Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
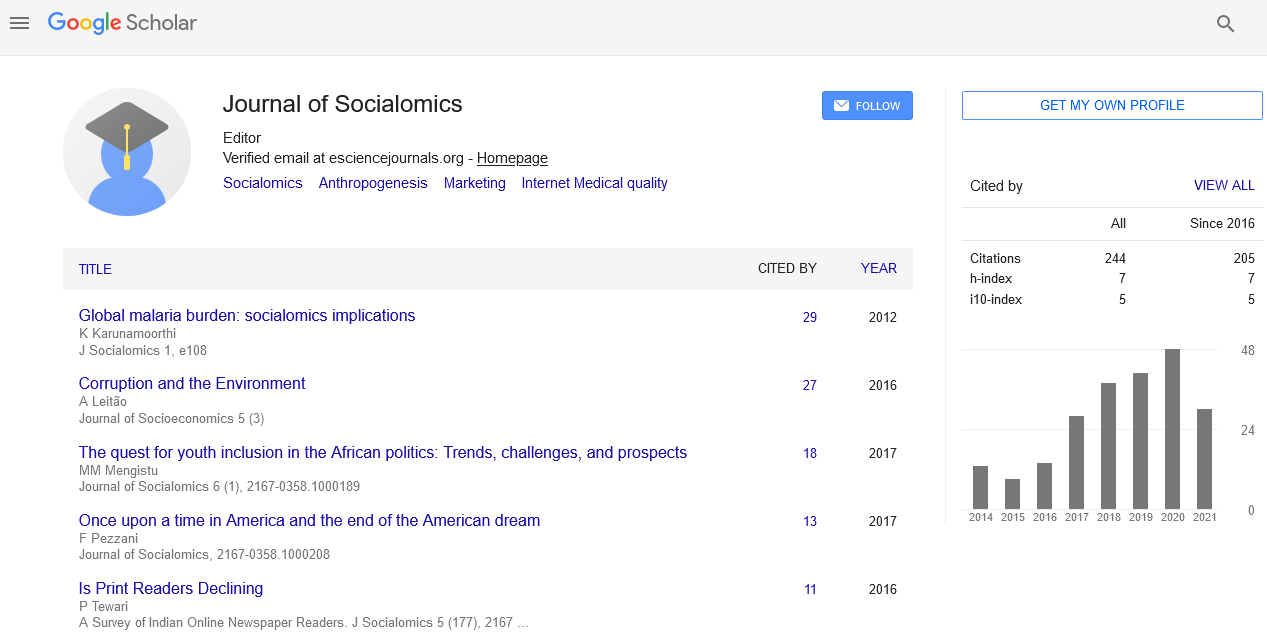
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2024) Volume 13, Issue 2
Assessment of Health Outcomes and Social Determinants of Health in United States Nursing Homes
Felix M Pabon-Rodriguez*Received: 28-Apr-2024, Manuscript No. JSC-24-25578; Editor assigned: 01-May-2024, Pre QC No. JSC-24-25578 (PQ); Reviewed: 16-May-2024, QC No. JSC-24-25578; Revised: 23-May-2024, Manuscript No. JSC-24-25578 (R); Published: 30-May-2024, DOI: 10.35248/2167-0358.24.13.227
Abstract
Addressing health disparities has become an important concern in public health, underlying the need to comprehensively investigate and understand the social determinants of health to foster equitable healthcare outcomes. This descriptive analysis examines the temporal and spatial patterns of social determinants of health in United States nursing homes from 2020 to 2023. Leveraging quarterly data obtained from the Centers for Medicare and Medicaid Services, the study provides an overview of key social drivers of health, including functional status, cognitive status, psychosocial factors, geriatric syndromes, and more. Through visual exploration, the study aims to elucidate trends and variations over time and across different regions. The analysis adopts a descriptive approach, emphasizing qualitative insights and policy considerations. This study contributes to a better understanding of the contextual factors influencing health outcomes in nursing homes, offering valuable insights for potential policy enhancements.
Keywords
Social determinants of health; Medicare; Health assessment; Public health
ORCID
https://orcid.org/0000-0003-3528-2354
Introduction
The aging population in the United States has brought a critical focus to the healthcare needs of individuals residing in nursing homes. As the demand for long-term care continues to rise, understanding the nuanced health and social determinants of this vulnerable population becomes increasingly essential. This study aims to explore the importance of performing assessments of residents in nursing homes, delving into their overall health status and potential social determinants and challenges they may face. In general, nursing homes serve as essential centers for the care of older adults, providing a spectrum of services to meet the diverse needs of residents. However, a nuanced understanding of the health landscape within these facilities goes beyond just medical diagnoses. It involves a thorough examination of the resident’s physical and mental well-being, encompassing their functional status, cognitive abilities, and the countless social determinants that shape their health outcomes. Recognizing the significance of this holistic approach, this study underscores the importance of regular assessments as a foundation for person-centered and equitable care.
An assessment of nursing home residents not only aids in identifying existing health conditions but also facilitates the early detection of potential issues, enabling timely and targeted interventions. This assessment could extend beyond traditional clinical measures to incorporate a consideration of social determinants, acknowledging the influence of factors such as socio economic status, living conditions, and social support networks on health outcomes. By integrating these other dimensions, health-care professionals can develop customized care plans that prioritize the unique needs and preferences of each resident.
In the subsequent sections, this paper will explore some of the social determinants of health variables relevant to nursing home residents considered in the analysis, high- lighting the importance of recognizing and addressing these factors for the delivery of high-quality and equitable care. Through a descriptive analysis, the paper seeks to contribute insights into the temporal and spatial patterns of social determinants within nursing homes from 2020 to 2023. Such an exploration is important for advancing our understanding of the complex interplay between health disparities and the diverse social determinants present in this vulnerable population.
Social determinants of health
Social Determinants of Health (SDOH) emerge as critical factors that influence individual’s well-being, encompassing the social, economic, and environmental conditions in which people live, work, and age [1,2]. Understanding and addressing SDOH is vital to delivering effective and equitable healthcare, especially in the context of vulnerable populations, such as those residing in nursing homes. At its core, SDOH encapsulates a diverse spectrum of elements, each intricately connected with an individual’s health trajectory. Economic stability, educational opportunities, social support networks, neighborhood environments, and access to healthcare services are some of these factors that collectively contribute to SDOH [2,3]. For individuals in nursing homes, where age and health vulnerabilities converge, understanding SDOH becomes very important. The impact of these determinants is amplified, shaping the residents’ over-all health outcomes and quality of life. From the financial resources available to them to the social connections within the facility, every facet of their well-being is intricately tied to the broader social determinants that define their environment. In addition, vulnerable populations often face systemic barriers rooted in social determinants, leading to unequal access to resources and healthcare [4]. Recognizing and addressing these disparities through the lens of SDOH is a fundamental step toward achieving health equity and ensuring that every individual in society, regardless of their background, has an opportunity to attain the highest level of health.
Health condition
The exploration of medical or clinical conditions within nursing homes holds important significance, especially when distinguishing between communicable and non-communicable diseases. These distinct categories of illnesses play important roles in shaping the health and targeted interventions for optimal care of nursing home residents. Communicable diseases pose a unique threat within nursing homes due to the communal living environment. Rapid transmission of infections can occur, affecting a significant portion of the vulnerable elderly population [5]. Investigating the prevalence and dynamics of communicable diseases is fundamental for implementing robust infection prevention and control measures [6]. On the other hand, non-communicable diseases also play a significant part in the healthcare landscape in nursing homes. Residents often suffer from chronic conditions such as cardiovascular diseases, diabetes, and respiratory disorders [7,8]. Investigating the prevalence and management of these diseases is indispensable for delivering effective, person-centered care. Taking into account the SDOH and overall health condition enables healthcare professionals to modify treatment plans, monitor disease progression, and enhance the overall quality of life for residents.
Health disparities in nursing homes
Over 15,000 certified Nursing Home (NHs) facilities housed about 1.2 million residents, according to a July 2022 report from the Centers for Medicare and Medicaid Services (CMS) [9]. For decades, care delivered in NHs has received significant policy attention due to the poor outcomes of care. These facilities are designed to provide care for the elderly, but they constantly face differences or challenges associated with health disparities. These differences show up in health outcomes and access to quality care, and they are often linked to factors like race, ethnicity, and socio economic status [10-12]. Studies reveal that residents from various racial backgrounds may experience distinct levels of care quality and health outcomes [13]. Economic disparities also play a role, making it harder for some residents to access quality services [14]. Furthermore, disparities are observed in areas like palliative and end-of-life care, where gaps in services impact nursing home residents differently [15]. It is essential to address these issues by promoting fairness, cultural understanding, and policies that break down barriers to healthcare access.
It is also essential to recognize that residing in a nursing home inherently becomes an important determinant of health for individuals. Residents of nursing homes experience a distinctive set of circumstances that distinguish them from non-residents, potentially leading to negative health impacts. Residential status itself serves as a critical determinant, influencing various aspects of health outcomes, access to care, and overall well-being. Factors such as the communal living environment, potential limitations in autonomy, and the prevalence of complex health conditions within nursing homes contribute to the unique health challenges faced by residents. Therefore, being a nursing home resident represents a distinctive determinant that necessitates specific attention in understanding and addressing the complexities of health disparities within this population.
Data
The data employed in this report originates from the Minimum Data Set (MDS), a standardized assessment tool required by the CMS for nursing homes throughout the United States [16]. This assessment captures a ironic array of aging-relevant domains, providing a detailed snapshot of residents’ functional and cognitive status, psychosocial functioning, geriatric syndromes, and others. In addition, we examine both communicable and non-communicable diseases within nursing homes. This dataset proves invaluable for researchers seeking to understand function and disability on a large scale in vulnerable older adults. The goal here is to analyze data spanning the years 2020 to 2023, capturing an overview of health and social determinant trends over this period. The quarterly nature of the assessments allows for a detailed exploration of temporal patterns, offering insights into how various factors evolve within the nursing home population.
Materials and Methods
Temporal mapping is employed to visualize and explore the patterns of social determinants over time within the United States nursing home population. This technique involves the creation of temporal maps that illustrate the changing landscape of social determinants across quarters. These maps provide a dynamic representation of trends and variations, allowing for a nuanced understanding of how social determinants evolve within the context of long-term care. The construction of these multiple maps focuses on different dimensions of SDOH and overall health. For instance, a diverse range of SDOH includes demographic factors, social support networks, cognitive and mental health indicators, functional status, nutritional status, health behaviors, cultural backgrounds, and healthcare service utilization. The goal is to create a comprehensive picture of the nuanced factors influencing residents’ health outcomes. Additionally, temporal maps tracking the frequencies of some communicable and non-communicable diseases over time will be generated, clarify on the prevalence and patterns of specific health conditions within the nursing home population. To measure the overall health outcome, the study will utilize life expectancy as a key metric, offering valuable insights into the duration of residents’ health while in the nursing home setting. If staff from the nursing homes believes the residents have a possibility of returning to the community, then this will be captured as well, particularly as a social outcome. This approach aims to capture the intricate interplay of various determinants and health indicators, contributing to a holistic understanding of the health landscape in nursing homes. All visualizations were generated using the R statistical software [17], particularly the R packages ggplot2 [18], for the mapping creation, and tidycensus [19] to get the geometry features of the boundaries of the United States map and each state.
Results
Each MDS dataset contains 605 features (items) associated with different dimensions, such as social, demographic, clinical, and psychological factors, that could be used for health assessment or research. For this exploratory analysis, we focused on a sub-set of these features to motivate other researchers and health disparity experts to fully analyze and deeply investigate the vulnerability of the nursing home population and what drives their health to deteriorate. As indicated in previous sections, the main categories for this exploration are:
1. Social determinants of health;
2. Non-communicable diseases;
3. Communicable diseases;
4. Healthcare services; and
5. Indicators of the nursing population’s overall health.
For each map, we present the percentage (0%-100%) represented according to the feature chosen. Due to the numerous maps generated for this exploratory analysis, all visualizations have been included as supplementary materials in the GitHub repository. To aid in the comprehension of this paper, alongside the supplementary files, we provide the corresponding file names for each featured visualization. The R code used to produce the visualizations is also provided within the repository.
Social determinants of health
Examining the spatial distribution of male and female residents (Social Feature 1) across each quarterly data from 2020 to 2023, we observed that nearly 75% of residents in the Midwestern region and the Caribbean are female. In contrast, the Western region of the United States exhibits a more balanced representation, with a comparable percentage of males and females residing in nursing homes. Based on the race/ethnicity categorization in the CMS data (Social Features 2 to 7), the U.S. Virgin Islands consistently demonstrates a higher proportion of nursing home residents identified as Asian throughout the study timeframe. In the Southeast region, several states consistently exhibit a higher percentage of nursing home residents identified as black or African American. When considering Hispanic/ Latino representation, it becomes evident that the Caribbean, particularly Puerto Rico, as well as the West and Southwest regions, exhibit a higher percentage within the nursing home population. The Northwest region displays a higher proportion of nursing home residents identified as white. These findings highlight the diverse demographic compositions of nursing home populations across different geographic areas, emphasizing the importance of considering regional variations in healthcare planning and provision. Understanding these spatial patterns is essential for modifying interventions and care strategies to meet the specific needs of residents in various regions and from diverse backgrounds.
In terms of reasons for admission to nursing homes, our analysis highlights notable patterns in certain states. Specifically, Wisconsin in the Midwest and Idaho, Utah, Wyoming, and Colorado in the Northwest and Southwest regions exhibit slightly higher percentages of residents being admitted due to serious mental illnesses (Social Feature 9). This discrepancy underscores the importance of examining state-specific factors and nuances in healthcare policies that contribute to divergent admission patterns. The Brief Interview for Mental Status (BIMS) is a mandatory tool used to screen and identify the cognitive condition of residents upon admission into a long-term care facility [20]. The total BIMS score ranges between 0 to 15 points and is categorized into three cognitive groups: Intact, Moderate, and Severe. The objective of a BIMS assessment is not to diagnose cognitive illnesses like dementia or Alzheimer’s but rather to assist facility staff with detecting early symptoms and the potential need for further evaluation. The CMS data (Social Feature 12) shows that between 45%-55% of the nursing residents per state show intact to borderline cognitive impairment with Puerto Rico in the upper 70%. In addition, more than 60% of the residents per state are not feeling depressed (Social Feature 13). However, some states in the Northwest and Midwest regions show residents expressing mild to moderate depression, respectively. These patterns are observed over each year from 2020 to 2023.
Activities of Daily Living (ADLs) encompass the personal tasks integral to our daily lives. As dementia advances, there is a natural decline in ADL skills, leading to an increased need for caregiver involvement over time. In adult day services programs, clients typically require less assistance with ADLs compared to individuals in other long-term care settings, particularly in activities such as bathing, dressing, and toileting [21,22], or when addressing estate and legal matters [23]. The CMS data reveals a consistent trend over the four years (Social Feature 16), indicating that over 50% of nursing home residents require extensive assistance with personal hygiene.
Another important factor we explored was psychiatric and mood disorders. For instance, the percentage of residents per state showing anxiety disorders (Social Feature 22) and depression (Social Feature 23) are at around 25%-30% and 50%-60%, respectively, over time. In regards to social support, the data shows that more than 60% of nursing home residents per state do not have participation from family, significant others (Social Feature 29), or legal guardians (Social Feature 30). In Puerto Rico, for instance, this percentage is lower, potentially indicating more participation from family members, significant others, or legal guardians, but due to missing data issues, this might not hold as true.
Communicable diseases and non-communicable diseases
Upon examining the distribution of cancer diagnoses (Non- Communicable Disease Feature 1) across nursing homes in the United States, the CMS data shows that the majority of nursing home residents do not have an active cancer diagnosis. When investigating the proportion of residents with hypertension (Non-Communicable Disease Feature 5), the CMS data reveals that most nursing homes have over 60% of residents suffering from hypertension. Regarding Diabetes Mellitus (Non- Communicable Disease Feature 7), the percentage of residents suffering from it varies between 25% and 40% for most states. The data on communicable diseases is significantly impacted by missing information, severely constraining the ability to interpret patterns per state and time.
Healthcare services
Among the various healthcare services rendered within nursing homes, analysis of the CMS data reveals that over 70% of nursing home residents report receiving no days of antianxiety medication (Services Feature 2) and no days of antibiotics (Services Fea- ture 4). In the case of antidepressant medications (Services Feature 3), a balance is observed, with approximately 50% of residents indicating either 0 or 7 days of administration. It is important to mention that the state of California and the United States territory of Puerto Rico, exhibit higher percentages for 0 days of administration compared to the rest of the states or regions. Administering the influenza vaccine (Services Feature 6) is essential for nursing home residents due to their increased vulnerability to severe complications from influenza such as age-related immune system weakening and underlying health conditions. The CMS data reveals that the vast majority of nursing home residents across the states and years have received the vaccine, with particularly noteworthy percentages observed in the center and northern regions of the country. On the other hand, in Puerto Rico, the percentage of no influenza vaccine administration is very high, but due to missing data issues, this might not be the real pattern.
Overall health status
Within the diverse features in the dataset, life expectancy at 6 months (Status Feature 1) and the assessment of returning to the community (Status Feature 2) were prioritized for an overall health assessment. Notably, the majority of nursing home residents per state are not anticipated to return to the community but are projected to have a life expectancy exceeding 6 months.
Discussion
This analysis of nursing home data obtained from the CMS provides valuable insights into the health landscape of residents across the United States. We uncovered nuanced patterns that clarify on the multifaceted nature of healthcare within these facilities. Notably, the examination of non-communicable diseases revealed variations in disease prevalence, emphasizing the importance of customized interventions for different regions. The prevalence of infectious diseases, while limited in available data, underscores the necessity for a more comprehensive exploration within nursing homes. Furthermore, the data about healthcare services within nursing homes highlighted intriguing patterns in medication usage. The majority of residents report no days of antianxiety or antibiotic medication, showcasing potential trends in prescription practices. The data also shows high influenza vaccination rates, particularly in the northern regions of the country. The analysis also considered broader aspects of residents’ well-being, such as life expectancy and the likelihood of returning to the community. These factors play a pivotal role in shaping the overall health trajectory of nursing home residents. While a significant percentage of residents are not expected to return to the community, the majority exhibit a life expectancy beyond 6 months.
However, this exploratory analysis encountered several limitations, primarily stemming from data constraints. Notably, a considerable number of feature percentages were found to be missing (colored gray in maps) for various states in the United States. across numerous quarters. Missing data poses a challenge to the evaluation of SDOH, potentially leading to gaps in the understanding of regional patterns and trends. The absence of this information may limit the ability to conclude the states affected by missing feature percentages. Therefore, caution should be exercised in making broad generalizations or definitive statements about the states with incomplete data, and future analyses may benefit from efforts to address and mitigate these missing values. Another noteworthy limitation is the limited inclusion of infectious diseases (communicable diseases) in the CMS data. Recognizing the critical importance of infectious diseases in healthcare settings, particularly nursing homes, highlights the need for a more comprehensive exploration of this aspect. Further research and data collection on a broader spectrum of infectious diseases among the population in United States. nursing homes is essential to enhancing our understanding and developing effective strategies to address and prevent communicable diseases within these healthcare settings. The data on communicable diseases was significantly impacted by missing information, severely constraining the ability to interpret patterns per state and time.
Building upon the current analysis, there are several encouraging avenues for future research in the province of nursing home health disparities and healthcare services. One direction involves a deeper look into the specifics of infectious diseases within nursing homes, including prevalence, management strategies, and the impact of vaccination efforts, which could significantly contribute to the understanding and mitigation of the risks associated with infectious diseases in these settings. Additionally, a longitudinal analysis could provide valuable insights into the temporal trends of health disparities among nursing home residents. Examining changes over time could uncover evolving patterns, contributing to a more dynamic understanding of healthcare delivery and outcomes within these facilities. Furthermore, investigating the correlation between healthcare service patterns and resident outcomes holds the potential to provide critical insights. Understanding how variations in medication usage or specific healthcare services related to health outcomes and quality of life for nursing home residents would be essential for optimizing care strategies and improving overall well-being. Achieving health equity requires addressing social determinants of health, promoting access to healthcare services, and dismantling systemic barriers that contribute to unequal health outcomes. Ultimately, the goal is to create a healthcare system and societal conditions that prioritize fairness, inclusivity, and the highest possible standard of health for all individuals.
Conclusion
This exploratory analysis of nursing home data from the CMS provides valuable insights into the complex landscape of healthcare within these facilities across the United States. The examination of various dimensions, including social determinants of health, communicable and non-communicable diseases, healthcare services, and overall health status, reveals nuanced patterns and disparities that warrant further investigation. Notably, variations in disease prevalence and medication usage underscore the need for customized interventions and a more comprehensive exploration of healthcare practices within nursing homes. The high influenza vaccination rates observed, particularly in certain regions, highlight successful preventive measures but also point to potential disparities in vaccine access and administration.
Despite the valuable insights gained, this exploratory analysis encountered limitations, primarily due to missing data and the limited inclusion of infectious diseases in the CMS dataset. Addressing these limitations and conducting further research is essential for a deeper understanding of nursing home health disparities and the development of effective strategies to improve resident outcomes. Future research directions may include a more comprehensive exploration of infectious diseases, a longitudinal analysis of health disparities, and an investigation into the correlation between healthcare service patterns and resident outcomes. Ultimately, achieving health equity for nursing home residents requires addressing social determinants of health and dismantling systemic barriers to ensure fair and inclusive healthcare for all. This work contributes to this broader goal and sets the stage for continued efforts to optimize care strategies and improve overall well-being in nursing home settings.
Declarations
Ethics approval and consent to participate
While the MDS dataset contains information about residents’ health status, it does not contain any subject-level information that could be used to identify specific individuals. The dataset was de-identified by the CMS to protect the privacy of nursing home residents, and state-level counts are presented instead. The Indiana University Human Research Protection Program (HRPP) staff determined the analysis done in this study is not human subject research and did not require further Institutional Review Board (IRB) review before conducting the study.
Data availability statement
All the data used for this study is freely and publicly available on the CMS website.
Declaration of conflicting interests
The author declares no competing interests.
Open access
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons License, and indicate if changes were made. The images or other third-party material in this article are included in the article’s Creative Commons License, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons License and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit: http://creativecommons.org/licenses/by/4.0/.
References
- Health C. Closing the gap in a generation: Health equity through action on the social determinants of health: final report of the commission on social determinants of health. World Health Organization. 2008.
- Organization WH. Social determinants of health. 2008.
- Beech BM, Ford C, Thorpe Jr RJ, Bruce MA, Norris KC. Poverty, racism, and the public health crisis in America. Frontiers in public health. 2021;9:699049.
- Alexander GL, Liu J, Powell KR, Stone PW. Examining structural disparities in US nursing homes: National survey of health information technology maturity. JMIR aging. 2022;5(3):e37482.
- Strausbaugh LJ, Sukumar SR, Joseph CL, High KP. Infectious disease outbreaks in nursing homes: An unappreciated hazard for frail elderly persons. Clin Infect Dis. 2003;36(7):870-876.
- Rubano MD, Kieffer EF, Larson E. Infection prevention and control in nursing homes during COVID-19: an environmental scan. Geriatr Nurs. 2022;43:51-57.
- McNabney MK, Onyike C, Johnston D, Mayer L, Lyketsos C, Brandt J, et al. The impact of complex chronic diseases on care utilization among assisted living residents. Geriatr Nurs. 2014;35(1):26-30.
- Bekhet AK, Zauszniewski JA. Chronic conditions in elders in assisted living facilities: Associations with daily functioning, self-assessed health, and depressive symptoms. Arch Psychiatr Nurs. 2014;28(6):399-404.
- CMS. Centers for Medicare and Medicaid Services. 2024.
- Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: Racial segregation and disparities in quality across US nursing homes. Health Aff. 2007;26(5):1448-1458.
- Azar KM, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California: Study estimates the COVID-19 infection fatality rate at the US county level. Health Aff. 2020;39(7):1253-1262.
- Dictus C, Cho Y, Baker T, Beeber A. Racial and ethnic disparities in pain management for nursing home residents: A scoping review. Innovation in Aging. 2021;5(1):878.
- Werner RM, Konetzka RT. Trends in post–acute care use among Medicare beneficiaries: 2000 to 2015. Jama. 2018;319(15):1616-1617.
- Riley WJ. Health disparities: Gaps in access, quality and affordability of medical care. Trans Am Climatol Clin Assoc. 2012;123:167.
- Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. Jama. 2013;309(5):470-477.
- Poverty, racism, and the public health crisis in America. Frontiers in public health
- Team RC. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2022.
- Wickham H. Ggplot2: Elegant graphics for data analysis. Springer. 2016.
- Walker K, Herman M. Tidycensus: Load us census boundary and attribute data as ’tidyverse’ and ’sf’-Ready Data Frames. 2022.
- Saliba D, Buchanan J, Edelen MO, Streim J, Ouslander J, Berlowitz D, et al. MDS 3.0: brief interview for mental status. J Am Med Dir Assoc. 2012;13(7):611-617.
- Jordan S, Gabe M, Newson L, Snelgrove S, Panes G, Picek A, et al. Medication monitoring for people with dementia in care homes: the feasibility and clinical impact of nurse-led monitoring. Sci world J. 2014;2014.
- Singh P, Lu Z, Sengupta M. Variation in adult day services center participant characteristics by center ownership: United States. National Center for Health Statistics. 2022.
- DeFina PA, Moser RS, Glenn M, Lichtenstein JD, Fellus J. Alzheimer's disease clinical and research update for health care practitioners. J Aging Res. 2013.
Citation: Pabon-Rodriguez FM (2024) Assessment of Health Outcomes and Social Determinants of Health in United States Nursing Homes. J Socialomics. 13:227.
Copyright: © 2024 Pabon-Rodriguez FM. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.