Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 5, Issue 2
Anesthetic Considerations and Perioperative Optimization of a Patient with Hereditary Hemorrhagic Telangiectasia in the Ambulatory Surgical Setting: A Case Report
Archana S. Hudson* and The-Hung Edward NguyenReceived: 29-Jan-2021 Published: 22-Feb-2021, DOI: 10.35248/2684-1606.21.5.142
Abstract
Hereditary Hemorrhagic Telangiectasia (HHT), also known as Osler-Weber-Rendu Syndrome, is a rare autosomal dominant disorder characterized by multiple systemic Arteriovenous Malformations (AVMs) which presents unique challenges and considerations for the anesthetic management during the perioperative period. Patients with HHT are not typically considered appropriate candidates for outpatient surgery centers due to their high risk of complications relating to these AVMs, including a higher incidence of symptomatic anemia, paradoxical air embolus and/or bacteremia due to pulmonary AVMs, congestive heart failure, portal hypertension, seizures, and intracranial hemorrhage. We present a case of a 55 year-old male with known history of HHT who presented to our outpatient surgery center for intranasal mass injection/excision and septodermoplasty. Extensive planning and optimization was performed by our center for perioperative optimization, including coordination with hematology, cardiology, pulmonology, and obtaining proper imaging to rule out significant pulmonary or cerebral AVMs prior to proceeding. The patient underwent general anesthesia with an unremarkable perioperative course, and did well in recovery without any bleeding complications. The patient with HHT can safely undergo surgery in the outpatient surgery setting with proper patient selection, preoperative coordination and optimization.Keywords
Anesthesia; Surgery; Perioperative optimization; Septodermoplasty; Osler-Weber-Rendu syndrome
Abbrevations
HHT: Hereditary Hemorrhagic Telangiectasia; AVMs: Arteriovenous Malformations; ASCs: Ambulatory Surgery Centers; TXA: Tranexamic Acid; CPO: Center for Perioperative Optimization
Introduction
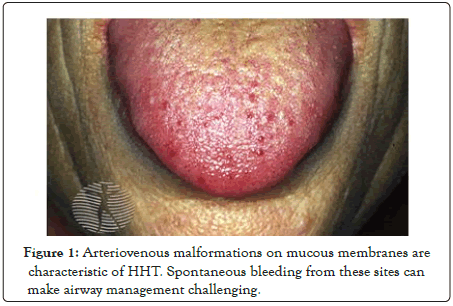
Beginning in the 1980’s, there has been a trend toward more surgeries being performed at ambulatory surgery centers (ASCs) [1]. From the period of 1996 to 2006, there was a 300% increase in procedures performed at free-standing ASCs, while today over 60% of all surgeries performed in the US occur in the outpatient surgical setting [2]. That number is only expected to grow over the next decade. The trend has been for both higher volumes and more complex cases to be done on an outpatient basis. Advances in patient selection algorithms and the development of perioperative optimization clinics have allowed for more surgeries to be safely performed in ASCs with minimal complications and low rates of morbidity and mortality [3,4]. Patients with rare conditions that present anesthetic and surgical challenges are often assumed to not be appropriate for the outpatient surgery setting. However, with proper planning and multidisciplinary coordination, these patients can often safely undergo surgery in the outpatient surgical setting with similar outcomes in comparison to the traditional inpatient setting [5]. Hereditary Hemorrhagic Telangiectasia (HHT) is a genetic condition that causes congenital Arteriovenous Malformations (AVMs) throughout the body, including in the GI tract, nasal mucosa, liver, lungs, brain, and spinal cord to name a few. Perioperative anesthetic concerns for patients with HHT include severe chronic anemia due to AVMs of the GI tract, refractory epistaxis, difficult airway due to bleeding, paradoxical embolus and significant V/Q mismatch due to pulmonary AVMs, portal hypertension and/or congestive heart failure secondary to hepatic AVMs, and neurologic manifestations including seizures, paralysis, and even intracerebral hemorrhage and death due to cerebral AVMs [6,7]. These patients are typically managed with long term iron supplementation and antifibrinolytics such as Tranexamic Acid [8]. In this case report, we present an otherwise healthy 55 year-old male with a known history of HHT who was scheduled to have nasal septodermoplasty for recurrent episodes of epistaxis and nasal mucosa destruction. He was seen preoperatively in our institution’s perioperative optimization center in collaboration with multiple specialists prior to his scheduled surgery (Figure 1).
Figure 1: Arteriovenous malformations on mucous membranes are characteristic of HHT. Spontaneous bleeding from these sites can make airway management challenging.
Case Presentation
A 55 year-old ASA-3 male with known history of HHT, chronic anemia (baseline hemoglobin ~ 7.1 g/dL), mild thrombocytopenia (baseline ~ 162,000/uL), hypertension, and hypercholesterolemia presented to our outpatient surgery center for nasal septodermoplasty due to history of chronic daily epistaxis refractory to conventional treatments. He was seen in our institution’s Center for Perioperative Optimization at the request of his surgeon. The patient’s care was coordinated with his cardiologist, pulmonologist, and hematologist. He had followed with hematology for years, requiring multiple rounds of IV iron infusion, with his hemoglobin ranging from 7-13 g/dL. For the procedure, hematology recommended he continue oral Tranexamic Acid (TXA) and receive two rounds of IV iron infusion no more than 3 weeks prior to surgery. Cardiology recommended he undergo right-sided heart catheterization to rule out significant pulmonary AVMs and pulmonary hypertension. Pulmonology ordered pulmonary function testing, which revealed only a mild obstructive ventilatory defect and normal gas transfer. He also underwent intracranial imaging to rule out significant brain AVMs.
On the morning of surgery, the patient took his oral TXA and received oral acetaminophen 1000 mg as per multimodal analgesic protocol. The patient’s intraoperative course was unremarkable. He underwent induction of general anesthesia using a combination of propofol, lidocaine, fentanyl, and rocuronium and was intubated orally without difficulty. Anesthesia was maintained using inhaled sevoflurane. Prior to emergence, nasal cavity was packed by surgeons and patient was extubated after meeting appropriate criteria. He spent a total of approximately 2 hours in PACU, with minimal pain, nausea, or bleeding issues. The patient had an unremarkable post-operative course without any bleeding complications and was discharged home later that day.
Results and Discussion
The conventional wisdom in medicine has long been that medically complex, challenging patients are not typically appropriate for surgery at ASCs. Although not without merits, this approach to patient care excludes a substantial percentage of patients as candidates for ambulatory surgery, potentially leading to higher costs, longer PACU and hospital length-of-stay, and poorer resource utilization [3,5]. In recent years, interest has grown in the concept of a pre-operative or perioperative optimization assessment prior to surgery, allowing for risk-stratification and best-practice implementation for medically complex patients having a wide range of surgeries. This concept has allowed for patients with multiple comorbidities and rare diseases to undergo surgical procedures with an increased emphasis on ambulatory and same-day models [4]. At our institution, many of our more complex patients are referred to the Center for Perioperative Optimization (CPO), where they are seen by an Advanced Practice Clinician (APC) or physician, who performs a thorough history, physical, and review of the medical record to assess how to best optimize the patient for their planned surgery. The optimization plan relies on a multidisciplinary approach, emphasizing communication and follow-up with a wide range of specialists and consultants to formulate a plan for the day of surgery that incorporates best practices and Evidence-Based Medicine (EBM).
Patients with HHT are at higher risk for chronic anemia, heart failure, pulmonary hypertension, seizures, hemorrhagic stroke, air embolism, and massive bleeding. We present an otherwise healthy 55 year-old male with a history of symptomatic HHT causing chronic iron deficiency anemia and severe recurrent epistaxis, requiring multiple prior surgeries of the nasal septum. The patient was followed by hematology and was managed on a regimen of IV iron infusions and oral TXA. Due to the potential for intraoperative and postoperative bleeding complications, plus the elevated risk of the patient having sequelae from intracranial, pulmonary, GI, or hepatic AVMs, this patient would not typically be considered appropriate for ambulatory surgery. Instead of excluding him from our ambulatory surgery center, the patient was referred to our CPO, which performed a detailed assessment and risk stratification process, reviewing prior imaging studies such as head CT, chest CT, echocardiography, right-sided heart catheterization, endoscopy procedures, and blood work. A thorough review of the data revealed that the patient did not have clinically significant AVMs outside of his nasal septum and that he did not have pulmonary hypertension or heart failure. The patient’s hematologist recommended continued IV iron infusion to maintain an adequate pre-operative hemoglobin and to continue his oral TXA the morning of surgery to reduce risk of bleeding. The patient’s cardiologist and pulmonologist did not make any specific recommendations for the planned procedure but did not note that the patient’s perioperative risk was acceptable and that surgery in the ambulatory setting should proceed. The plan was communicated with the anesthesia and surgical teams prior to surgery, and the patient underwent the procedure without intraoperative or postoperative complication. Without proper optimization, planning, and risk stratification, the patient may have otherwise had significant complications or sustained costly hospital admission.
Conclusion
We present a case of a patient with symptomatic HHT who was deemed appropriate for and underwent complex nasal septum surgery in our ambulatory surgery center and was discharged home later that day without complication. The Perioperative Optimization Center at our institution allowed for appropriate risk stratification, patient selection, and a coordinated multidisciplinary approach to optimization of the patient prior to surgery. Though he had a rare disease not often seen in patients undergoing outpatient surgery, the patient received appropriate anesthetic care and avoided unnecessary and costly hospital admission, reducing both healthcare costs and potential complications. This case demonstrates the importance and utility of preoperative planning and optimization, which can allow even the most medically complex of patients to safely undergo most types of surgery in the ambulatory setting with similar outcomes when compared to the traditional inpatient setting.
REFERENCES
- National Center for Health Statistics. Hospital Admissions, Average Length of Stay, Outpatient Visits, and Outpatient Surgery by Type of Ownership and Size of Hospital: United States, Selected Years 1975–2008. National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology, Table 104
- Cullen K, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009; 11: 1-25.
- Agency for Healthcare Research and Quality. Hospital-based ambulatory surgery.
- Fong R, Sweitzer BJ. Preoperative optimization of patients undergoing ambulatory surgery. Curr Anesthesiol Rep. 2014; 4: 303–315.
- Mathis MR, Naughton NN, Shanks AM, Freundlich RE, Pannucci CJ, Chu YJ, et al. Patient selection for day case-eligible surgery: Identifying those at high risk for major complications. Anesthesiology. 2013; 119: 1310–1321.
- Robinson D, Rogers B, Kapoor R, Swan J, Speas G, Gutmann R. Anesthetic considerations for a patient with hereditary hemorrhagic telangiectasia (osler-weber-rendu syndrome) undergoing a five-box thoracoscopic maze procedure for atrial fibrillation. J Investig Med High Impact Case Rep. 2014; 2: 2324709614553669.
- Weingarten TN, Hanson JW, Anusionwu KO, Moncrief ML, Opdahl TJ, Schneider DD, et al. Management of patients with hereditary hemorrhagic telangiectasia undergoing general anesthesia: A cohort from a single academic center's experience. J Anesth. 2013; 27: 705-711.
- Chin CJ, Rotenberg BW, Witterick IJ. Epistaxis in hereditary hemorrhagic telangiectasia: An evidence based review of surgical management. J Otolaryngol Head Neck Surg. 2016: 45: 3.
Citation: Hudson AS, Nguyen THE (2021) Anesthetic Considerations and Perioperative Optimization of a Patient with Hereditary Hemorrhagic Telangiectasia in the Ambulatory Surgical Setting: A Case Report. J Surg Anesth. 5:142.
Copyright: © 2021 Hudson AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.