Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2024) Volume 16, Issue 8
Caught in the Crossfire- A Case of Anti GBM Disease with Rapid Renal Decline
Ishana Gaur*Received: 31-Jul-2024, Manuscript No. BLM-24-26935; Editor assigned: 02-Aug-2024, Pre QC No. BLM-24-26935 (PQ); Reviewed: 16-Aug-2024, QC No. BLM-24-26935; Revised: 23-Aug-2024, Manuscript No. BLM-24-26935 (R); Published: 30-Aug-2024, DOI: 10.35248/0974-8369.24.16.722
Abstract
Background: Anti-Glomerular Basement Membrane (Anti-GBM) disease is a rare autoimmune disorder that primarily affects the kidneys and less commonly, the lungs. The rapid progression of glomerulonephritis is an important feature of this disease, leading to significant renal damage if not treated promptly. Early diagnosis and treatment are essential to preventing irreversible kidney injury.
Case Description: We report a case of a 45-year-old male who presented with 15 days of hematuria and 2 days of breathlessness. The patient had no history of hypertension or diabetes. Clinical examination revealed pallor, high blood pressure and fine crepitations in bilateral lower lung fields. Laboratory investigations showed elevated serum creatinine, reduced hemoglobin and significant proteinuria. Anti-GBM antibodies were markedly elevated and a kidney biopsy confirmed the diagnosis of crescentic glomerulonephritis with a necrotizing pattern. The patient was treated with plasmapheresis, steroids and cyclophosphamide, along with maintenance hemodialysis. Despite the aggressive nature of the disease, early intervention helped stabilize his renal function.
Conclusion: This case highlights the importance of rapid diagnosis and prompt initiation of aggressive treatment in patients with anti-GBM disease presenting as rapidly progressive glomerulonephritis. Early intervention is a key to preserving renal function and improving patient outcomes.
Keywords
Anti-GBM disease; Rapidly progressive glomerulonephritis; Crescentic glomerulonephritis; Plasmapheresis; Autoimmune nephritis
Introduction
Anti-Glomerular Basement Membrane (anti-GBM) disease is a rare but serious autoimmune disorder that predominantly targets the kidneys and in some cases, the lungs. This condition is characterized by the rapid onset of glomerulonephritis, leading to significant kidney damage if left untreated. Early diagnosis and swift medical intervention are essential to prevent irreversible renal injury. This report presents a case of a 45-year-old male diagnosed with anti-GBM disease, emphasizing the need for immediate recognition and treatment to preserve kidney function.
Case Description
A 45-year-old male presented to the emergency department with complaints of red urine for 15 days and breathlessness for 2 days. The patient reported no associated fever, pain or dysuria with the hematuria. His breathlessness was not accompanied by orthopnea, cough or edema. He also experienced vomiting for 2 days. The patient had no prior history of hypertension, diabetes, or similar illness in his family [1].
Upon physical examination, the patient was pale, with a pulse rate of 100/min and blood pressure of 170/98 mmHg. Fine crepitations were heard in the lower lung fields bilaterally. Heart sounds were normal, and the abdomen was soft and non-tender. Neurologically, the patient was alert and oriented. Review of other systems was unyielding (Figures 1 and 2).
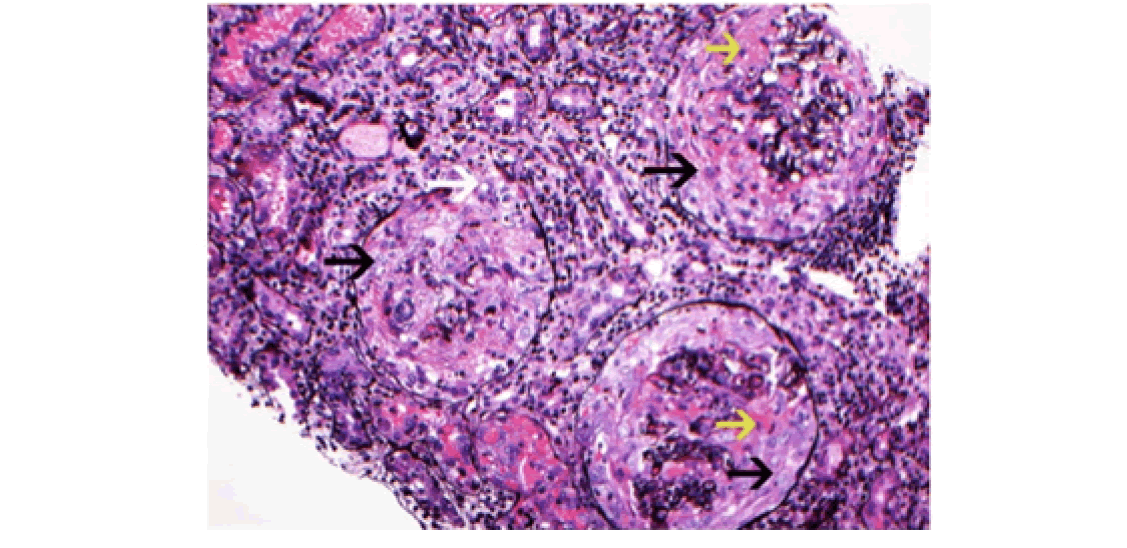
Figure 1: Silver stain showing with large circumferential cellular crescents with necrosis. Note: Disruption of Bowman’s capsule. There is prominent
interstitial inflammation present. Red Blood Cells (RBC) are present in tubules. ( ) at cellular crescents, (
) at cellular crescents, ( ) points at Fibrinoid necrosis) and
(
) points at Fibrinoid necrosis) and
( ) points at disruption of Bowman’s capsule, Jones silver methanamine stain 200X).
) points at disruption of Bowman’s capsule, Jones silver methanamine stain 200X).
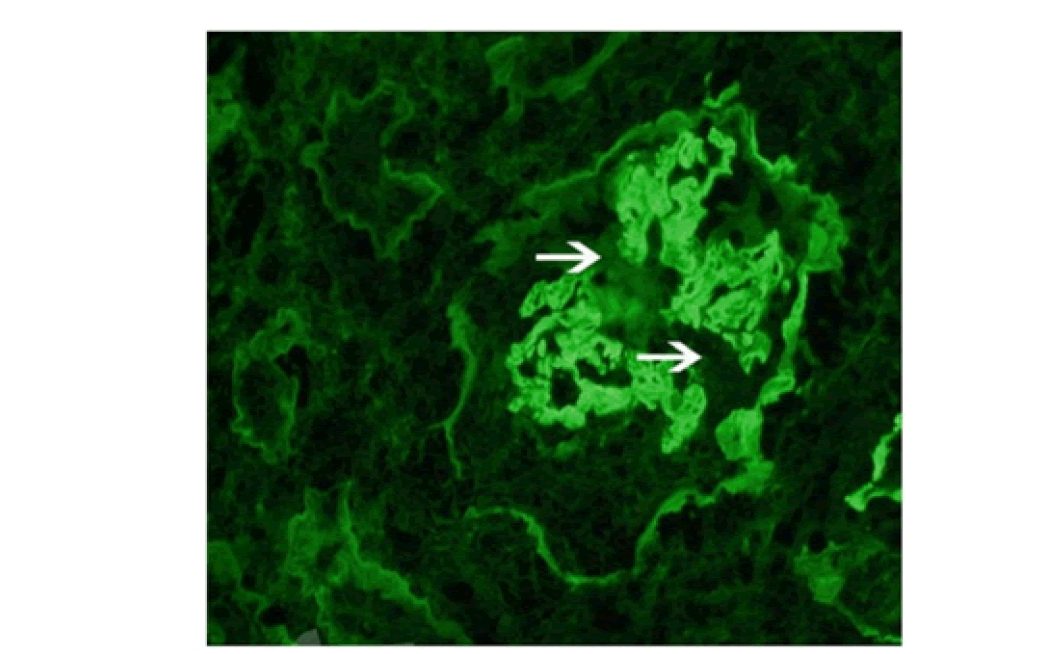
Figure 2: Immunofluorescence microscope showing linear staining for anti Ig-G along the glomerular capillary walls. Note: Disruption of the linear
staining necrosis/crescent. ( ) represents disruption 400X.
) represents disruption 400X.
Laboratory findings were significant for severe anemia (hemoglobin: 7 g/dl), elevated serum urea (274 mg/dl), serum creatinine (14.8 mg/ dl) and hyperkalemia (serum potassium: 7 mEq/l). Urinalysis showed 500 RBCs/HPF and proteinuria of 300 mg/dl. The urine protein- creatinine ratio was 650 mg/g of creatinine.
Further investigations revealed elevated anti-GBM antibodies (55 U/ ml, normal <20 U/ml), and a kidney biopsy confirmed crescentic glomerulonephritis with a necrotizing pattern. Immunofluorescence showed linear staining for IgG along the glomerular basement membrane. perinuclear Anti-Neutrophil Cytoplasmic Antibodies (pANCA) and cANCA (cytoplasmic Anti-Neutrophil Cytoplasmic Antibodies (cANCA) were negative.
The patient was diagnosed with renal-limited anti-GBM disease, treated with plasmapheresis, intravenous corticosteroids, cyclophosphamide and maintenance hemodialysis.
Results and Discussion
Anti-Glomerular Basement Membrane (anti-GBM) disease, also known as Goodpasture syndrome when the lungs are involved, is a rare autoimmune disorder. It is caused by the generation of circulating auto-antibodies that attack the non-collagen part of the alpha 3 chain of the type IV collagen. These antibodies are targeted against the glomerular and the alveolar basement membranes leading to a rapidly progressive glomerulonephritis and at times pulmonary haemorrhage [2,3].
Pathogenetic factors are related to both genetics and environmental influences. It has high correlation with particular HLA class II molecules such as HLA-DR15 and HLA-DR4 that are presumed to present collagen derived peptide to T cells leading to production of pathogenic antibodies. Several environmental factors such as smoking, viral infections and hydrocarbon exposure can also act as disease promoters, aggravating the immune response. Although, there was no clear environmental eliciting factor in this case, smoking is often associated with higher risk of pulmonary hemorrhages in anti-GBM patients [4]. Clinical presentation is characterized by rapidly progressive glomerulonephritis. The renal changes are usually the most pronounced, frequently resulting in hematuria, proteinuria and in severe renal failure. Histopathological examination reveals presence of crescentric glomerulonephritis, a key feature of severe glomerular injury. Immunoflorescence studies show a picture of linear deposition of IgG class of antibodies along the glomerular basement membrane. This finding is highly suggestive of anti GBM disease. These crescents compress the glomerular capillary tuft, leading to glomerular necrosis and irreversible renal damage if left untreated. In this case, the patient presented with a classic feature of anti-GBM disease -hematuria and rapidly progressive renal failure. His elevated serum creatinine, significant proteinuria, and positive anti-GBM antibodies confirmed the diagnosis. Crescentic glomerulonephritis was identified on kidney biopsy, further supporting the diagnosis [5]. Pulmonary involvement although absent in this case is an important aspect of this disease. Clinical presentation of hemoptysis, dyspnea or diffuse pulmonary infiltrates on chest imaging should prompt a suspicion of pulmonary hemorrhage. The disease has a strong predilection for smokers. Younger male smokers appear to be at higher risk. This kind of pulmonary involvement was not present in this case and this spared the patient from more respiratory symptoms although renal damage was massive.
In anti-GBM disease urgent management is important, intensive and early treatment is required to prevent organ losses that are beyond salvageable. Plasmapheresis is a proven method, useful in circulation of anti-GBM antibodies removal from the bloodstream. High-dose corticosteroids are given to the patient concomitantly to control the inflammatory response while cytotoxics like cyclophosphamide are used to prevent new antibodies from being generated [6].
Despite these available therapies that are provided, the outcome is still dismal for patients who present with severe renal failure. In this particular case, the patient’s creatinine levels at time of presentation were markedly elevated and the patient was started on dialysis. For these patients with such severe kidney injury, recovery of kidney function to normal is often a farfetched dream, dialysis is inevitable and/or renal transplant is required emergently or later on. The most important determinant for predicting outcomes is the promptness of diagnosis and initiation of treatment. Several studies show that patients who receive early treatment preferably before the dependence of dialysis sets in, tends to have better outcomes than those who do not. Time is Kidney! Patients who present later in the course of disease tend to perform worse with regards to both short term and long term outcomes. They frequently become dialysis dependent even if aggressive immunosupression is started. The rapidity and severity of this disease is attributable to formation of large crescents in the glomeruli, which at first are cellular but later, can become fibrous and lead to scarring in kidneys and the disease process becomes irreversible at this stage. Cellular crescents are made of proliferating epithelial cells and macrophages which lead to destruction of glomerular basement membrane and the classical clinical features.
Strangely, the existence of anti-Glomerular Basement Membrane (anti- GBM) antibodies has also been linked to other autoimmune disorders such as ANCA-associated vasculitis. About 10% of persons diagnosed with anti-GBM disease are identified as ‘double-positive’ because those patients test both anti-GBM and Anti-Neutrophil Cytoplasmic Antibodies (ANCA). These patients are clinically inclined to be more vasculitis-like, making them more responsive to treatment than those who have anti-GBM disease only. However, this patient was also ANCA- negative and during the course of illness the patient had more typical isolated anti-GBM disease with severe renal involvement. As discussed earlier, the degree of renal failure at diagnosis is the most important determinant for predicting outcomes. Patients who present with high serum creatinine levels or require dialysis will have a lower rate of renal recovery. Patients with serum creatinine levels above 5.7 mg/dl or those requiring dialysis at presentation have a poorer prognosis, with a high likelihood of progressing to End-Stage Renal Disease (ESRD) despite treatment. The presence of pulmonary hemorrhage especially among the active smokers is another important predictor of poor prognosis.
Conclusion
In summary, anti-GBM disease remains a diagnostic and therapeutic challenge because of its rapid clinical onset and the high degree of potential of irreversible organ damage. Timely identification and treatment are necessary to achieve favorable outcomes. Early intervention with plasmapheresis, immunosuppressive therapy and supportive care remains the essential aspect of management in these cases, with the goal of preserving renal function and improving long- term outcomes. However, as exemplified by the case above, even with treatment the prognosis remains poor in patients who present late or with significant renal involvement. Further research is much needed to better management of this deadly disease.
References
- McAdoo SP, Pusey CD. Anti-Glomerular Basement Membrane (aGBM) disease. Clin J Am Soc Nephrol. 2017;12(7):1162-1172.
- Biesenbach P, Kain R, Derfler K, Perkmann T, Soleiman A, Benharkou A, et al. Long-term outcome of anti-glomerular basement membrane antibody disease treated with immunoadsorption. PLoS One. 2014;9(7):103568.
[Crossref] [Google Scholar] [PubMed]
- Hellmark T, Segelmark M. Diagnosis and classification of Goodpasture's disease (anti-GBM). J Autoimmun. 2014;48:108-112.
[Crossref] [Google Scholar] [PubMed]
- George MG. Risk factors for ischemic stroke in younger adults: A focused update. Stroke. 2020;51(3):729-735.
- Kluth DC, Rees AJ. Anti-glomerular basement membrane disease. J Am Soc Nephrol. 1999;10(11):2446-2453.
[Crossref] [Google Scholar] [PubMed]
- Alchi B, Griffiths M, Sivalingam M, Jayne D, Farrington K. Predictors of renal and patient outcomes in anti-GBM disease: clinicopathologic analysis of a two-centre cohort. Nephrol Dial Transplant. 2015;30(5):814-821.
[Crossref] [Google Scholar] [PubMed]
Citation: Ishana Gaur (2024). Caught in the Crossfire- A Case of Anti GBM Disease with Rapid Renal Decline. Bio Med. 16:722.
Copyright: © 2024 Gaur I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


