Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2022) Volume 8, Issue 2
Cannabinoid Association with Opioid in Cancer Pain Management Therapy: A Systematic Review
Helena Freitas*Received: 11-Mar-2022, Manuscript No. JPMME-22-15769; Editor assigned: 16-Mar-2022, Pre QC No. JPMME-22-15769 (PQ); Reviewed: 30-Mar-2022, QC No. JPMME-22-15769; Revised: 06-Apr-2022, Manuscript No. JPMME-22-15769 (R); Published: 13-Apr-2022, DOI: 10.35248/2684-1320.8.2.167
Abstract
Background: Cancer is the disease that causes the highest numbers of morbidity and mortality in the world, being one of the main symptoms chronic pain. Moderate and severe pain is usually treated with opioids, whose efficacy is proven but with several risks for the patient. Medical cannabis appears as a new hope for these patients. This study aims to understand whether the concomitant use of cannabinoids and opioids allows a more effective management of pain and reduce opioid use in cancer patients.
Methodology: This systematic review was done through a search in three databases for published articles that included the concomitant use of cannabinoids and opioids for the treatment of cancer-related pain. The results were presented in a table indicating the results obtained, as well as the population under study.
Results: 10 studies between 2011 and 2021 with a total of 4,963 participants were considered. The studies range from randomized controlled-trials, prospective surveys and a case study. Most studies have reflected benefits in pain control and reduced use of opioids.
Discussion: Several studies pointed at a possible benefit of using cannabinoids and opioids in association to manage cancer-related pain, but there is a need for further investigation.
Keywords
Opioids; Medical cannabis; Cancer-related pain; Cannabinoids
Introduction
Cancer is the disease that causes the highest numbers of morbidity and mortality in the world, having emerged 18.1 million new cases and caused 9.6 million deaths in 2018 [1]. Although scientific advances have provided increasingly innovative treatments in radiotherapy and chemotherapy or even curative surgery, its application generates, in addition to the symptoms of the disease itself, adverse effects that significantly affect the patient’s quality of life [2]. One of the most prevalent symptoms in cancer patients and that affects their quality of life is chronic pain whether it’s persistent or intermittent pain resulting from the disease or even from treatments [3]. It is estimated that 33% of patients experience pain after curative treatment, 59% during the treatment and 64% in metastasized, advanced or terminal disease [3].
The guidelines for cancer-related pain follows the three-step ladder proposed by the World Health Organization, in which the first step in pain management is non-opioid medications, escalating to the next levels with the introduction of opioids for moderate and severe pain, using a scheme of opioid rotation to achieve results in pain management [1].
Effective opioid therapy involves individualization of the dose, titration of its increase and decrease and rotation of different opioids. It also requires a rigorous control in the balance between efficacy and side effects, being common the need to increase the dose, due to the creation of tolerance, without exceeding the therapeutic window of the drug [4].
Another common effect of opioid use, experienced by patients treated with these drugs, is the withdrawal symptom generated by dose reduction [5]. Finally, these drugs are also likely to cause overdose, sometimes related to an improper increase in dose and without medical supervision, related to loss of effectiveness (tolerance) after long periods of use [4,5].
Considering that opioids are the main therapy for moderate and severe pain in cancer patients, and even though opioids are relatively accessible and available on the market, their use often proves difficult due to the need for constant adaptation to the patient and the risks of dependence, tolerance and overdose. Thus, it makes sense to find new treatments that can replace opioids or, at least, reduce their dangers to the health of patients, improving their quality of life before, during and after treatment [3].
The legalization of the use of cannabis for medicinal purposes has created new hope for patients with chronic pain, namely cancer patients. Despite its application in cancer-related pain in several countries (namely Canada, Netherlands, Switzerland, Czechia, Australia, Germany and more recently, Portugal), the WHO guidelines still refer to the need for greater evidence of its benefits in this therapeutic application, namely, in comparison with opioids [1].
One of the potential advantages of using cannabinoids is the less serious side effects than opioids. Whiting et al. studied the adverse effects of cannabinoid use, identifying that the most frequent risks were dizziness, dry mouth, disorientation, nausea, euphoria, confusion and drowsiness. He further concluded from his observations that serious adverse effects were rare [6]. Effects of prolonged use of cannabinoids were studied by Serpell et al. during a three-year patient follow-up with multiple sclerosis, revealing that common side effects were experienced by most patients in mild to moderate form. The main symptoms were dizziness, fatigue and headache [7].
The issues of addiction induced by cannabis use have been discussed and need further development. A report produced by the European Union reveals that in studies carried out with prolonged use of recreational cannabis, this substance could possibly cause dependence, which could also be an indicator for medicinal use [8].
Some studies intended to verify the effectiveness of medicinal cannabis in various diseases, comparing it with placebo or other conventional medicines. A study by Fallon et al. with patients with advanced cancer unresponsive to maximum opioid dosages, sought to understand whether the use of a commercial cannabis product (Sativex®) compared to placebo influenced these patients’ perception of pain. The results obtained suggested that there was no significant difference in the reduction of pain in patients between the group given cannabis and the placebo group. However, the questionnaires on the perception of quality of life showed that patients who were in the cannabis group revealed a slight improvement in quality of life despite the pain indices not having changed significantly [9].
Some systematic reviews and meta-analyses, in order to understand the effectiveness and safety of cannabinoid use, applied to different diseases [10] or even to various cancer symptoms [11], concluded that there are no benefits in the use of cannabinoids and still significant adverse effects (such as drowsiness and dizziness) related to the use of these products.
However, a 2020 review on the concomitant use of cannabinoids and opioids in non-cancer related pain brought together 9 studies that suggested the use of medicinal cannabis as an adjunct to opioids allowed for a reduction in the use of opioids in participants [12].
All the studies mentioned above point to the need for more well- planned research studies to better understand the role of medicinal cannabis in different symptoms, namely pain and cancer-related pain.
The objective of this work is to determine whether the use of cannabinoids along with opioid therapy brings benefits for patients with chronic cancer-related pain. These benefits were classified as (1) improved pain management (2) reduced use of opioids. To define the research questions, it was used the PICO strategy (population, intervention, comparison and outcome) as demonstrated in Table 1.
| Population | Intervention | Comparison | Outcome |
|---|---|---|---|
| Patients with cancer-associated pain | Cannabinoids or Medical cannabis for pain management | Opioids | Pain management; opioids reduction |
Table 1: PICO strategy.
For this purpose, articles related to the impacts of the simultaneous use of medicinal cannabis or cannabinoids and opioids on cancer- related pain were searched in three databases of scientific articles. The articles resulting from the research were analyzed and selected through inclusion and exclusion criteria and the results presented and discussed.
Methodology
This literature review was carried out by searching articles published in three databases, PubMed, Scopus and Web of Science, and later analysed and included using the PRISMA methodology (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) [13].
Research questions and hypothesis
The hypotheses we put forward in this study are directly related to the research questions and with the objectives proposed to this review and are presented in the Table 2.
| Questions | Hypothesis |
|---|---|
| Is there evidence that the use of cannabinoids together with opioids causes a decrease in chronic cancer-related pain? | Concomitant use of cannabinoids and opioids reduces pain in patients with chronic cancer-related pain |
| Can the use of cannabinoids lead to decreased opioid consumption in patients with chronic pain associated with cancer? | The use of cannabinoids allows the reduction of opioid use |
Table 2: Research questions and hypothesis.
Search strategy
The search for scientific articles on the use of medicinal cannabis or cannabinoids and opioids was performed in June 2021 and the keywords “cannabis or cannabinoids”, “cancer or tumor”, “pain” and “opioid” were used. Three databases were selected for the research: PubMed, Web of Science and Scopus. The date filter was applied between 2011 and 2021, considering that, in most countries, the use of cannabis for medicinal purposes was approved less than 10 years ago [8].
Inclusion, exclusion and selection criteria
Studies published between 2011 and 2021 were included. Studies were included in the review if they met the following criteria: studies in people comparing the use of cannabinoids and opioids for cancer-related pain with an outcome that could be pain management or change in opioid consumption; Studies considering multiple pathologies were also considered, if patients with chronic pain associated with cancer were considered in the sample; Studies including synthetic cannabinoids.
Exclusion criteria considered for non-selection of articles were: recreational use of cannabis by patients; studies in animals; studies in models or in healthy people; comparative studies with only placebo or other drugs other than opioids; patients with chronic pain associated with other pathologies and where the outcomes are not mentioned; systematic reviews or meta-analysis to avoid duplication of results; and finally, reports, unpublished articles and conference abstracts were also excluded.
Results
A total of 406 articles were found in the three databases by searching for keywords. After removing the duplicate articles using Mendeley Desktop Software, 267 articles were eligible for screening. In the next phase, the titles and abstracts of selected articles were read, removing all those not related to cancer-related pain, studies carried out in murine or other models, studies in non-English language and systematic reviews and meta-analyses. After this exclusion, 108 articles were to be considered.
Finally, the articles were read in their entirety, and we preceded the exclusion stage. We have excluded articles which were analyzing different diseases or symptoms, did not make a clear separation between them and articles in which the cannabis-opioids comparison was made based on the recreational use of cannabis by patients. At the end of this stage, we found that 10 articles could be included in our analysis.
A summary of the methodology applied for inclusion and exclusion of results is illustrated in Figure 1.
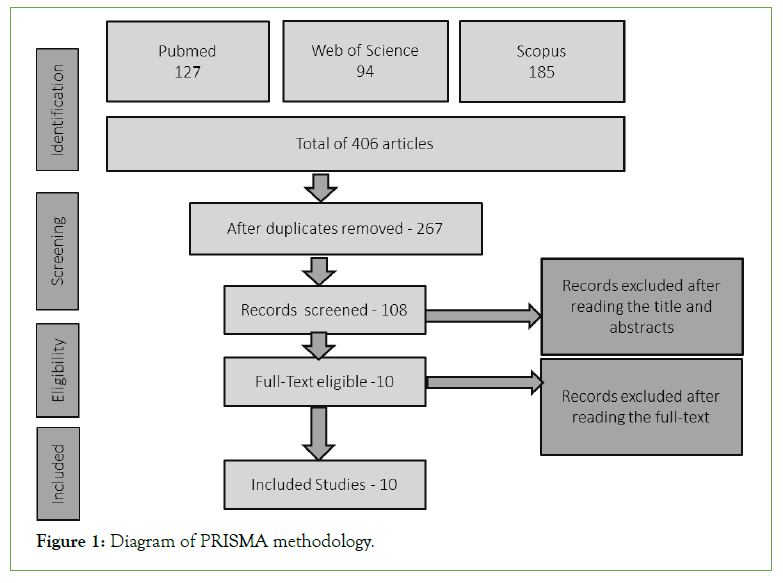
Figure 1: Diagram of PRISMA methodology.
We were able to identify 10 studies that met the inclusion requirements and are represented in Table 3. The 10 publications with the studies identified that met the inclusion requirements are represented in Table 3 [14-23].
| Method | Population | Intervention | Results |
|---|---|---|---|
| Single-Institution Survey-based study | 34 Patients with a gynaecologic malignancy, with more than 18 years old, able to read and understand English | Received a prescription (certification) for medical cannabis by a gynaecologic oncology provider, and used medical cannabis obtained through a licensed dispensary. | Patients perceived medical cannabis to be effective in relieving cancer and treatment-related symptoms. Patients reported improvement in a variety of symptoms including pain, neuropathy, nausea, insomnia, decreased appetite, and anxiety. Most patients in the study felt that medical cannabis was equivalent or superior in efficacy to other medications (e.g., opioids, antiemetics, anxiolytics, and sleep aids) in relieving their symptoms. |
| Retrospective cohort study of patients with cancer | A total of 83 cancer patients at an academic medical centre palliative care clinic | 61 in the opioid monotherapy group and 22 in the cannabis plus opioid group | The findings suggest that further research is warranted to determine the impact of cannabis use on opioid dosing in patients receiving palliative care for cancer. |
| Prospective study with interviews 1 and 6 months after medication | 2736 patients above 65 years of age (1001 cancer related patients) | Medical cannabis from January 2015 to October 2017 in a specialized medical cannabis clinic | The study finds that the therapeutic use of cannabis is safe and efficacious in this population. Cannabis use can decrease the use of other prescription medicines, including opioids. |
| Retrospective chart review of Medical Marijuana (MMJ)-certified oncology patients | 232 patients | Medical Marijuana (MMJ) | Compared to patients solely utilizing opioids, MMJ as an adjunctive therapy provided analogous symptomatic relief without the additional burden of opioid dose escalation. |
| Sub-analyses of patients, using MMJ reduced daily opioid consumption by 33% compared to those who did not use MMJ, which daily opiate consumption experienced a statistical and clinically significant median increase of nearly 23%. | |||
| Retrospective cohort study, monocentric | 28 patients with lung cancer under 50 years old | Cannabis | The impact of cannabis use on opioids prescription in patients with bronchial cancer in terms of analgesia is not confirmed |
| Retrospective online survey | 1513 participants, but only 5.9% cancer patients | Medical cannabis (vaporizer, edibles, tincture, concentrates and topic) | 76.7% of all the participants indicated the reduction of opiodsopioids use slightly or a lot since they began using Medical Cannabis (MC) |
| Randomized controlled trial, (open-label, multicenter, follow-up study). | 43 patients with cancer-related pain experiencing inadequate analgesia despite chronic opioid dosing | THC/CBD spray, THC spray | Brief Pain Inventory-Short Form scores for “pain severity” and “worst pain” domains showed a decrease (i.e., improvement) at each visit in the THC/CBD spray patients. |
| This study showed that the long-term use of THC/CBD spray was generally well tolerated, with no evidence of a loss of effect for the relief of cancer-related pain with long-term use. Furthermore, patients who kept using the study medication did not seek to increase their dose of this or other pain-relieving medication over time, suggesting that the adjuvant use of cannabinoids in cancer-related pain could provide useful benefit. | |||
| Case-Report | A 56-year-old man who developed chronic pain following the excision of a facial cancer | Nabilone (a synthetic cannabinoid) | Improved pain control, itching sensation and was able to touch the right side of his face and ear comfortably for the first time in 4 years. The patient went several days without requiring any breakthrough analgesia being able to reduce his oxycodone and ketamine doses without adversely impacting on his symptom control. The adverse effect encountered on starting of nabilone was initial light-headedness that disappeared within 48 h of starting the medication. He was reviewed in the clinic after 1 month and he remained pain free. |
| Randomized, double-blind, placebo-controlled, graded-dose study. | 263 adult patients with active cancer and chronic pain that was moderate or severe despite a stable opioid regimen that could not be made more effective by further opioid dose titration | Nabiximols or an identically appearing placebo | Nabiximols has analgesic efficacy as add-on therapy for pain from advanced cancer that is poorly responsive to opioid therapy has great potential clinical relevance |
Table 3: Included studies.
Reduction of cancer-related pain
Of the 10 studies included in this review, 7 report the effectiveness of cannabinoids in the treatment of cancer-related pain and 2 reveal this inconclusive link, referring to the need for more studies to establish a more concrete relationship between the use of these medications and the relief of pain from disease or its ongoing treatments. In the study by Webster et al. in addition to effectiveness on pain, authors also point to effectiveness on other symptoms resulting or not from the disease, such as anxiety, insomnia and nausea [14]. Three of the included studies also revealed that cannabinoids were safe and well tolerated by patients.
Reduction of opioid use
One of the major problems related to the use of opioids is the creation of tolerance to the drug and therefore the need for dose adjustments. In this review, one of the aims was to understand whether cannabinoids used as adjuvants to opioids in pain reduction could also help patients to maintain or reduce the use of opioids without losing their ability to manage pain.
Of the studies named, 6 referred to the possibility of using cannabinoids as an adjuvant, being able to maintain or reduce the use of opioids. Pawasarat et al. mentions a reduction of about 33% in the daily use of opioids by patients who used medical marijuana compared to patients who only took opioid therapy [17]. On the other hand, Johnson et al. reveals that the use of cannabinoids by patients allowed them not to need an increase in the dosage of opioids, not mentioning, however, the possibility of reduction [20].
Discussion
This study aimed to compare the concomitant use of cannabinoids and opioids and look for evidence on the potential reduction of cancer-related pain and on the reduction in the use of opioids by patients resulting from the association of cannabinoids and opioids as a pain management therapy.
Most of the studies consulted revealed not only effectiveness in reducing pain but also the potential of cannabinoids in maintaining or reducing the use of opioids. However, this link is not completely conclusive, considering the small number of studies consulted.
Cannabis illegalization in the 20th century in most countries around the world made it difficult to access the product and, consequently, to the scientific investigation of its medical properties [24]. Although its mechanism of action, the endocannabinoid system, and the isolation of its molecules, has brought more knowledge about its capabilities, its benefits for human health continue to need more evidence and studies [25].
The need for well-designed, prospective, randomized studies becomes imperative if we are to better understand their benefits or harms to human health.
Thus, the limitations of this study were the number of articles that met the inclusion criteria. In most of the articles found, studies were performed on other diseases or symptoms, or on animal models. Cases where recreational uses were considered were also excluded as they did not meet the requirements or medical control of dosages and doses. Few articles were based on prospective randomized clinical-trials, and several were retrospective, being difficult to assess potential secondary variables. The results obtained by this article show the need for further investigation, mainly through more robust studies that can identify with greater evidence the relevancy of the use of medical cannabis in pain and in greater control in the use of opioids.
Conclusion
This theme still has a long way to go. Future studies can provide more answers to the questions raised here and do it broken down by symptom or disease, allowing for a more concrete reading of the results. In cancer, treatments have greatly increased the life expectancy of patients, which means a longer period with symptoms associated with the disease and treatment that must be managed efficiently. Opioid therapy for pain, in addition to bringing serious health risks to these patients, is also dragged in time, losing its effect. The search for alternative or adjuvant medications for this symptom is increasingly pressing and medical cannabis can be an effective alternative. But for that, more studies must be carried out to confirm or refute this relationship.
Conflict of Interest
The Author declares that there is no conflict of interest.
REFERENCES
- World Health Organization. WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. In: World Health Organization. 2018.
[GoogleScholar] [PubMed]
- Cheng X, Wei S, Zhang H, Xue S, Wang W, Zhang K. Nurse-led interventions on quality of life for patients with cancer: A meta-analysis. Medicine. 2018;97(34).
[CrossRef] [GoogleScholar] [PubMed]
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, et al. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2018;29:iv166-iv191.
[CrossRef] [GoogleScholar] [PubMed]
- Portenoy RK, Ganae-Motan ED, Allende S, Yanagihara R, Shaiova L, Weinstein S, et al. Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded-dose trial. J Pain. 2012;13(5):438-449.
[CrossRef] [GoogleScholar] [PubMed]
- Ebbert JO, Scharf EL, Hurt RT. Medical cannabis. Mayo Clin Proc. 2018; 93(12):1842-1847.
[CrossRef] [GoogleScholar] [PubMed]
- Whiting PF, Wolff RF, Deshpande S, di Nisio M, Duffy S, Hernandez AV, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
[CrossRef] [GoogleScholar] [PubMed]
- Serpell MG, Notcutt W, Collin C. Sativex long-term use: an open-label trial in patients with spasticity due to multiple sclerosis. J neurol. 2013;260(1):285-295.
[CrossRef] [GoogleScholar] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction. Medical use of cannabis and cannabinoids. 2018.
[CrossRef]
- Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, et al. Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain. 2017;11(3):119-133.
[CrossRef] [GoogleScholar] [PubMed]
- Montero-Oleas N, Arevalo-Rodriguez I, Nuñez-González S, Viteri-García A, Simancas-Racines D. Therapeutic use of cannabis and cannabinoids: an evidence mapping and appraisal of systematic reviews. BMC Complement Med Ther. 2020;20(1):1-5.
[CrossRef] [GoogleScholar] [PubMed]
- Boland EG, Bennett MI, Allgar V, Boland JW. Cannabinoids for adult cancer-related pain: systematic review and meta-analysis. BMJ Support Palliat Care. 2020;10(1):14-24.
[CrossRef] [GoogleScholar] [PubMed]
- Okusanya BO, Asaolu IO, Ehiri JE, Kimaru LJ, Okechukwu A, Rosales C. Medical cannabis for the reduction of opioid dosage in the treatment of non-cancer chronic pain: a systematic review. Syst Rev. 2020;9(1):1-8.
[CrossRef] [GoogleScholar] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Webster EM, Yadav GS, Gysler S, McNamara B, Black J, Tymon-Rosario J, et al. Prescribed medical cannabis in women with gynecologic malignancies: A single-institution survey-based study. Gynecol Oncol Rep. 2020;34:100667.
[CrossRef] [GoogleScholar] [PubMed]
- Pritchard ER, Dayer L, Belz J, Forseth B, Harrington SE, Painter JT. Effect of cannabis on opioid use in patients with cancer receiving palliative care. J Am Pharm Assoc. 2020;60(1):244-247.
[CrossRef] [GoogleScholar] [PubMed]
- Abuhasira R, Schleider LB, Mechoulam R, Novack V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur J Intern Med. 2018;49:44-50.
[CrossRef] [GoogleScholar] [PubMed]
- Pawasarat IM, Schultz EM, Frisby JC, Mehta S, Angelo MA, Hardy SS, Kim TW. The efficacy of medical marijuana in the treatment of cancer-related pain. J Palliat Med. 2020;23(6):809-816.
[CrossRef] [GoogleScholar] [PubMed]
- Renard O, Corbin S, Drouet Y, Lasset C, Chvetzoff G. Cannabis and analgesic management: what consequences on the prescription of strong opioids? Observational study at the Léon-Bérard center of a population of patients with lung cancer. Anal pain. 2019;32(2):82-86.
[CrossRef]
- Piper BJ, de Keuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. 2017;31(5):569-575.
[CrossRef] [GoogleScholar] [PubMed]
- Johnson JR, Burnell-Nugent M, Lossignol D, Ganae-Motan ED, Potts R, Fallon MT. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage. 2010;39(2):167-79.
[CrossRef] [GoogleScholar] [PubMed]
- Reynolds TD, Osborn HL. Case Report: The use of cannabinoids in chronic pain. BMJ Case Rep. 2013;2013:bcr2013010417.
[CrossRef] [GoogleScholar] [PubMed]
- Portenoy RK. A practical approach to using adjuvant analgesics in older adults. J Am Geriatr Soc. 2020;68(4):691-698.
[CrossRef] [GoogleScholar] [PubMed]
- Zylla DM, Eklund J, Gilmore G, Gavenda A, Guggisberg J, VazquezBenitez G, et al. A randomized trial of medical cannabis in patients with stage IV cancers to assess feasibility, dose requirements, impact on pain and opioid use, safety, and overall patient satisfaction. Support Care Cancer. 2021;29(12):7471-7478.
[CrossRef] [GoogleScholar] [PubMed]
- Pisanti S, Bifulco M. Medical Cannabis: A plurimillennial history of an evergreen. J Cell Physiol. 2019;234(6):8342-8351.
[CrossRef] [GoogleScholar] [PubMed]
- Crocq MA. History of cannabis and the endocannabinoid system. Dialogues Clin Neurosci. 2020;22(3):223-228.
[CrossRef] [GoogleScholar] [PubMed]
Citation: Freitas H (2022) Cannabinoid Association with Opioid in Cancer Pain Management Therapy: A Systematic Review. J Pain Manage Med. 8:167.
Copyright: © 2022 Freitas H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

