Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 9, Issue 6
Balloon-Assisted Occlusion for Surgical Repairment of Iatrogenic Subclavian Artery-Internal Jugular Vein Fistula
Qunshan Shen1, Jing Jin2, Jiajia Lu2, Gangcheng Zhang1* and Xuan Zheng1*2Department of Cardiac Surgery, Wuhan Asia Heart Hospital, Wuhan, China
Received: 29-Nov-2021 Published: 20-Dec-2021
Abstract
Central Vein Catheterization (CVC) is a safe procedure with occasional complications. Iatrogenic arteriovenous fistula may happen during CVC, among which subclavian artery-internal jugular vein fistula is extremely rare. The clinical presentations vary from asymptomatic to heart failure. Surgical repairment can be challenging due to the anatomic obstacle and high risk of bleeding. Here we present a case report of iatrogenic subclavian artery-internal jugular vein fistula in a young woman who received successfully surgical repairment with balloon-assisted occlusion.
Keywords
Balloon-assisted occlusion; Iatrogenic arteriovenous fistula; Subclavian artery-internal jugular vein fistula; Right heart catheterization
Introduction
Central Vein Catheterization (CVC) is an invasive procedure that allows medicine administration, hemodynamic monitoring and percutaneous treatment. Catheters are chosen based on clinical requirements, such as tunneled catheter maintains longterm central vein access for medicine administration, Swan-Ganz catheter offers real-time hemodynamic parameters for unstable patients during right heart catheterization. Though CVC procedure is simple and safe, complications occasionally happen when there is anatomic variation. Iatrogenic arteriovenous fistula rarely occurs during catheterization, and lead to heart failure or even death sometimes [1]. Challenging for surgical repair depends on the location of fistula and risk management during operation, such as bleeding, artery damage, and organ failure [2]. Here we present a patient with iatrogenic subclavian artery-jugular vein fistula after right heart catheterization. She received successful surgical repairment with balloon-assisted occlusion and recovered well thereafter.
Case Presentation
A 27-year old female presented moderate neck pain and nausea after right heart catheterization via internal jugular vein approach two days earlier. The patient underwent surgical repairment of Atrial Septal Defect (ASD) nine months ago. Right heart catheterization was suggested at her first follow-up because of the severe pulmonary arterial hypertension before surgery. Physical examination revealed a continuous murmur above right clavicle. Vascular ultrasound indicated a communication between subclavian artery and internal jugular vein with colorful blood flow signal (Figure 1A). Computed Tomography Angiography (CTA) imaging showed a fistula between subclavian artery and internal jugular vein with approximately 3 mm diameter (Figure 1B). Endovascular treatment would be inappropriate because the fistula was very close to the bifurcation of internal carotid artery (Figure 1C).
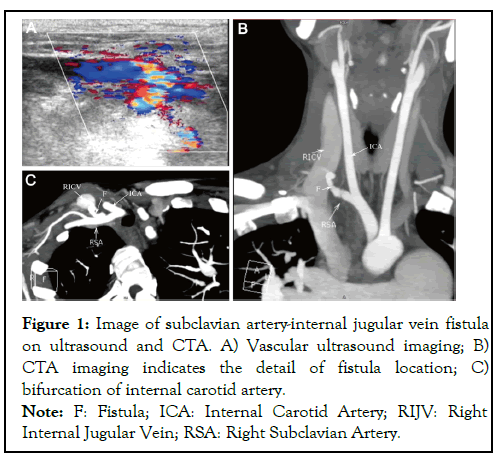
Figure 1: Image of subclavian artery-internal jugular vein fistula
on ultrasound and CTA. A) Vascular ultrasound imaging; B)
CTA imaging indicates the detail of fistula location; C)
bifurcation of internal carotid artery.
Note: F: Fistula; ICA: Internal Carotid Artery; RIJV: Right
Internal Jugular Vein; RSA: Right Subclavian Artery.
Routine surgical approach might not be able to expose the fistula, which would lead to uncontrolled blood loss and severe injury to the patient. Given the experience that using balloonassisted occlusion during great artery surgery significantly reduced the blood loss and surgery time, surgical repairment with balloon-assisted occlusion under a general anesthesia was planned to close the fistula. Angiography before surgery confirmed a leak from subclavian artery to internal jugular vein (Figure 2A), and the opening of fistula on subclavian artery was close to internal carotid artery (Figure 2B).
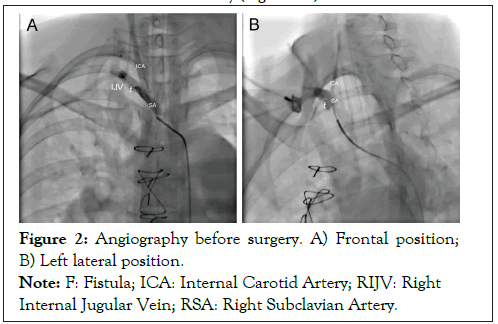
Figure 2: Angiography before surgery. A) Frontal position;
B) Left lateral position.
Note: F: Fistula; ICA: Internal Carotid Artery; RIJV: Right
Internal Jugular Vein; RSA: Right Subclavian Artery.
An 8 mm × 20 mm balloon dilatation catheter (SterlingTM, Boston Scientific, MA, USA) was preplaced on the fistula opening via right femoral artery access. Then a supraclavicular approach with transverse incision was performed to surgical close the fistula. Opening on internal jugular vein was first identified and sutured with a 6-0 polypropylene suture. The assisting balloon was soon dilated at 8 atm after fistula opening on subclavian artery was discovered. Blood flow in subclavian artery was occluded without significantly affecting in internal carotid artery (Figure 3A). Close of the fistula opening was completed in 5 min without any blood interference (Figure 3B). Digital Subtraction Angiography (DSA) later confirmed successful surgical repairment of subclavian artery without leaking or stenosis (Figure 3C). There was no remarkable change in hemoglobin after surgery. The continuous murmur and neck pain disappeared immediately after surgery. The patient recovered well and was discharged two days later.
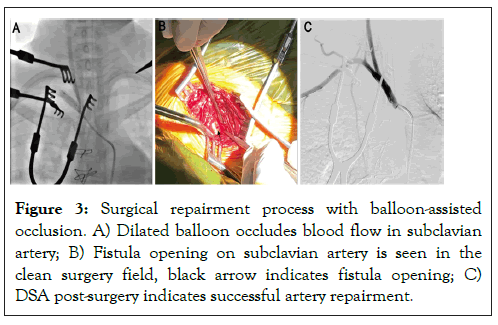
Figure 3: Surgical repairment process with balloon-assisted occlusion. A) Dilated balloon occludes blood flow in subclavian artery; B) Fistula opening on subclavian artery is seen in the clean surgery field, black arrow indicates fistula opening; C) DSA post-surgery indicates successful artery repairment.
Discussion
Right heart catherization is one of the common procedure that needs CVC. By placing the catheter into pulmonary, hemodynamic parameters can be easily obtained and monitored. Jugular vein, subclavian vein, and femoral vein are used for right heart catheterization with different advantages. Jugular vein and subclavian vein are convenient for daily maintenance. Femoral vein is preferred when straight approach is need. Being an invasive procedure, complications during CVC varied among different veins. Hematoma and artery injury are difficult to treat in jugular vein and subclavian vein because of anatomic features. Differently, thrombosis are more seen in femoral vein after catheterization due to the long-term immobilization. Among broad types of complications, iatrogenic arteriovenous fistula is uncommon but can be seen during CVCs [3]. Ultrasound guided central venous catheter insertion will significantly reduce the incidence of such complications, nonetheless, abnormal anatomy, blind puncture at emergency, lack of experience, and other reasons still cause iatrogenic arteriovenous fistula [4]. Inappropriate puncture site, sharp puncture angle, and deep insertion of the needle would also increase the chances of iatrogenic arteriovenous fistula between different vessels. Whenever this rare complication happens, repairment is necessary to reduce the symptoms and long-term complications. Though less invasive, endovascular treatment might not be considered when the fistula locating near to the original of other arteries [2,5]. In addition, high cost of the stent used for endovascular treatment also limits its clinical usage. On the contrary, surgical treatment offers a comprehensive solution to repair all kinds of arteriovenous fistula, however, complications, such as large amount of blood lost and artery damage, could be fatal. Due to the surgical process, stenosis of impaired vessel, residual fistula, and wound infection may happen post-operation. Additional surgical wound and prolonged in-hospital duration are also unacceptable for most patients. Therefore, carefully operation during catheterization is most important to avoid iatrogenic vascular damage.
Clinical diagnosis of arteriovenous fistula depends on physical examination and imaging findings. Continuous murmur on puncture site always indicates a vascular damage [6]. Vascular ultrasound indicates arteriovenous fistula with colorful blood flow signal across the vessels [7]. CTA confirms the communication between artery and venous with anatomic details. Multiple imaging will help making repairment plan to reduce the surgical risks, where vascular angiography may be further required [8].
Artery bleeding during operation is one of the most adverse complications that interfere surgical process as well as organ perfusion for surgical repairment of arteriovenous fistula. Careful preparation before surgery and advanced suture technique may reduce the risk [2]. Total circulatory arrest and median sternotomy approach provide more convenience during surgery, though extensive wound will prolong the duration of hospitalization [9]. Instead, hybridized strategy including surgical repairment and endovascular treatment/assistant may minimize the invasive approach [10]. For those who are not suitable for endovascular treatment, balloon-assisted occlusion is used during vascular surgery to reduce blood loss and improve operation performance [11].
The iatrogenic arteriovenous fistula in our case happened between subclavian artery and internal jugular vein, which might be the result of too deep insertion of the needle. The lower position of the fistula led to great difficulties in dissecting subclavian artery and bleeding control during surgical repairment. Median sternotomy approach was considered at beginning but abandoned later given the history of previous cardiac surgery. Balloon-assisted occlusion in our case not only reduced the blood loss and provided clear operation field, but also minimized the invasive approach and shortened recovery time.
Conclusion
Successful surgical repairment of iatrogenic arteriovenous fistula relies on two major factors. One is multiple imaging assessment before surgery to identify the location of fistula, which helps to accurately locate the balloon and perform the occlusion. The other is closely collaboration between surgical team and interventional team, which significantly lower the risk. Our patient recovered well at 3-months follow-up. We here provide a good solution for surgical repairing iatrogenic arteriovenous fistula less invasively.
REFERENCES
- Tohmasi S, Kabutey NK, Chen SL, Sheehan B, Duong WQ, Kuo IJ, et al. Iatrogenic arteriovenous fistula formation after endovenous laser treatment resulting in high-output cardiac failure: A case report and review of the literature. Ann Vasc Surg. 2021;72:666-e13.
- Tatar A, Mallios A. Iatrogenic jugulo-subclavian fistula. J Vasc Access. 2020:1129729820923920.
- Björkander M, Bentzer P, Schött U, Broman ME, Kander T. Mechanical complications of central venous catheter insertions: A retrospective multicenter study of incidence and risks. Acta Anaesthesiol Scand. 2019;63(1):61-68.
- Franco-Sadud R, Schnobrich D, Mathews BK, Candotti C, Abdel-Ghani S, Perez MG, et al. Recommendations on the use of ultrasound guidance for central and peripheral vascular access in adults: A position statement of the society of hospital medicine. J Hosp Med. 2019;14(14):E1-E22.
- He H, Li Q, Du M, Chen K, Li X, Li J, et al. Endovascular and surgical approaches of iatrogenic vertebrovertebral arteriovenous fistula. J Vasc Surg Cases Innov Tech. 2021;7(2):206-210.
- Sousa CN, Teles P, Dias VF, Apóstolo JL, Figueiredo MH, Martins MM. Physical examination of arteriovenous fistula: The influence of professional experience in the detection of complications. Hemodial Int. 2014;18(3):695-699.
- Novelli M, Righi D, Pilato A. Color Doppler evaluation and diagnosis of local complications after arterial endovascular procedures. Recenti Prog Med. 2012;103(9):337-347.
- González SB, Busquets JC, Figueiras RG, Martín CV, Pose CS, de Alegría AM, et al. Imaging arteriovenous fistulas. Am J Roentgenol. 2009;193(5):1425-1433.
- Jung TE, Kwon JT, Lee DH, Lee JH, Shon OJ. Surgery for subclavian arteriovenous fistula with ruptured pseudoaneurysm using total circulatory arrest. J Cardiothorac Surg. 2013;8(1):1-3.
- Palermo C, Sanfiorenzo A, Giaquinta AT, Virgilo C, Veroux M, Veroux P. Mini-invasive treatment of a large pseudoaneurysm of the neck related to central venous catheter placement: A case report. Medicine. 2018;97(29).
- Cho SB, Hong SJ, Lee S, Won JH, Choi HC, Ha JY, et al. Preoperative prophylactic balloon-assisted occlusion of the internal iliac arteries in the management of placenta Increta/Percreta. Medicine. 2020;56(8):368.
Citation: Shen Q, Jin J, Lu J, Zhang G, Zheng X (2021) Balloon-Assisted Occlusion for Surgical Repairment of Iatrogenic Subclavian Artery- Internal Jugular Vein Fistula. J Vasc Med Surg. 9:431.
Copyright: © 2021 Shen Q, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

