Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
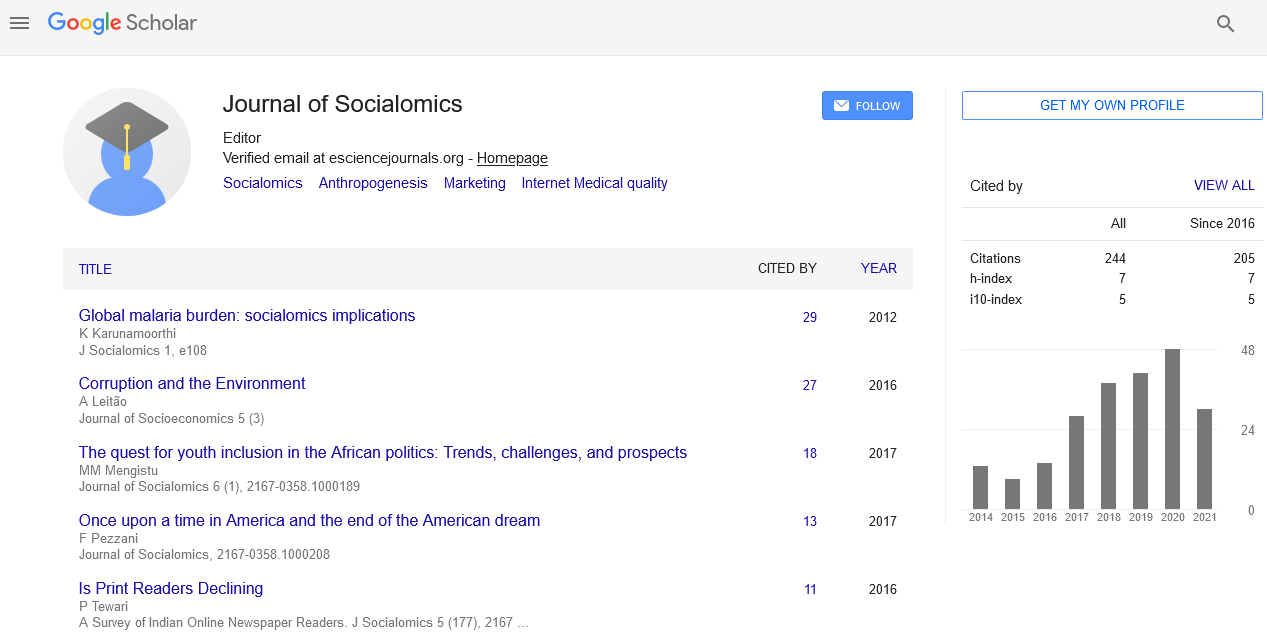
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 11, Issue 10
Authentication of Social and Non-Social Cognition in Schizophrenia and Autism Spectrum Disorders
Derks Belle*Received: 03-Oct-2022, Manuscript No. JSC-22-18628; Editor assigned: 06-Oct-2022, Pre QC No. JSC-22-18628 (PQ); Reviewed: 20-Oct-2022, QC No. JSC-22-18628; Revised: 27-Oct-2022, Manuscript No. JSC-22-18628 (R); Published: 04-Nov-2022, DOI: 10.35248/2167-0358.22.11.149
Description
Autism spectrum disorder (ASD) is characterised by persistent deficits in social interaction and communication across a variety of contexts, including deficits in social reciprocity, nonverbal communicative behaviours used for social interaction and the capacity to develop, manage, and understand relationships. Additionally, individuals with Autism spectrum disorder (ASD) exhibit constrained, recurring patterns of behaviour, interests, or activities. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, lists schizophrenia and other neurodevelopmental disorders as differential diagnoses for Autism spectrum disorder (ASD) (DSM-5) because to the similarity between the social deficiencies, unusual interests, and beliefs prevalent in Autism spectrum disorder ASD and schizophrenia's prodromal condition. Due to negative symptoms (such as decreased emotional expression or avolition), people with schizophrenia frequently exhibit of the illness. Other psychotic disorders, Autism spectrum disorder, major depressive disorder, and anxiety disorders are included in the differential diagnosis of Schizophrenia must also be identified as a comorbid illness based on DSM-5, meaning that patients with autism spectrum disorder must also have symptoms that satisfy the diagnostic standards for Schizophrenia. The unique brain mechanisms behind Autism spectrum disorder and Schizophrenia remain unknown, despite the fact that they should be clinically distinguished, produce socially and economically poor functional outcomes for individuals, and have a large detrimental impact on society.
A growing body of study demonstrates that Autism spectrum disorder and Schizophrenia have different neurocognitive dysfunction and share abnormalities in social and non-social impairment. For instance, patients with Autism spectrum disorder performed worse on tests involving facial expression perception and identification compared to patients with Schizophrenia or healthy subjects. Another study found that patients with Autism spectrum disorder Autism spectrum disorder (ASD) and Schizophrenia shared a poor performance on battery after battery of social and non-social cognition tests. To our knowledge, however, there aren't many that compare and contrast the brain correlates of social and non-social cognition in the two illnesses. Based on observations in individuals with Autism spectrum disorder (ASD) healthy people, a meta-analysis of fMRI studies aimed to infer differences in the brain foundations of social cognition between Autism spectrum disorder and Schizophrenia healthy individuals Patients with Autism spectrum disorder Autism spectrum disorder ASD performed worse on face emotion identification tasks than those with Schizophrenia Showed decreased activation in the ventrolateral prefrontal cortex, parahippocampal gyrus, and regions within the temporoparietal junction, inferior occipital gyrus, and the cerebellum, and increased brain activity in temporal regions near the superior temporal sulcus and in the anterior and posterior cingulate cortex. However, there hasn't yet been a functional neuroimaging comparison study of social and non-social cognition (such executive function) in Schizophrenia and Autism spectrum disorder individuals. The real-time hemodynamic change over the surface of the brain is measured by Functional Near-Infrared Spectroscopy (fNIRS) using infrared spectrum light. In contrast to Functional Near-Infrared Spectroscopy (fMRI), which may be unpleasant, the Functional Near-Infrared Spectroscopy (fNIRS) method is noninvasive, relatively insensitive to motion artefacts, and may evaluate brain function with individuals sat in a natural position with minimum stress throughout the examination to the participants. Due to these benefits, Functional Near-Infrared Spectroscopy (fNIRS) can be used to evaluate brain function in individuals who have psychiatric diseases including Autism spectrum disorder (ASD) and schizophrenia. Prior fNIRS investigations of Autism spectrum disorder (ASD) patients revealed that when compared to controls, Autism spectrum disorder (ASD) patients' frontopolar prefrontal areas were less activated during executive tasks (verbal fluency tasks). In a similar vein, numerous Functional Near-Infrared Spectroscopy (fNIRS) investigations of Schizophrenia patients have consistently demonstrated that their frontotemporal regions are less active during executive and emotional social cognitive tasks than those of healthy individuals. There hasn't yet been a study comparing patients with Autism spectrum disorder (ASD) and Schizophrenia that used Functional Near-Infrared Spectroscopy (fNIRS) to assess social cognition and non-social cognition (such executive function).
Citation: Belle D (2022) Authentication of Social and Non-Social Cognition in Schizophrenia and Autism Spectrum Disorders. J Socialomics. 11:149.
Copyright: © 2022 Belle D. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.