Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
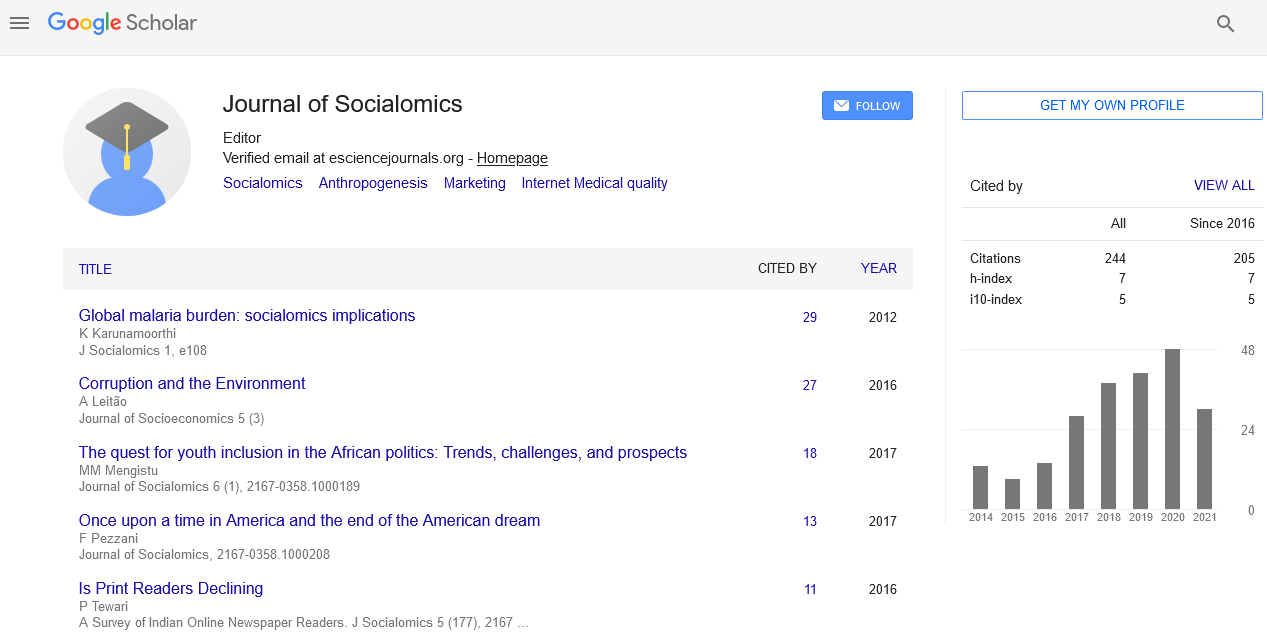
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 12
Authentication of Low-Income Patients on Social Welfare Programs
Wearne Travis*Received: 25-Nov-2022, Manuscript No. JSC-22-19370; Editor assigned: 28-Nov-2022, Pre QC No. JSC-22-19370 (PQ); Reviewed: 13-Dec-2022, QC No. JSC-22-19370; Revised: 20-Dec-2022, Manuscript No. JSC-22-19370 (R); Published: 28-Dec-2022, DOI: 10.35248/2167-0358.22.11.157
Description
The well-known factors that affects people's health and behaviours connected to their health, such as their susceptibility to infection with the coronavirus illness of 2019 (COVID-19), is low poverty. Public Assistance (PA), which covers both a minimum income and medical costs, and Free Low-Cost Medical Care (FLCMC), which only covers medical costs, is two social welfare services that help low-income patients access medical care financially. In order to determine whether social welfare programmes helped to protect low-income people's health-related quality of life during the pandemic, the goal of this study was to describe and compare the changes in Health- Related Quality of Life (HRQOL) scores before and after the COVID-19 pandemic among low-income patients receiving Public Assistance (PA), Free Low-Cost Medical Care (FLCMC), and the general population. One of the well-known factors that determine people's health and health-related behaviour and can impact Quality Of Life (QOL) is low income.
The inability to afford health care, bad habits like smoking and insufficient exercise, lower rates of cancer screening, and vaccination reluctance are just a few examples of how low income can make it difficult to maintain healthy lifestyles. Additionally, low-income individuals struggle with a variety of concerns associated to poverty, such as time and social isolation. Low-income individuals are thought to be more vulnerable to the spread of certain illnesses, such as the currently prevalent coronavirus sickness (COVID-19). According to reports, COVID-19, particularly in low-income individuals, has been linked to decreased levels of physical activity, worsened mental health, and increased levels of social isolation. As low income is one of the major factors influencing health, governments in developed nations have a number of welfare programmes that can offer financial assistance to improve livelihoods and healthcare access among the underprivileged people. Public Assistance refers to two well-known social programmes in Japan. Public Assistance is a government programme for those who are unemployed, have no assets, and are living below the poverty level. The Public Assistance programme has around 1.7% of the Japanese populace enrolled. The local municipal welfare office performs a thorough means test on each potential household to determine whether they qualify for Public Assistance (i.e., whether they are living below the poverty line, their capacity to work, the amount of financial assistance they receive from family members, and their household income). The Free Low-Cost Medical Care (FLCMC) programme is an optional one that falls under the Social Welfare Act and is offered by specific medical facilities.
The Free Low-Cost Medical Care (FLCMC's) mission is to ensure that those who are struggling financially have access to the essential medical treatment without being constrained by the cost of such care. If applicants fulfil the eligibility requirements, which are determined uniquely for each patient by the institution, Free Low-Cost Medical Care candidates are free from out-of-pocket medical payments at the authorized institutions, which cover their medical care costs. Depending on the percentage of patients using their Free Low-Cost Medical Care (FLCMC) programme, institutions may qualify for tax deductions. As a result, while FLCMC beneficiaries are considered financially constrained individuals who profit exclusively from medical care expenses, Public Assistance recipients are considered low-income individuals who benefit from minimal income protection and livelihood, including medical care expenditures. Previous international study has demonstrated that Public Assistance beneficiaries had worse health outcomes when compared to the general population. For instance, diabetes, depressed symptoms, and suicidal thoughts acts are more prevalent in Public Assistance (PA) recipients. In a similar vein, Free Low-Cost Medical Care (FLCMC) patients in Japan are more likely to have a worse quality of life connected to their health (HRQOL). The data used in these earlier investigations was collected prior to the COVID-19 pandemic. There are no studies examining the impact of welfare services on low-income persons, who could have protective health effects, despite the fact that the health implications of the pandemic have been greater among low-income communities.
Citation: Travis W (2022) Authentication of Low-Income Patients on Social Welfare Programs. J Socialomics. 11:157
Copyright: © 2022 Travis W. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.