Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 0, Issue 0
Can we Improve the Perinatal Outcomes and Early Postnatal Survival of Fetuses with Congenital Heart Disease by Initiating Specialized Prenatal Consultation Service?
Yanji Qu1, Jimei Chen1, Fengzhen Han1, Shao Lin2, Erin M. Bell2, Wei Pan1, Teresa Huang2, Yanqiu Ou1, Shusheng Wen1, Jinzhuang Mai1, Zhiqiang Nie1, Xiangmin Gao1, Yong Wu1, Emily Lipton2, Richard G. Ohye3, Jian Zhuang1 and Xiaoqing Liu1*2Department of Environmental Health Sciences, University at Albany, State University of New York, New York, USA
3Department of Cardiac Surgery, University of Michigan, Ann Arbor, Michigan, USA
Received: 21-Aug-2020 Published: 11-Sep-2020
Abstract
Background: Requirements of specialized prenatal consultation after prenatal diagnosis of Congenital Heart Disease (CHD) is increasing, but its impact is not clear. This study was to introduce such a specialized prenatal consultation service and assess its impact on outcomes of CHD fetuses.
Methods: We initiated specialized prenatal consultation in a referral tertiary cardiac center in southern China in 2013. A multidisciplinary team serves as consultants in this service and is especially responsible by two pediatric cardiologists in regular outpatient clinics. We included CHD fetuses diagnosed from 2011 to 2015 consecutively. They were divided into before (2011-2013) and after (2014-2015) specialized prenatal consultation groups and their perinatal outcomes, delivery location and early postnatal survival were compared. Risk factors for termination were also assessed.
Results: Totally, 1032 CHD fetuses were included and 533 accepted specialized prenatal consultation. After initiation of specialized prenatal consultation, the live birth rate significantly improved (OR=1.59, 95% CI: 1.10-2.29) and termination rate significantly reduced (OR=0.63, 95% CI: 0.44-0.91) in single CHD fetuses. No significant change in delivery location and postnatal survival of CHD fetuses were observed after specialized prenatal consultation. Referrals from district hospitals, along with multiple-lesion CHD, critical CHDs, gestational age<28 weeks at prenatal diagnosis were risk factors for termination.
Conclusion: Specialized prenatal consultation can improve the perinatal outcomes in single CHD fetuses. Education for district hospitals of standardizing counseling, especially for minor CHD fetuses and timely transferring of mothers with critical CHDs/multiple CHDs fetus is crucial to improve the outcomes of CHD fetuses further.
Keywords
Congenital heart disease; Prenatal diagnosis; Prenatal consultation; Perinatal outcomes; Survival
Introduction
Congenital Heart Disease (CHD), is a major cause of infant morbidity and mortality worldwide. CHD incidence is 1 per 100 live births [1,2]. The etiology of CHD remains largely unknown. Prenatal diagnosis is regarded as an effective secondary and tertiary prevention strategy [3,4]. Advances in fetal echocardiography using high-resolution ultrasound has increased CHD cases diagnosed prenatally since the 1980s [5]. Thus, the requirements for optimal prenatal consultation for the prospective parents and sequential care for CHD fetuses is increasing accordingly [6].
Although prenatal consultations are available universally, most currently available services focus on genetic and neurological congenital anomalies only [7]. While specialized prenatal consultation services exist for structural anomalies, such as CHD, only a small number of centers have designated CHD outpatient clinics [8].
Prenatal diagnosis has been expected to improve the outcomes of CHD babies by altering the site and mode of delivery, proper preparation for neonatal care, and performing intervention in utero. These expectations could not be satisfied without a professional specialized prenatal consultation service. During specialized prenatal consultation, the prenatal and postnatal natural history of CHD, its available therapies, potential perinatal management, and the long-term prognosis are provided to assist the affected families in decision making. Historically, specialized prenatal consultation service was rarely introduced and its impact on outcomes of CHD fetuses has not been investigated.
To optimize care for CHD fetuses, in December, 2013, we developed a specialized prenatal consultation service in our referral tertiary cardiac center in Southern China. A fixed outpatient clinic was selected and two professional pediatric cardiologists were designated to conduct consultations. Multidisciplinary experts provided integrated prenatal and postnatal care. This study aimed to assess the impact of this specialized prenatal consultation service on CHD fetuses’ perinatal outcomes (live birth, elective terminations, spontaneous fetal death and stillbirths), delivery location, and early postnatal survival by comparing the outcomes before and after the initiation of specialized prenatal consultation. Additionally, factors associated with elective termination compared to live births were evaluated to seek key points to improve the outcomes of CHD fetuses.
Materials and Methods
Study setting and subjects
This is a prospective cohort study. Fetuses with confirmed diagnoses of CHD were consecutively included in our center from January, 2011. Our center is one of the largest referral tertiary cardiac centers in China with more than 32,000 fetal and pediatric echocardiograms, 2000 CHD surgeries, and 1000 cardiac catheterizations are performed annually. All pregnant women in Guangdong province accepted cardiac scans through basic ultrasound and suspected fetuses were mostly referred to our center to undergo an echocardiogram [9,10]. Each prenatal CHD diagnosis was approved by two senior specialists. The prenatal diagnoses were also confirmed by postnatal echocardiogram or cardiac surgery for live births. After prenatal diagnosis of CHD, an immediate specialized prenatal consultation service was provided and serial follow-ups including echocardiogram examination and consultation were performed during pregnancy periods 4-week intervals.
Inclusion criteria: Fetuses with confirmed CHD diagnosis by echocardiogram from January, 2011 to December, 2015.
Exclusion criteria: Cases with prenatally diagnosed atrial septal defect and patent ductus arteriosus were excluded given that the foramen ovale and ductus arteriosus are still patent during pregnancy and will close physiologically after birth.
Definition of CHD phenotypes
The diagnosed CHD phenotypes were coded according to the International Classification of Diseases, 10th Revision (Q20.000-Q28.000). Principal diagnosis for a fetus affected with more than one phenotype was determined according to the Fetal Cardiovascular Disease Severity Grading Scale [11]. All cases classified as “critical CHDs (structural malformations usually require intervention to prevent death in the first year of life) [12]” versus “minor CHD (other than critical CHDs)”, and “single CHD (a single CHD phenotype presented without extra-cardiac malformation)” versus “multiple CHDs (more than one CHD phenotype presented with/without extra-cardiac malformation associated)” [6].
Specialized prenatal consultation service
We provided integrated care from prenatal to postnatal periods for CHD patients in our center. Algorithm for referral for echocardiogram and subsequent care management in our center are illustrated in Figure 1. The particular services that were not available before specialized prenatal consultation service initiation are highlighted in grey.
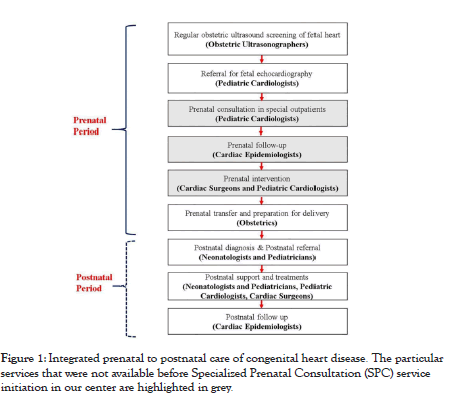
Figure 1: Integrated prenatal to postnatal care of congenital heart disease. The particular services that were not available before Specialized Prenatal Consultation (SPC) service initiation in our center are highlighted in grey
After confirmation of the prenatal CHD diagnosis and other test of chromosomal anomalies and non-cardiac abnormalities, specialized prenatal consultation was provided by two dedicated, professional pediatric cardiologists (Yufen Li, and Pan Wei) in a fixed outpatient clinic immediately. A multidisciplinary team including Obstetricians, Cardiac Surgeons, Neonatologists and Pediatrics, Cardiac Image and Epidemiologists provided integrated prenatal and postnatal care. A multidisciplinary team meeting was held to discuss the solutions for complex cases. The consultation was conducted according to the guidelines modified from practices in other countries [13].
During each consultation, consultants completed the following comprehensive criteria:
• Explain the diagnosis of fetal CHD according to the echocardiogram findings using an imaging technique.
• Explain the potential impact of fetal CHD and other associated non-cardiac defects and genetic anomalies on intrauterine fetal growth, pregnancy outcomes, delivery, neonates’ symptoms, and development after birth.
• Provide current treatment options such as medications, intrauterine treatment, interventional therapy, cardiac surgery, and more, as well as provide information on the short and long-term prognostic outcomes after treatments.
• Provide prenatal consultation suggestions for the affected parents. Only mothers of fetuses diagnosed with multiple critical were recommended to deliver at the tertiary center, but parents of all CHD fetuses were encouraged to continue regular (every 4 weeks) screening and consultation until delivery. The mean time for each consultation was 30 minutes.
Definition of study outcomes
The primary endpoint was perinatal outcomes of CHD fetuses which were defined as outcomes of pregnancy and included live births, elective termination, spontaneous abortion (natural death of an embryo or fetus <20 weeks of gestation), and stillbirths (fetal death at or after 20 to 28 weeks of pregnancy). The secondary endpoint was delivery location (our center and others) and early postnatal survival in live births with prenatally diagnosed CHD.
Data collection
A standardized questionnaire was designed to obtain maternal demographic characteristics and follow up information from all CHD fetuses. Hospital information data systems was reviewed to abstract perinatal outcomes of CHD fetuses. For cases born out of the hospital area, mothers were contacted via telephone to obtain the outcomes. For live births with CHD, postnatal diagnoses were performed and follow-ups were continued annually.
Statistical analysis
Distribution of demographic characteristics were compared between these two groups using Kruskal-Wallis or Mann-Whitney U test for continuous variables and Chi-square test for categorical variables. Proportion change of CHD phenotypes was assessed through multivariable unconditional logistic regression models adjusting for characteristics with different distributions based on iterative stepwise algorithm of significance probability (entry P<0.05, removal P>0.1).
Multivariate logistic model adjusting for maternal characteristics and proportion change of CHD phenotypes with the same algorithm was used to determine the diversity of perinatal outcomes of CHD fetuses between before and after specialized prenatal consultation group. We also used logistic models to assess the factors significantly associated with elective termination=1 compared to live births=0. Delivery location were compared between before and after specialized prenatal consultation group using Chi-square test. Survival estimates for live births were calculated using Kaplan-Meier and compared between before and after specialized prenatal consultation service with log-rank tests. SPSS ® 22.0 (IBM Co. Ltd) was used for all computations.
Results
Flow chart of our study participants was shown in Figure 2. Overall, 1,032 cases were included in the final analysis. Among them, 499 (48.4%) and 533 (51.6%) were categorized as before and after specialized prenatal consultation, respectively. The overall maternal characteristic and comparison between before and after specialized prenatal consultation was as shown in Supplementary Table 1. Numbers and proportions of CHD phenotypes diagnosed prenatally, before and after specialized prenatal consultation were presented in Figure 3.
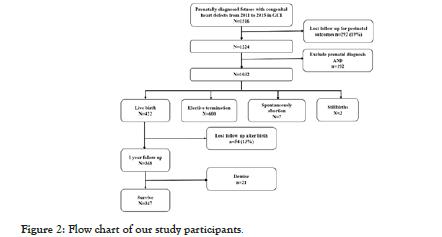
Figure 2: Flow chart of our study participants.
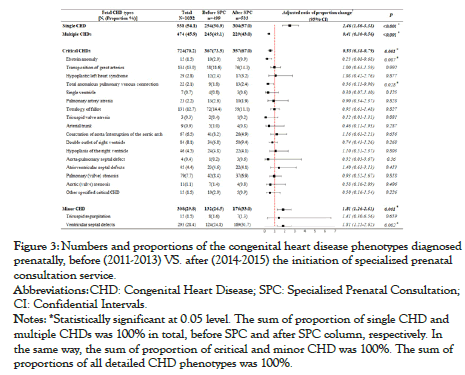
Figure 3: Numbers and proportions of the congenital heart disease phenotypes diagnosed prenatally, before (2011-2013) VS. after (2014-2015) the initiation of specialized prenatal consultation service.
Abbreviations: CHD: Congenital Heart Disease; SPC: Specialized Prenatal Consultation;CI: Confidential Intervals.
Notes: *Statistically significant at 0.05 level. The sum of proportion of single CHD and multiple CHDs was 100% in total, before SPC and after SPC column, respectively. In the same way, the sum of proportion of critical and minor CHD was 100%. The sum of proportions of all detailed CHD phenotypes was 100%.
After initiation of specialized prenatal consultation, the proportion of single and minor CHD increased (RR=2.46, 95% CI: 1.80-3.38; RR=1.81, 95% CI: 1.26-2.61) while multiple CHDs and critical CHD decreased significantly (RR=0.41, 95% CI: 0.30-0.56; RR=0.55, 95% CI: 0.38-0.79).
Overall, there were 422 (41%) live births, 600 (58%) electively terminations, 7 (0.7%) spontaneously abortion and 3 (0.3%) stillbirths. Comparison of live birth and elective termination numbers and rates of CHD fetus between before and after specialized prenatal consultation was shown in Table 1.
| CHD and phenotypes † | Before SPC | After SPC | Adjusted RR livebirth § | Adjusted RR termination § | ||||
|---|---|---|---|---|---|---|---|---|
| N ‡ | Live birth | Termination | N ‡ | Live birth | Termination | |||
| Overall CHDs | 499 | 188 (37.7) | 305 (61.1) | 533 | 234 (43.9) | 295 (55.3) | 1.22 (0.92-1.62) | 0.83 (0.62-1.10) |
| Single CHD | 254 | 118 (46.5) | 132 (52.0) | 304 | 172 (56.6) | 129 (42.4) | 1.59 (1.10-2.29) | 0.63 (0.44-0.91) |
| Multiple CHDs | 245 | 70 (28.6) | 173 (70.6) | 229 | 62 (27.1) | 166 (72.5) | 0.92 (0.60-1.41) | 1.10 (0.72-1.68) |
| Critical CHDs | 367 | 102 (27.8) | 260 (70.8) | 357 | 112 (31.4) | 242 (67.8) | 1.22 (0.89-1.71) | 0.85 (0.61-1.18) |
| TGA | 58 | 11 (19.0) | 47 (81.0) | 76 | 20 (26.3) | 56 (73.7) | 1.86 (0.76-4.52) | 0.54 (0.22-1.31) |
| TOF | 72 | 22 (30.6) | 48 (66.7) | 59 | 18 (30.5) | 39 (66.1) | 1.39 (0.56-3.41) | 0.71 (0.30-1.71) |
| CoA/IAA | 41 | 17 (41.5) | 24 (58.5) | 26 | 12 (46.2) | 14 (53.8) | 1.28 (0.43-3.86) | 0.78 (0.26-2.35) |
| DORV | 34 | 6 (17.6) | 27 (79.4) | 50 | 16 (32.0) | 33 (66.0) | 2.12 (0.69-6.48) | 0.46 (0.16-1.35) |
| C/PAVC | 23 | 4 (17.4) | 19 (82.6) | 22 | 8 (36.4) | 14 (63.6) | 3.69 (0.53-25.63) | 0.27 (0.04-1.89) |
| P(v)S | 42 | 17 (40.5) | 24 (57.1) | 37 | 17 (45.9) | 20 (54.1) | 1.08 (0.40-2.96) | 0.96 (0.35-2.61) |
| Minor CHDs | 132 | 86 (65.2) | 45 (34.1) | 176 | 122 (69.3) | 53 (30.1) | 1.25 (0.74-2.13) | 0.78 (0.45-1.32) |
| VSD | 124 | 83 (66.9) | 40 (32.3) | 169 | 118 (69.8) | 50 (29.6) | 1.20 (0.69-2.08) | 0.81 (0.47-1.41) |
Abbreviations: CHD: Congenital Heart Disease; SPC: Specialized Prenatal Consultation; Adjusted RR livebirth: Rates Ratio of the live birth rate before and after specialized prenatal consultation service; Adjusted RR termination: Rates Ratio of the elective termination rate before and after specialized prenatal consultation service; TGA: Transposition of Great Arteries; TOF: Tetralogy of Fallot; CoA/IAA: Coarctation of Aorta/Interruption of the Aortic Arch; DORV: Double Outlet Right Ventricle; CAVC/PAVC: Atrioventricular Septal Defects; P(V)S: Pulmonary Valve Stenosis; VSD: Ventricular Septal Defects
Notes: † Only CHD phenotypes with number >40 were presented;
‡ Total number of live births, elective termination, stillbirths and spontaneous abortion; Spontaneous abortion (n=7) and stillbirths (n=3) were not present;
§ For overall CHD, we adjusted proportion change of isolated/multiple-lesion CHD, minor/CCHD, referrals from district hospitals for echocardiogram, maternal education, and migrants; For CHD phenotypes, we only adjusted for referrals from district hospitals for echocardiogram, maternal education, and migrants.
Table 1: Comparison of live birth and elective termination numbers and rates [N, (%)] of fetuses with prenatally diagnosed congenital heart disease, before (2011-2013) vs. after specialized prenatal consultation service (2014-2015).
In brief, we observed a significant increase of the live birth rate (OR adjusted=1.59, 95%CI: 1.10-2.29) and a decrease of elective termination rate (OR adjusted=0.63, 95%CI: 0.44-0.91) in single CHD after specialized prenatal consultation service initiation after adjusting for discrepancies of demographic characteristics and proportional change of CHD phenotypes. We did not observe a significant change of perinatal outcomes in other CHD phenotypes after specialized prenatal consultation service initiation. However, most rate ratios (RR) of live birth rate after and before specialized prenatal consultation were consistently at above 1.0. The termination rate in fetuses with minor CHD, such as ventricular septal defects was stable at a high level (30%), even after specialized prenatal consultation.
For location of outcomes occurred, overall, 34.1% (144/422) live births, 8.2% (49/600) elective terminations, 57.1% (4/7) spontaneous abortions, and 33.3% (1/3) still birth occurred at our tertiary cardiac center. As Supplementary Table 2 showed, the location of perinatal outcome diagnoses did not change after specialized prenatal consultation initiation.
The risk factors for termination using live birth as a reference. Critical CHDs (OR=4.19, 95%: 2.97-5.91), gestational age<28 weeks at the prenatal diagnosis (OR=2.87, 95%: 2.13-3.85), multiple CHDs (OR=1.61, 95%: 1.17-2.21), and referrals from district hospitals for fetal echocardiogram (OR=1.6, 95%: 1.16- 2.19) were significantly associated with termination (Figure 4).
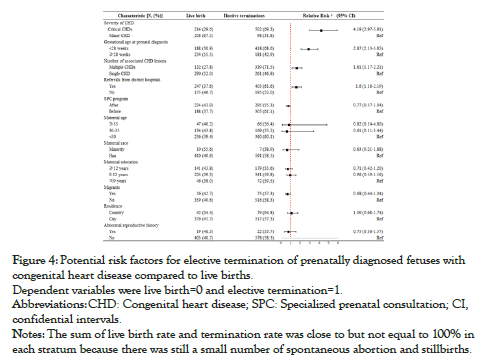
Figure 4: Potential risk factors for elective termination of prenatally diagnosed fetuses with congenital heart disease compared to live births. Dependent variables were live birth=0 and elective termination=1.
Abbreviations: CHD: Congenital heart disease; SPC: Specialized prenatal consultation; CI, confidential intervals.
Notes: The sum of live birth rate and termination rate was close to but not equal to 100% in each stratum because there was still a small number of spontaneous abortion and stillbirths.
Among the 422 live births, 47 (12.8%) patients were lost to follow up and ten (2.4%) died within seven days of delivery. The survival rate for overall live births, before and after specialized prenatal consultation service was 95.2%, 94.2% and 96.0% with a mean follow-up time of 4.01, 4.07 and 1.89 years after birth, respectively. There was no significant difference in the survival rate between before and after specialized prenatal consultation (P=0.192), under the context that the distribution of maternal characteristics and CHD phenotypes were comparable between the two groups.
Discussion
Overall, specialized prenatal consultation service significantly improved the perinatal outcomes [live birth rate] of single CHD fetuses. There is no significant change in delivery location and the early postnatal survival of CHD live births after specialized prenatal consultation compared to before its initiation. Referrals from local hospitals, along with multiple CHDs, critical CHDs, gestational age<28 weeks at prenatal diagnosis were independent risk factors for elective termination compared to live birth.
Perinatal outcomes of CHD fetuses after specialized prenatal consultation service initiation
The improvement of perinatal outcomes [higher live birth rate, lower termination rate] in single CHD was inspiring and supported the objective of specialized prenatal consultation. While most single and minor CHD can be corrected, the termination rate was high (30%) for minor CHDs and we did not observe an improved perinatal outcome after specialized prenatal consultation initiation. These termination seldomly occurred at our center (<10%). Highlighting the importance of standardizing counseling in district hospitals targeting parents with minor CHD fetuses in further study. Limited by sample size, we did not observe a significantly improved live birth rate in overall CHD fetuses after specialized prenatal consultation. The power to detect the significance of an OR=1.22 was only 26% at 0.05 level with our current sample size.
Although the impact of specialized prenatal consultation on perinatal outcomes of CHD fetuses was rarely assessed. Several previous studies described perinatal outcomes following prenatal diagnosis of CHD and their results varied significantly by country [14-18]. Different insurance systems, legal limitations on termination, social policy and ethnic and religious beliefs contributed to the varied termination rate in different regions. The overall elective termination rate (58.1%) in our study was higher than other countries, with rates ranging from 20% to 53% [14-17,19]. Similar to previous studies, it was difficult to change termination rates after prenatal diagnosis of CHD due to locally accepted cultural and social norms [20,21]. We respected the choice of the affected families after informing them of the diagnosis and known interventions and survival rates. The termination rates in this study are comparable to previous results from South China (57%) [18] and lower than that in Northern China (85%) [22]. The observed lower rate in south China may be attributable to treatment improvements, better access of such specialized prenatal consultation service for CHD cases in that region.
Proportion change of CHD phenotypes after specialized prenatal consultation service initiation
Due to a higher detection rate for critical CHDs compared to minor CHD prenatally, critical CHDs comprised the majority of our CHD patients. This was consistent with prior studies [14,23]. However, after specialized prenatal consultation began, the proportion of minor and single CHD significantly increased. This increase accordingly led to the decrease of proportions of critical CHDs and multiple CHDs. Enhanced prenatal screening access and improved detection technique may be a contributor to both the significant increase of diagnosed single and minor CHDs. Meanwhile, some fetuses with severe CHD tended to be terminated after suspected diagnosis in district hospitals before their referral to our center. This may contribute to the decreased proportion of critical CHDs and multiple CHDs. Early detection of severe forms of CHD resulting in an increased pregnancy termination rate in the first trimester was also reported previously [16].
Early postnatal survival after specialized prenatal consultation service initiation
No improvement of early postnatal survival because of similar delivery location for live births between before and after specialized prenatal consultation. Even for live births with critical CHDs and multiple CHDs, the percentage of them delivering at our center remained stable at less than 50%. Although we emphasized the benefit of transferring mothers for delivery to a tertiary cardiac center instead of transferring neonates with critical CHDs and multiple CHDs, more than half of the affected families refused to do so. Therefore, education for district hospitals on timely transferring mothers with prenatally diagnosed critical CHDs and multiple CHDs babies is just as important as improving management and treatment protocols in these same hospitals.
Risk factors for elective termination compared to live birth
As anticipated, the independent risk factors for elective terminations (compared to live births) included multiple CHDs, critical CHDs, gestational age<28 weeks at prenatal diagnosis, and referrals from local hospitals. Maternal geographic origins, gestational age at diagnosis, severity of the heart defect and presence of associated malformations has been reported to be the significant factors for termination of pregnancy in previous studies [19,24]. Referral from local hospitals is a novel and potentially modifiable predictor for elective termination in this study.
We observed that a very low proportion of the total elective terminations (8%) occurred at our center. Mothers from primary and secondary health facilities tended to return to their local hospital after echocardiogram for follow-up where they may have been counseled to terminate due to the high complexity of CHD and inadequately trained local doctors. The high elective termination rate for ventricular septal defects (30%) and extremely low proportion (6%) of terminations occurring at our center also supports this explanation. Continued specialized follow-up care, including professional consultation has been identified as a critical component in a family’s decisions regarding termination [6]. Therefore, moving forward, we are providing training to health professionals using our standardized consultation and referral system, with a particular focus on minor CHD education in district hospitals to improve the CHD fetuses’ perinatal outcomes.
Limitations
Limitations should be considered when interpreting the results. First, potential bias associated with different distributions of certain maternal demographics between the populations before and after specialized prenatal consultation initiation should be considered. However, since we included all prenatally diagnosed CHD fetuses and their mothers in our tertiary cardiac center continuously without selection, and maternal characteristics together with the proportional change of CHD phenotypes, were included as adjusted factors in the models, the bias impact should be minimized. Second, selection bias would also affect the study outcomes if the loss of follow-up rate was high. Of all the enrolled mothers, 81% (1224/1516) were successfully followed up. For live births, 88.7% (375/422) were followed up for their early survival status. Sensitivity analysis was performed, and we did not observe a significant difference of the maternal characteristics between follow-up gravidas and not, before and after specialized prenatal consultation participants. Third, misclassification of the CHD lesion could be another concern during prenatal diagnosis. In the current study, we confirmed the prenatal diagnoses by postnatal echocardiographic examination or operation in live births. The positive predictive value of prenatal diagnosis was 91% and the overall concordance rate was comparable to previous studies (81%) [25].
Conclusion
Specialized prenatal consultation service reduced unnecessary terminations and improved the live birth rate of CHD fetuses with single CHD. Similar delivery location resulted in no significant improvement of early survival for CHD live births after specialized prenatal consultation. Referrals from local hospitals, along with multiple CHDs, critical CHDs, gestational age<28 weeks at prenatal diagnosis were independent risk factors for elective termination compared to live birth. In the future, multilevel education for standardizing prenatal counseling for CHD, especially for minor CHD and timely transferring mothers with critical CHDs/multiple CHDs fetuses to deliver at an equipped hospital is crucial for improving the outcomes of CHD fetuses.
Financial Support
This work was supported by the [Chinese National Key Research and Development Program] under Grant [2018YFC1002600]; [Science and Technology Department of Guangdong Province] under Grant [2014A050503048, 2017A070701013, 2017B090904034, 2017030314109, and 20193020230003]; [Guangdong Peak Project] under Grant [DFJH201802] and [Guangdong Provincial Key Laboratory of South China Structural Heart Disease] under Grant [2012A061400008].
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation in China and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Ethics Committee of Guangdong Provincial People’s Hospital.
REFERENCES
- Qu Y, Liu X, Zhuang J,Chen G, Mai J, Guo X, et al. Incidence of congenital heart disease: The 9-year experience of the guangdong registry of congenital heart disease, China. PLOS One.2016;11 (3):e0159257.
- Hoffman J. Incidence of congenital heart disease:II. Prenatal incidence. Pediatr cardiol.1995; 16:155-165.
- Calderon J, Angeard N, Moutier S, Plumet MH, Jambaqué I, Bonnet D, et al. Impact of prenatal diagnosis on neurocognitive outcomes in children with transposition of the great arteries. J Pediatr. 2012;161:94-98.
- Velzen VC, Haak M, Reijnders G. Prenatal detection of transposition of the great arteries reduces mortality and morbidity. Ultrasound Obstet Gynecol. 2015;45: 320-325.
- Gardiner H. Fetal echocardiography: 20 years of progress. Heart. 2001;86 [Suppl II]:ii12–ii22.
- Donofrio MT, Moon-Grady AJ, Hornberger LK. Diagnosis and treatment of fetal cardiac disease: A scientific statement from the American Heart Association. Circulation . 2014;129: 2183-2242.
- Gagnon A. Genetics committee: Evaluation of prenatally diagnosed structural congenital anomalies. J Obstet Gynaecol Can. 2009;31(9):875-881.
- Aite L, Zaccara A, Cuttini M, Mirante N, Nahom A, Bagolan P, et al. Lack of institutional pathways for referral: Results of a survey among pediatric surgeons on prenatal consultation for congenital anomalies. Prenat Diagn.2013; 33(9):904-907.
- Carvalho JS, Allan LD. International Society of Ultrasound in Obstetrics and Gynecology, ISUOG Practice Guidelines (updated): Sonographic screening examination of the fetal heart. Ultrasound ObstetGynecol.2013;41:348-359.
- Lee W, Allan L, Carvalho JS. ISUOG consensus statement: What constitutes a fetal echocardiogram .Ultrasound Obstet Gynecol.2008; 32:239-242.
- Davey B, Donofrio MT, Moon-Grady AJ. Development and validation of a fetal cardiovascular disease severity scale. Pediatr Cardiol. 2014; 35:1174-1180.
- Liberman RF, Getz KD, Lin AE. Delayed diagnosis of critical congenital heart defects: Trends and associated factors. Pediatrics. 2014;134:e373-381.
- Rychik J, Tian Z. Fetal cardiovascular imaging: A disease-based approach. Philadelphia: Elsevier Inc.2012:73-82.
- Montaña E, Khoury MJ, Cragan JD, Sharma S, Dhar P, Fyfe D, et al. Trends and outcomes after prenatal diagnosis of congenital cardiac malformations by fetal echocardiography in a well defined birth population, Atlanta, Georgia, 1990-1994. J Am Coll Cardiol. 1996; 28: 1805-1809.
- Lee JE, Jung KL, Kim SE. Prenatal diagnosis of congenital heart disease: Trends in pregnancy termination rate, and perinatal and 1-year infant mortalities in Korea between 1994 and 2005. J Obstet Gynaecol Res. 2010; 36:474-478.
- Khoshnood B, De Vigan C, VodovarV. Trends in prenatal diagnosis, pregnancy termination, and perinatal mortality of newborns with congenital heart disease in France, 1983-2000: A population-based evaluation. Pediatrics. 2005; 115:95-101.
- Levi S, Zhang WH, Alexander S, Viart P, Grandjean H. Eurofetus study group. Short-term outcome of isolated and associated congenital heart defects in relation to antenatal ultrasound screening. Ultrasound Obstet and Gynecol .2003;21:532-538.
- Chu C, Yan Y, Ren Y, Li X, Gui Y. Prenatal diagnosis of congenital heart diseases by fetal echocardiography in second trimester: A Chinese multicenter study. Acta obstetgynecol Scand. 2017;96:454-463.
- Khoshnood B, Lelong N, Houyel L. Prevalence, timing of diagnosis and mortality of newborns with congenital heart defects: A population-based study. Heart. 2012; 98:1667-1673.
- Khoshnood B, Lelong N, Andrieu T. Assessing sociodemographic differences [or lack thereof] in prenatal diagnosis of congenital heart defects: A population-based study. BMJ open. 2016;6:e009353.
- Fesslova V, Brankovic J, Boschetto C. Changed outcomes of fetuses with congenital heart disease: New Italian Multicentre study. J Cardiovasc Med (Hagerstown). 2015;16:568-575.
- Yang XY, Li XF, Lü XD, Liu YL. Incidence of congenital heart disease in Beijing, China. Chin med J (Engl). 2009;122:1128-1132.
- Jicinska H, Vlasin P, Jicinsky M. Does first-trimester screening modify the natural history of congenital heart disease? analysis of outcome of regional cardiac screening at 2 different time periods. Circulation. 2017; 35:1045-1055.
- Mellander M. Perinatal management, counselling and outcome of fetuses with congenital heart disease. Semin Fetal Neonatal Med .2005;10: 586-593.
- Oggè G, Gaglioti P, Maccanti S, Faggiano F, Todros T. Prenatal screening for congenital heart disease with four-chamber and outflow-tract views: A multicenter study. Ultrasound Obstet Gynecol. 2006;28:779-784.
Citation: Qu Y, Chen J, Han F, Lin S, Bell EM, Pan W, et al. (2020) Can we Improve the Perinatal Outcomes and Early Postnatal Survival of Fetuses with Congenital Heart Disease by Initiating Specialized Prenatal Consultation Service? Clinics Mother Child Health. 17:365.
Copyright: © 2020 Qu Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

