Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2024) Volume 8, Issue 1
Anesthesia Management in a patient with Berardenilli-Seip Congenital Lipodystrophy (BSCL) Scheduled for Open Reduction and Internal Fixation of Femur
Sami Ur Rehman*, Ahmad Farooq, Arshad Taqi and Ayesha AsadReceived: 23-Dec-2023, Manuscript No. JSA-23-24509; Editor assigned: 27-Dec-2023, Pre QC No. JSA-23-24509 (PQ); Reviewed: 17-Jan-2024, QC No. JSA-23-24509; Revised: 24-Jan-2024, Manuscript No. JSA-23-24509 (R); Published: 01-Feb-2024, DOI: 10.35248/2684-1606.24.8.235
Abstract
We are presenting our case of the patient with Berardinelli-Seip Congenital Lipodystrophy (BSCL), characterized by hyperinsulinemia caused by insulin resistance combined with lipodystrophy and acromegaloid features. This patient had portal vein thrombosis, prognathosis, hypertrophic obstructive cardiomyopathy, (Left Ventricular Outflow Tract) LVOT obstruction, hyperthyroidism, hypertension and diabetes mellitus. He underwent Open Reduction and Internal Fixation (ORIF) with titanium elastic plates under spinal anesthesia.
Keywords
Berardinelli-Seip congenital lipodystrophy, LVOT obstruction, Lipodystrophy, Acromegaloid features, Hyperinsulinemia, Insulin resistance
Introduction
Berardinelli-Seip Congenital Lipodystrophy (synonyms: Congenital generalized lpodystrophy/Berardinelli-Seip Syndrome/ Seip-Lawrence syndrome/Lipodystrophy acromegaloid gigantism syndrome/Lipoatrophic diabtes) was first reported in 1954 in Brazil by Waldemar Berardinelli in a 2 year old boy and later in 1959 by Martin Seip in three patients [1,2]. Its prevalence worldwide is estimated to be 1 in 12 million people [3]. This disease is inherited as an autosomal recessive trait, with parental consanguinity as the main factor [1].
Berardinelli-seip syndrome is featured by lack of adipose tissue with resultant dysregulation in carbohydrate and lipid metabolism. These patients have low serum leptin and adiponectin levels. They usually have elevated circulating serum triglycerides (very-low-density lipoproteins plus chylomicrons) and develop severe steatosis within their lean organs, such as the liver and skeletal muscles [4,5]. Two key metabolic features are much- increased gluconeogenesis along with much-decreased insulin-mediated skeletal muscle glucose uptake. Usually, by the 2nd decade of life, they develop type 2 diabetes requiring very high insulin doses. Hypertriglyceridemia in these patients is very difficult to treat, and it may manifest itself as cutaneous xanthomas. The criteria for labelling a patient being suffering from Berardinelli-Seip Congenital Lipodystrophy (BSCL) consists of a major criteria (Lipoatrophy affecting the trunk, limbs, and face; Acromegaloid features; Hepatomegaly; Elevated serum concentration of triglycerides(upto 80 g/dl); Insulin resistance(elevated serum concentrations of insulin and C-peptide and clinically as acanthosis nigricans)) and a minor criteria (Hypertrophic cardiomyopathy; Psychomotor retardation or mild (IQ 50-70) to moderate (IQ 35-50) intellectual impairment; Hirsutism; Precocious puberty in females; Bone cysts occur in 8%-20% of affected individuals and have a polycystic appearance on x-ray; Phlebomegaly) [6]. The best current treatment for CGL is recombinant leptin, but this is not widely available [5].
We were able to find only two case reports on anesthesia management of patients with Berardinelli-Seip Syndrome, tonsillectomy and dental extraction, both of which were under general anesthesia [7,8]. There was unexpected delayed emergence in dental extraction case report [8]. We have obtained permission and written informed consent from the patient's father presented in this case report.
Case Presentation
A 12 year-old-boy (50 kg weight, height of 147 cm) presented for ORIF of femur following the fracture of left shaft of femur. He had delayed achievement of developmental milestones. At the age of 5 years, diagnosed with hypertension (Took atenolol for it but from last one year not taking), Diabetes Mellitus from the last 6 years (Using Lantus Insulin 30 units in the morning, Novorapid 30 units in the evening and Metformin 500 mg once-a-day. He was hyperthyroid (Taking Propranolol 5 mg twice-a-day and thyroxin 50 mg once-a-day) and parents had given the history of portal vein thrombosis, with documented record missing. On physical examination; there is prognathic jaw, Macroglossia, Palatine tonsils hypertrophy, acanthosis nigricans in neck, axillary and groin region, frontal bossing, muffled speech, follows commands and cooperative (Figure 1). On systemic examination, there was mid-systolic murmur and distended abdomen. Echocardiography stated hypertrophic obstructive cardiomyopathy, severe concentric Left Ventricular Hypertrophy (LVH), Ejection fraction of 67%, Left ventricular Outflow-Tract (LVOT) dynamic obstruction with PG 68-77 mmHg, Grade1 diastolic dysfunction and grade 1-2 mitral regurgitation. On Electrocardiogram (ECG), there is Q-wave in lead 3 and T-wave inversion in lead 1, aVL, V4, V5 and V6. His lab reports showed a platelet count of 88000 and serum total bilirubin 2.75 mg/dl and INR 1.66, with all other reports in normal range. Abdominal ultrasound state hepato- spleenomegaly, distended gall-bladder, enlarged kidneys and debris in urinary bladder. We had advised to continue propranolol and thyroxine, and to skip insulin on the morning of day of surgery. We had arranged 2 Fresh Frozen Plasma (FFP’s) keeping in mind the INR.
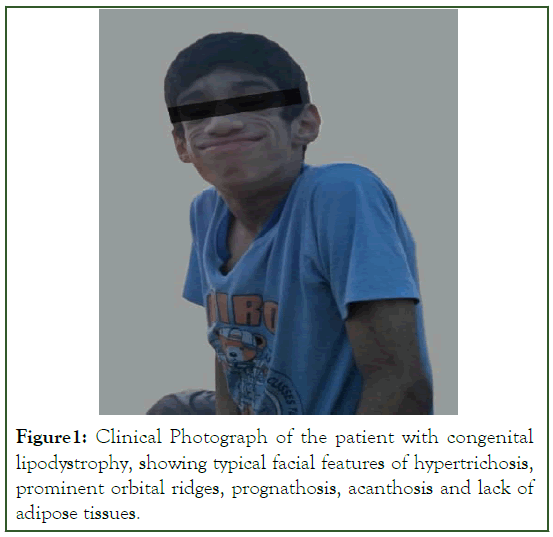
Figure 1: Clinical Photograph of the patient with congenital lipodystrophy, showing typical facial features of hypertrichosis, prominent orbital ridges, prognathosis, acanthosis and lack of adipose tissues.
After taking informed consent from parents and a cardiologist on-board, patient was shifted to Operation Theater (OT) after taking a wide-bore IV cannula. One FFP was transfused in pre-op before shifting and the other one transfused on OT table just before subarachnoid block (SAB). On OT-table, left lateral position was made after giving 1 mg of midazolam and 30 mg ketamine intravenously. Ringer Lactate fluid was started@90 ml/hour and propofol infusion@100 mg/hour intravenously. Unilateral subarachnoid block was performed in left lateral position@L4-L5 level with a 27G Pencil point needle and 0.75%Bupivacaine 7.5 mg (1 ml) injected after conformation of free flow of CSF. After 7 minutes, supine position was made. Face mask attached@5 LO2/min and standard monitoring was done with ECG, Pulse oximetry, BP, temperature and EtCO2. Total duration of surgery was 1 hour and 30 minutes and the propofol infusion was stopped at the end of procedure. Total fluid given during intra-operative course was 150 ml and estimated blood loss was minimal (only about 20 ml to 30 ml).
Patient was shifted to Post-Operative Care Unit (PACU) with stable vitals, fully awake, responding to vocal commands, maintaining saturation of 97%@room air and modified bromage score of 3 and a folley’s catheter in situ. He had unremarkable postoperative time and was discharged after 5 hours after removing folley’s catheter with modified bromage score of 0 and Post-Anesthesia discharge score of 9. Before discharge, informed consent regarding the publication of case report was signed by the father.
Discussion
Berardenilli-Seip Congenital Lipodystrophy has at least four types: Type 1, due to mutations in the AGPAT2 gene; Type 2, due to mutations in the BSCL2 gene; Type 3, due to mutations in the CAV1 gene; and Type 4, due to mutations in the Polymerase I and Transcript-Release Factor [PTRF] gene [2]. 95% of the patients with BSCL have either a mutation in AGPAT2 or BSCL2 gene [1]. Type4 BSCL have Cav3 gene deficiency (Cav3 has role in Ca+2 and RYR gene). These patients are considered at risk of developing Malignant Hyperthermia (MH) [6].
Keeping in mind the LVOT dynamic obstruction, general anesthesia is usually preferred over spinal anesthesia for stabilization of circulatory dynamics. As postulated in one of the case report that the absence of adipose tissue resulted in the brain being disproportionately affected by anesthetic agent, so it is advisable to avoid highly fat-soluble anesthetic agents [8]. As our patient had lipodystrophy and having one case report of delayed emergence from general anesthesia in BSCL, we opted for low dose unilateral spinal anesthesia to avoid excessive sympathectomy and higher level of block; hence avoiding the hemodynamic instability and maintaining a fix-gradient across LVOT. In HCOM, decrease preload and afterload; and increased myocardial contractility can worsen LVOT obstruction and decreases cardiac output. So, care should be taken to maintain intravenous volume and phenylephrine infusion should be in-hand for hypotension guided by invasive monitoring. In our case, preoperative and intraoperative hemodynamics remained same, maintaining the gradient across LVOT, with an uneventful intraoperative course.
In general, patients having lipodystrophy, triglyceride levels should be maintained by restricting the dietary fat to 20%-30% of total energy. Based on patient’s weight, estimated calorie requirement was 1500 kcal; with ideal lipid intake of 43 g-64 g [9]. We calculated that if we use propofol 1 mg/kg-2 mg/kg for induction and 4 mg/kg-12 mg/kg/hr for maintenance of anesthesia, then the amount of lipid intake would be higher than the calculated limit. As we were using intravenous mode of administration, actual lipid intake would be higher than oral intake. The amount of propofol that we had used for sedation in this patient was at very low rate, making only up to 0.15 g for the whole duration of surgery [10,11]. But in hindsight, we will recommend the use of dexmedetomidine for sedation and also for induction of anesthesia where needed, so as to avoid lipid containing drugs as much possible.
Conclusion
Given the rarity of syndrome, hope this case report will provide a precedent for the anesthesia management of patients with BSCL and a means to quickly decide regarding anesthetic management. This case report describes that patients with Berardenilli-Seip Congenital Lipodystrophy are at increased risk of Malignant Hyperthermia. As these patients have LVOT obstruction, preload and afterload should be maintained. And most importantly, lipid soluble drugs should be used as cautiously as possible.
Acknowledgement
This case report completion wouldn't have been possible without the supervision of my seniors. And most of all to our Almighty creator, the creator of knowledge and wisdom, who made this possible and to my family, the source of strength for me.
Funding
None
Conflicts of Interest
There are no conflicts of interest.
References
- Arif A, Afzal MF, Hamid MH. Berantinelli-Seip Syndrome: A Rare Autosomal Disorder. Annals of King Edward Medical University. 2019;25(3).
- Berardinelli-Seip Congenital Lipodystrophy (BSCL). In: Bissonnette B, Luginbuehl I, Engelhardt T. eds. Syndromes: Rapid recognition and perioperative implications, 2e. McGraw Hill; 2019.
- Garg A. Acquired and inherited lipodystrophies. N Engl J Med. 2004;350(12):1220-1234.
[Crossref] [Google Scholar] [PubMed]
- Gomes KB, Pardini VC, Fernandes AP. Clinical and molecular aspects of Berardinelli–Seip Congenital Lipodystrophy (BSCL). Clin Chim Acta. 2009;402(1-2):1-6.
[Crossref] [Google Scholar] [PubMed]
- Garg A, Agarwal AK. Lipodystrophies: Disorders of adipose tissue biology. Biochimica et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids. 2009;1791(6):507-513.
[Crossref] [Google Scholar] [PubMed]
- Maldergem VLB. Berardinelli-seip congenital lipodystrophy. 2016.
- Vijayanti GN. Berardinelli’s Syndrome-Anaesthetic considerations. JMSCR-2019.
[Crossref]
- Bennett T, Allford M. Delayed emergence from anesthesia in a child with congenital generalized lipodystrophy (Berardinelli-Seip syndrome). Paediatr Anaesth. 2012;22(3):299-300.
[Crossref] [Google Scholar] [PubMed]
- Hirano A, Takada T, Senda M, Takahashi H, Suzuki T. Anesthesia for patients with PTRF mutations: A case report. JA Clin Rep. 2018;4(1):1-4.
[Crossref] [Google Scholar] [PubMed]
- Contreras PH. Berardinelli-Seip Syndrome: Report of an old case successfully treated with anti-glucocorticoid therapy followed by bilateral adrenalectomy. In Evolving Concepts in Insulin Resistance. 2022.
- Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med. 2002;346(8):570-578.
[Crossref] [Google Scholar] [PubMed]
Citation: Rehman SU, Farooq A, Taqi A, Asad A (2024) Anesthesia Management in a Patient with Berardinelli-Seip Congenital Lipodystrophy (BSCL) scheduled for Open Reduction and Internal Fixation of Femur. J Surg Anesth. 8:235.
Copyright: © 2024 Rehman SU, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : None
