inferior and superior mesenteric arteries. However, in 50% of the population, this artery is underdeveloped. Watersheds account for approximately 70% of ischemic colitis cases. Venous outflow of the large intestine occurs in parallel with the arterial supply. The superior mesenteric vein drains the area supplied by the superior mesenteric artery, and the inferior mesenteric vein drains the left side of the colon and rectum. Acute reduction in mesenteric artery blood flow is responsible for 60%-70% of patients with mesenteric ischemia. The remaining causes are related to colonic ischemia. Abdominal pain is the most common symptom in patients suffering with intestinal ischemia. Several patient characteristics help to distinguish between acute intestinal ischemia and colonic superior mesenteric artery ischemia. Patient characteristics such as age 60 years or older, no serious medical conditions, mild abdominal pain, tenderness, rectal bleeding, and bloody diarrhoea are more common features of acute colonic ischemia. Computed tomography of the abdomen is commonly used in hemodynamically stable patients with acute abdominal pain. Computed tomography is the first examinations in patients with high suspicion of intestinal ischemia. Different drug treatments have been proposed based on subtypes of acute mesenteric ischemia. Papaverine can be given through angiographic catheters in all arterial forms and in the relaxation mechanism of vasospasm in non-occlusive mesenteric ischemia.
Necrosis of the mucosal villi is the first change and usually occurs within 3-4 hours of intestinal ischemia. This can leads to transmural, mural, or mucosa infarction. Splenic flexure and rectal sigmoid junction are often prone to decreased blood flow and hypoxia. The first reaction to an injury is an obstruction of the intestinal wall. It then appears to be edematous, fragile, and hemorrhagic. Without intervention, bowel bleeding can occur within 1 to 4 days. The gut bacteria then cause intestinal gangrene and perforation.
Citation: Gizaw M (2022) Causes, Symptoms and Diagnosis of Intestinal Ischemia. Bio Med. 14:519.
Copyright: ©2022 Gizaw M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.