Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
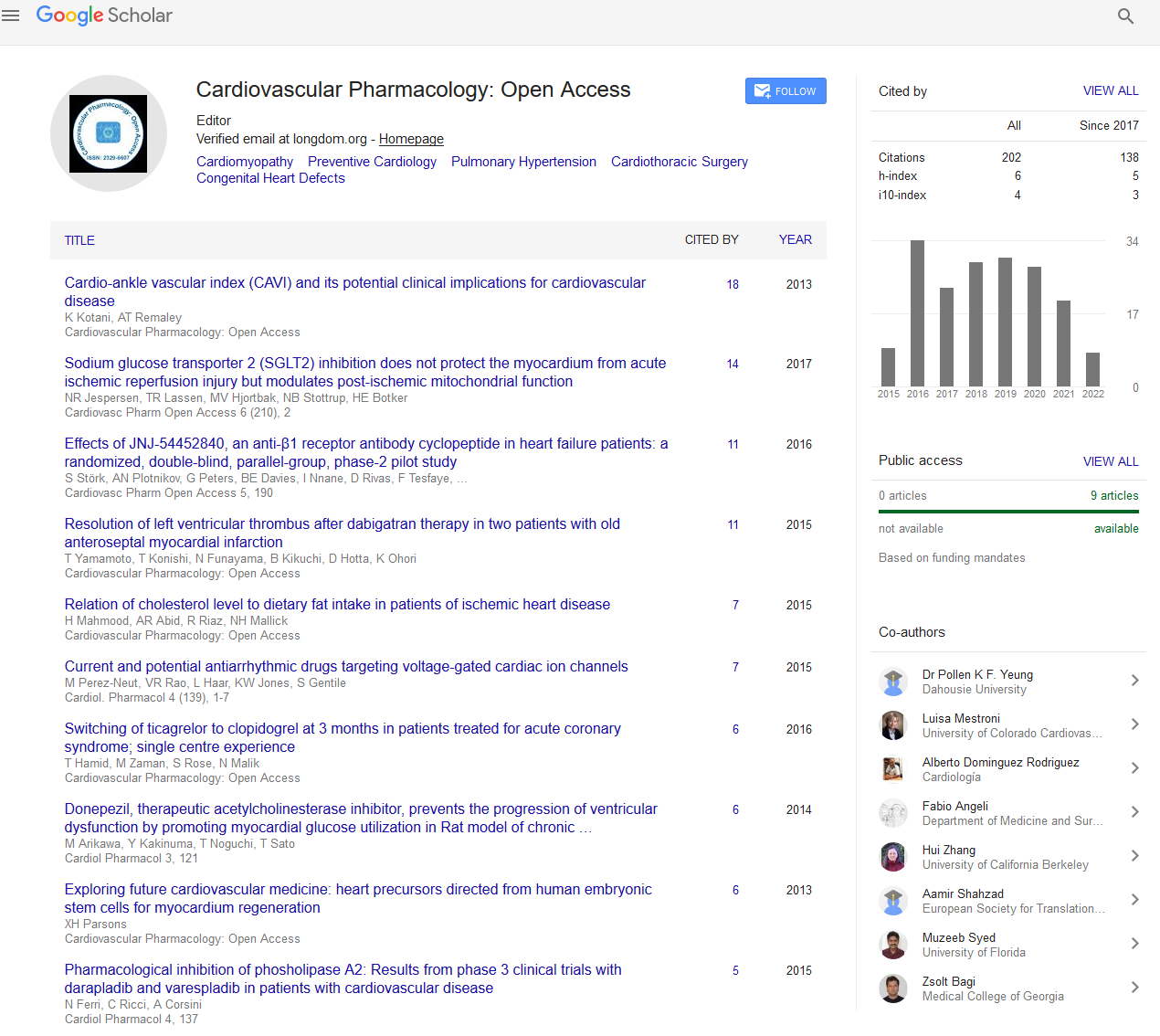
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 11, Issue 8
Cardiac Catheterization in Patients with Coronary Artery Disease
Julius Grieben*Received: 08-Aug-2022, Manuscript No. CPO-22-17906; Editor assigned: 11-Aug-2022, Pre QC No. CPO-22-17906 (PQ); Reviewed: 25-Aug-2022, QC No. CPO-22-17906; Revised: 01-Sep-2022, Manuscript No. CPO-22-17906 (R); Published: 08-Sep-2022, DOI: 10.35248/2329-6607.22.11.297
Description
Recent developments in molecular methods and cardiological studies have improved our understanding of cardiac illness, a well-known consequence of myotonic dystrophy. In myotonic dystrophy, conduction abnormalities and tachyarrhythmias frequently develop. The most prevalent muscular dystrophy in adulthood, myotonic dystrophy (also known as dystrophia myotonica or Steinert's disease), is a multisystem condition with an incidence of 1 in 8000. Steinert defined the condition as a separate ailment in 1909, and it was in this pioneering study that cardiovascular involvement was initially proposed since bradycardia was recognised to be a characteristic of numerous patients. A hereditary condition known as Myotonic Dystrophy type 2 (DM2) is characterised by symptoms involving the skeletal muscles, metabolic abnormalities, and cardiac involvement. Fibrosis and fatty infiltration are examples of the skeletal muscle's histopathologic changes. The purpose of this study was to determine if cardiovascular magnetic resonance may already identify preclinical cardiac involvement in DM2 in patients with maintained left ventricular function.
Mbnl-deficient mice models mimic cardinal DM1 cardiac abnormalities and exhibit multiple splicing alterations, including events impacting sodium and calcium channels, which are consistent with the functional loss of MBNL proteins as a result of their sequestration by enlarged CUG repeats. The human DMPK gene with enlarged CTG repeats and improper SCN5A mRNA splicing were discovered in cardiac samples from DM1 patients by RNAseq, and abnormal sodium current characteristics were also connected with conduction deficits in a mouse model. The alpha-subunit of the cardiac voltage-gated sodium channel, Nav1.5, which is encoded by the SCN5A gene, is involved in the fast depolarization of cardiac cells, the length of the cardiac action potential, and the propagation of the impulse throughout the myocardium. Arrhythmic conditions including Brugada syndrome and autosomal dominant conduction system illness are caused by the loss of Nav1.5 function.
Most MD1 patients die from cardiac or respiratory problems. Sudden death is thought to be caused by ventricular arrhythmias or atrioventricular block. Recent research revealed that significant Electrocardiographic (ECG) abnormalities and atrial arrhythmias are independent risk factors for sudden death in MD1 patients, albeit with a modest sensitivity. Compared to individuals with other muscular dystrophies, death from progressive heart failure occurs less often in patients with MD1, although left ventricular systolic dysfunction is linked to a higher risk of overall mortality and sudden death. As a result, it becomes clear that individuals with MD1 have a complicated cardiac phenotype that includes both the myocardium and the conduction system. Given the significance of cardiomyopathy as a prognosis predictor, we sought to assess heart function and find structural abnormalities in MD1 patients. In the current study, we used Cardiovascular Magnetic Resonance (CMR) because it is a precise and highly reproducible method for determining cardiac volumes, function, mass, and focal fibrosis, and because it has superior interstudy reproducibility in normal, dilated, and hypertrophic hearts to 2-dimensional echocardiography.
The most common cardiac manifestation of DM1 is conduction system disease. When patients were diagnosed, first-degree atrioventricular, fascicular, or bundle branch blockages were present in 28%–45% of cases. Electrophysiological examinations of individuals with minor conduction problems on the surface ECG typically reveal infrahisian conduction deficiencies, with the HV interval highly associated with the PR interval and QRS widening. In addition, 55% of individuals with normal ECG results exhibited infrahisian conduction abnormalities. In a large cohort of unselected DM1 patients over the course of a 12-year follow-up (median age, 50 years), 19% of patients progressed to full atrioventricular block, and 55% of patients had an HV interval of less than 70 ms over the course of a 55-month followup. Age, male sex, atrial fibrillation, syncope, and the presence of any conduction deficit on the ECG are all independent predictors of progressive atrioventricular block. There have been a few cases of biventricular failure recorded without an arrhythmia, however it is difficult to determine whether this is due to myotonic dystrophy itself or a cardiomyopathy that occurs concurrently with the illness. Numerous researches have looked into the possibility of subclinical myocardial dysfunction. Even in the absence of coronary artery disease, the ECG frequently shows aberrant Q-waves and ST segments.
Citation: Grieben J (2022) Cardiac Catheterization in Patients with Coronary Artery Disease. Cardiovasc Pharm. 11:297.
Copyright: © 2022 Grieben J. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.