Indexed In
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 3, Issue 1
Albumin Bilirubin (ALBI) Score: A New and Simple Model to Predict Mortality in Patients of Acute on Chronic Liver Failure.
Uttayan Chakrabarti* and Manisha Bais ThakurReceived: 24-May-2019 Published: 11-Jun-2019
Abstract
The ALBI score is a new model for assessing the severity of liver dysfunction and to predict the outcome of patients with acute on chronic liver failure. The purpose of this study was to look for the prognostic value of ALBI score in predicting the outcome in patients of Acute on chronic liver failure. This prospective observational study included 50 consecutive patients of ACLF where we looked for the etiology of the underlying chronic liver disease, routine blood investigations were done, ALBI, MELD and CTP scores were calculated within 24 hours of admission. The mortality was assessed during the hospital stay and if discharged at 3 months by telephonic conversation. The association of ALBI score with the mortality in patients of ACLF was looked for and was compared with that of CTP and MELD scores. A higher ALBI score was noted in the non-surviving group than in the surviving group with a statistically significant difference (p-0.03). Comparison of the prognostic scores revealed ALBI to have a significant association with the outcome (p-0.0004), had the best predictive efficacy with the largest AUROC with a statistically significant difference noted with CTP score (p-0.044) but not with MELD score (p-0.3047). In the subgroup analysis of alcohol related ACLF, ALBI again had the best predictive efficacy though the difference with the other two scores was not statistically significant. A positive correlation was seen between ALBI and CTP, MELD scores. The fact that ALBI score uses only two convenient parameters, albumin and total bilirubin, readily obtained by an easily accessible blood test, objectively evaluated and being non inferior to the existing CTP and MELD scores indicate that ALBI score could be used as a simple, reliable prognostic score to predict the mortality in patients of Acute on chronic liver failure and for liver transplant prioritization.
Keywords
Acute on chronic liver failure; ALBI score; Mortality
Abbreviations
ACLF: Acute on Chronic Liver Failure, Autoimmune Hepatitis; ALBI: Albumin Bilirubin; APASL: Asian Pacific Association for the Study of the Liver; AUC: Area under curve; AUROC: Area under Receiver Operating Characteristics; CLD: Chronic Liver Disease; CTP: Child Turcotte Pugh; HBV: Hepatitis B Virus; HCC: Hepatocellular Carcinoma; HCV: Hepatitis C virus; INR: International Normalised Ratio; MELD: Model for End Stage Liver Disease; NASH: Non-Alcoholic Steatohepatitis; ROC: Receiver Operating Characteristic; SD: Standard Deviation; T bil: Total Bilirubin.
Introduction
Acute on chronic liver failure (ACLF) is an acute hepatic insult manifesting as jaundice (serum bilirubin ≥ 5mg/dl) and coagulopathy (INR ≥ 1.5 or prothrombin activity<40%) complicated within 4 weeks by clinical ascites and/or encephalopathy in a patient with previously diagnosed or undiagnosed chronic liver disease/cirrhosis, and is associated with a high 28-day mortality. The acute event in ACLF can be of infectious etiology comprising of hepatotropic and non-hepatotropic viruses, reactivation of hepatitis B or hepatitis C or other infectious agents afflicting the liver or it can be of non-infectious etiology like alcohol: active drinking within last 4 weeks, use of hepatotoxic drugs, herbs, flare of autoimmune hepatitis or Wilson’s disease, surgical intervention, variceal bleed A characteristic feature of ACLF is its rapid progression, the requirement for multiple organ supports, and a high incidence of mortality. Attempts to abrogate, ameliorate, or reverse the ongoing injury would allow return of hepatic synthetic functions and reversal of the liver damage [1]. In ACLF survival being the principal end-point the main objective of prognostic scores is to estimate the probability of death within a given time interval and represent a quantitative estimation of the liver reserve to stand up surgery or therapeutic interventions [2]. At present Child Pugh and MELD scores are in vogue in predicting the mortality in patients of ACLF but they have certain limitations. The ALBI score is a new model for assessing the severity of liver dysfunction and to predict the outcome of patients with acute on chronic liver failure. The score involves only 2 common laboratory parameters, albumin and total bilirubin, which is readily obtained by an easily accessible blood test and it is objectively evaluated. Therefore, high bilirubin levels combined with low albumin levels may be used to predict the severity and progression of liver injury in ACLF patients [3]. The ALBI score is simpler and easier to calculate than the MELD and Child-Pugh scores eliminates the need for subjective variables and thus avoid inter-observer variation [4].
Though there have been few studies on association of ALBI score with a subset of patients of ACLF, studies to look for its association with ACLF as a whole lacked. Therefore, we conducted this study to look for the association of Albumin-Bilirubin score with mortality in patients of Acute on Chronic Liver Failure and also compared it with CTP and MELD scores which are in vogue and widely used as prognostic scores in ACLF.
Materials and Methods
The study was a prospective observational study over a period of 18 months which included 50 consecutive patients of Acute on chronic liver failure admitted in Medicine wards of Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi. Written and informed consent was taken from all the subjects participating in the study and ethical clearance was taken from the ethical committee before conducting the study. Patients above the age of 18 years meeting the APASL criteria of ACLF were included. Known cases of malignancy, protein loss/hypo proteinemia (like malnutrition, chronic diarrhoea, nephrotic syndrome), dementia, pregnancy, chronic kidney disease was excluded. Patients were looked for the etiology of the underlying chronic liver disease; routine blood tests were done in the first 24 hours of admission. ALBI, CTP and MELD scores were calculated on admission. The Child-Pugh score was calculated from 5 variables, including bilirubin, albumin, prothrombin, ascites status, and degree of encephalopathy [5].
MELD=3.78 × logeserum bilirubin (mg/dl) + 11.20 × logeINR + 9.57 × logeserum creatinine (mg/dl)+6.43 (constant for liver disease etiology)
ALBI score=-0.085 × (albumin g/l) + 0.66×lg (TBil μ mol/l)
All patients were followed up during the hospital stay. Short term mortality was defined as patient’s death within 7days of admission while long term mortality was assessed at 3months by telephonic conversation. The patients were divided into Surviving (A) and Non-Surviving groups (B). Non-surviving group were again subdivided into subgroups B1 (7th day mortality) and B2 (90th day mortality). ALBI score was compared with CTP and MELD scores for prediction of mortality at 7th and 90th day. The mortality was also predicted by combining the ALBI and MELD scores together.
Data Collection
Serum albumin was estimated in biochemistry lab of the hospital by the Bromocresol green (BCG) method while serum total bilirubin was estimated by the Diazo method. The estimation was done in an autoanalyzer by the name of Advia 2400. All routine investigations were done by the pathology and biochemistry department of the hospital. The observations were recorded in a proforma for detailed analysis. The data of the study for further research and analysis is available from the Guru Gobind Singh Indraprastha University or from the Medicine library, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi where the study has been submitted as thesis.
Statistical Analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected, then nonparametric test was used. Quantitative variables were compared using Independent T test/Mann-Whitney Test (when the data sets were not normally distributed) between the two groups whereas qualitative variables were correlated using Chi-Square test/Fisher’s Exact test. Pearson correlation coefficient was used to assess the association of ALBI with CTP and MELD. Receiver operating characteristic curve was used to find out cut off point of parameters for predicting mortality and comparison of AUC was performed by comparing ROC curve. Univariate and multivariate cox proportional hazard regression was performed to assess the significant factors affecting mortality. The p value of <0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
Our study included 50 consecutive cases of all age groups (age ≥ 18 years) and both sexes. All the patients in our study fell in the age group of 21-70 years with a median age of 38 years with the majority being in the age group 31-40 years (40%) and the least being in the age group 61-70 years (8%). Our study had a male predominance with 42 patients (84%) being males. In our study, of the 50 patients alcohol was the most common etiology of the chronic liver disease (n=31) which was followed by Hep B virus (HBV) infection (n=8), autoimmune hepatitis (n=5), non-alcoholic steatohepatitis [NASH] (n=3), cryptogenic (n=2), hepatitis C virus [HCV] infection (n=1).
The median survival of the patients in our study was 14 days ranging from 1-90 days. Out of the 50 patients, only 6 patients had survived for 3 months (Group A) while the rest 44 patient (88%) had expired (Group B). Out of the 44 patients who had expired, 19 patients (43.18%) had short time mortality (≤7 days of hospital admission) {Group B1} while 25 patients (56.82%) had long term mortality (8-90 days of hospital admission) {Group B2}.100% mortality was seen in the age groups <30 years, 51-70 years while the major group (31-40 years) had a 10% mortality. Male and female patients had no significant difference in mortality (Male- 88.10%, female-87.50%). There was a 100% mortality observed with HBV related and NASH related CLD patients while alcohol related CLD had a mortality of 93.55%, whereas autoimmune hepatitis and cryptogenic related CLD had a mortality of 60% and 50% respectively.1 patient of HCV related CLD had survived. The etiology of chronic liver disease had a significant association with the outcome of the patients (p- 0.006) (Table 1). Among the baseline parameters in our study (Tables 1 and 2). Direct Bilirubin and ALBI score had a statistically significant association with the outcome of the patients with a higher direct bilirubin and ALBI score noted in the non-surviving group than that in the surviving group.
| Parameters | Sample size | Mean ± St. Dev | Median | Min-Max | Inter quartile Range |
|---|---|---|---|---|---|
| AGE | 50 | 40.7 ± 11.03 | 38 | 21-70 | 34-44 |
| ALB | 50 | 1.99 ± 0.41 | 2 | 1.29-3.3 | 1.700-2.200 |
| ALBI | 50 | -0.07 ± 0.44 | -0.04 | -1.05-1.2 | -0.220-0.140 |
| ALP | 50 | 224.2 ± 195.95 | 150.5 | 33-1163 | 123-215 |
| ALT | 50 | 115.06 ± 158.64 | 65.5 | 14-770 | 36-104 |
| AST | 50 | 212.56 ± 193.6 | 137.5 | 42-912 | 86 -260 |
| Cr | 50 | 2.29 ± 2.1 | 1.68 | 0.3-11 | 0.800-2.700 |
| CTP | 50 | 12.58 ± 0.99 | 13 | 10-14 | 12 -13 |
| D.BIL | 50 | 11.72 ± 6.42 | 11.5 | 2.4-30 | 7.200-15.400 |
| Hb | 50 | 8.94 ± 2.21 | 8.5 | 3.2-13.7 | 7.500-10.600 |
| INR | 50 | 2.85 ± 1.23 | 2.58 | 1.5-8.5 | 2.060-3.100 |
| K | 50 | 4.29 ± 1.13 | 4.2 | 2.8-6.8 | 3.600-4.900 |
| MELD | 50 | 33.34 ± 8.5 | 31.86 | 18.9-54 | 27.300 -37.200 |
| Na | 50 | 130.07 ± 6.39 | 130.5 | 117-142.7 | 126 -135 |
| OS in days | 50 | 27.06 ± 31.15 | 14 | 1-90 | 3-30 |
| Platelet | 50 | 113080 ± 81792.13 | 90000 | 25000-427000 | 60000-150000 |
| T.BIL | 50 | 17.75 ± 9.33 | 16.45 | 5-43.1 | 10.90-23.700 |
| T.PROTN | 50 | 5.91 ± 0.95 | 5.75 | 3.53-7.9 | 5.300-6.460 |
| TLC | 50 | 13100 ± 7862.39 | 11550 | 3200-39400 | 6600-17900 |
| U | 50 | 80.93 ± 58.03 | 63 | 15-297 | 46-114 |
ALB: Albumin; ALBI: Albumin bilirubin; ALP: Alkaline phosphatase; ALT: Alanine transaminase; AST: Aspartate transaminase; Cr: Creatinine; CTP: Child Turcotte Pugh; D.Bil: Direct Bilirubin; Hb: Hemoglobin; INR: International Normalised Ratio; K: Potassium; MELD: Model for End Stage Liver Disease; Na: Sodium; OS: Survival; T.Bil: Total Bilirubin; T.Protn: Total protein; TLC: Total leucocyte count; U: Urea; St.Dev: Standard deviation; Min-Max: Minimum-Maximum.
Table 1: Baseline parameters of the study population
| Parameters | Mortality | ||
|---|---|---|---|
| No | Yes | p value | |
| AGE | 0.419 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 41.67 ± 5.68 | 40.57 ± 11.61 | |
| Median | 42.5 | 38 | |
| Min-Max | 34-50 | 21-70 | |
| Inter quartile Range | 37 - 44 | 32.500 - 45 | |
| Hb | 0.179 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 10.05 ± 2.87 | 8.79 ± 2.11 | |
| Median | 10.4 | 8.4 | |
| Min-Max | 5.5-13.2 | 3.2-13.7 | |
| Inter quartile Range | 8.500 - 12.300 | 7.450 - 10.600 | |
| Platelet | 0.054 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 65833.33 ± 46995.39 | 119522.73 ± 83741.71 | |
| Median | 53500 | 94000 | |
| Min-Max | 29000-150000 | 25000-427000 | |
| Inter quartile Range | 30000 - 79000 | 64500 - 159500 | |
| TLC | 0.654 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 12016.67 ± 7795.75 | 13247.73 ± 7949.21 | |
| Median | 10450 | 11550 | |
| Min-Max | 4900-23200 | 3200-39400 | |
| Inter quartile Range | 5100 - 18000 | 6700 - 17800 | |
| Na | 0.083 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 125.83 ± 5.34 | 130.65 ± 6.35 | |
| Median | 126 | 132 | |
| Min-Max | 117-133 | 120-142.7 | |
| Inter quartile Range | 124 - 129 | 126 - 136 | |
| K | 0.659 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 4.48 ± 1.33 | 4.26 ± 1.11 | |
| Median | 4.2 | 4.2 | |
| Min-Max | 3-6.5 | 0.8-6.8 | |
| Inter quartile Range | 3.400 - 5.600 | 3.650 - 4.900 | |
| U | 0.199 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 57.33 ± 47.65 | 84.15 ± 59.03 | |
| Median | 37.5 | 64 | |
| Min-Max | 20-145 | 15-297 | |
| Inter quartile Range | 27 - 77 | 48 - 115 | |
| Cr | 0.332 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 1.55 ± 1.28 | 2.39 ± 2.18 | |
| Median | 1.2 | 1.95 | |
| Min-Max | 0.6-4 | 0.3-11 | |
| Inter quartile Range | 0.700 - 1.600 | 0.850 - 2.800 | |
| INR | 0.905 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 2.68 ± 0.74 | 2.87 ± 1.28 | |
| Median | 2.64 | 2.53 | |
| Min-Max | 1.66-3.91 | 1.5-8.5 | |
| Inter quartile Range | 2.320 - 2.900 | 2.025 - 3.125 | |
| T.PROTN | 0.953 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 5.93 ± 1.2 | 5.91 ± 0.93 | |
| Median | 5.6 | 5.8 | |
| Min-Max | 4.8-7.9 | 3.53-7.7 | |
| Inter quartile Range | 4.900 - 6.800 | 5.300 - 6.405 | |
| ALB | 0.478 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 2.1 ± 0.52 | 1.98 ± 0.39 | |
| Median | 2.05 | 1.98 | |
| Min-Max | 1.42-2.8 | 1.29-3.3 | |
| Inter quartile Range | 1.700 - 2.600 | 1.700 - 2.150 | |
| T.BIL | 0.056 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 10.93 ± 5.05 | 18.68 ± 9.43 | |
| Median | 10.35 | 17.75 | |
| Min-Max | 6.2-16.4 | 5-43.1 | |
| Inter quartile Range | 6.200 - 16.100 | 11 - 26.200 | |
| D.BIL | 0.034 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 6.55 ± 3.6 | 12.42 ± 6.43 | |
| Median | 6.55 | 12 | |
| Min-Max | 2.4-11.3 | 2.57-30 | |
| Inter quartile Range | 3.200 - 9.300 | 7.700 - 16.250 | |
| AST | 0.117 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 108.5 ± 42.32 | 226.75 ± 201.96 | |
| Median | 98.5 | 142.5 | |
| Min-Max | 71-164 | 42-912 | |
| Inter quartile Range | 71 - 148 | 96.500 - 291 | |
| ALT | 0.581 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 57.17 ± 23.01 | 122.96 ± 167.58 | |
| Median | 53 | 68 | |
| Min-Max | 32-86 | 14-770 | |
| Inter quartile Range | 36 - 83 | 35.500 - 124.500 | |
| ALP | 0.474 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 185 ± 138.99 | 229.54 ± 203.13 | |
| Median | 130.5 | 154.5 | |
| Min-Max | 53-431 | 33-1163 | |
| Inter quartile Range | 103 - 262 | 125 - 213 | |
| ALBI | 0.030 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | -0.38 ± 0.38 | -0.03 ± 0.44 | |
| Median | -0.17 | 0.04 | |
| Min-Max | -1.05--0.12 | -1-1.2 | |
| Inter quartile Range | -0.600 - -0.140 | -0.215 - 0.210 | |
| CTP | 0.385 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 12.17 ± 1.17 | 12.64 ± 0.97 | |
| Median | 12.5 | 13 | |
| Min-Max | 10-13 | 10-14 | |
| Inter quartile Range | 12 - 13 | 12 - 13 | |
| MELD | 0.225 | ||
| Sample size | 6 | 44 | |
| Mean ± St.dev | 29.36 ± 6.92 | 33.88 ± 8.62 | |
| Median | 29.2 | 32.6 | |
| Min-Max | 18.9-40.6 | 19-54 | |
| Inter quartile Range | 28 - 30.270 | 27.150 - 37.800 | |
Table 2: Comparison of the baseline parameters in the surviving and non-surviving groups: (No-surviving group, Yes-non surviving group)
A univariate cox regression was applied to see the association of baseline parameters with the outcome and a high total and direct bilirubin, serum sodium was found to be independent risk factors for the 3-month mortality in ACLF patients (Table 3). A multivariate cox regression when applied for the above three parameters didn’t reveal any statistically significant association with the outcome (Table 4).
| Parameters | B | SE | P value | Hazard ratio | 95.0% CI for Hazard ratio | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| AGE | .002 | .016 | .907 | 1.002 | .972 | 1.033 |
| Hb | -.021 | .061 | .734 | .979 | .868 | 1.105 |
| Platelet | .000 | .000 | .556 | 1.000 | 1.000 | 1.000 |
| TLC | .000 | .000 | .438 | 1.000 | 1.000 | 1.000 |
| Na | .067 | .029 | .022 | 1.070 | 1.010 | 1.133 |
| K | -.084 | .141 | .548 | .919 | .697 | 1.211 |
| U | .004 | .003 | .103 | 1.005 | .999 | 1.010 |
| Cr | .061 | .066 | .350 | 1.063 | .935 | 1.209 |
| INR | .045 | .134 | .735 | 1.046 | .805 | 1.361 |
| T.PROTN | -.150 | .163 | .358 | .861 | .626 | 1.184 |
| ALB | -.340 | .384 | .376 | .712 | .336 | 1.511 |
| T.BIL | .045 | .017 | .010 | 1.046 | 1.011 | 1.083 |
| D.BIL | .050 | .022 | .025 | 1.051 | 1.006 | 1.098 |
| AST | .001 | .001 | .316 | 1.001 | .999 | 1.002 |
| ALT | .002 | .001 | .088 | 1.002 | 1.000 | 1.003 |
| ALP | .000 | .001 | .903 | 1.000 | .998 | 1.002 |
| ALBI | .623 | .325 | .055 | 1.865 | .986 | 3.527 |
| CTP | .313 | .183 | .087 | 1.368 | .955 | 1.958 |
| MELD | .022 | .018 | .220 | 1.022 | .987 | 1.057 |
| Sex | ||||||
| F | 1 | |||||
| M | -.494 | .416 | .236 | .610 | .270 | 1.380 |
| Etiology | ||||||
| Alcoholism | 1 | |||||
| Autoimmune Hepatitis | -.622 | .612 | .309 | .537 | .162 | 1.781 |
| Cryptogenic | -.859 | 1.023 | .401 | .424 | .057 | 3.145 |
| HBV related | .213 | .400 | .595 | 1.237 | .565 | 2.710 |
| HCV related | - | - | - | - | - | - |
| NASH | .976 | .637 | .125 | 2.654 | .761 | 9.250 |
Table 3: Univariate cox regression analysis of the baseline parameters with the outcome of patients.
| Parameters | B | SE | P value | Hazard ratio | 95.0% CI for Hazard ratio | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Na | .053 | .030 | .076 | 1.054 | 0.994 | 1.118 |
| T.BIL | .045 | .041 | .276 | 1.046 | 0.965 | 1.134 |
| D.BIL | -.012 | .056 | .832 | 0.988 | 0.886 | 1.102 |
Table 4: Multivariate cox regression analysis of the of the independent risk factors with the outcome of patients.
The area under the ROC curve for ALBI, CTP and MELD scores (Table 5) were 0.775, 0.604, 0.665 with a sensitivity/specificity of 65.91%/100%, 18.18%/100%, 68.18%/83.33% with the cut offs being > -0.12, >13, >30.27 respectively. ALBI had a p value of 0.0004 and that of CTP and MELD scores were 0.3571 and 0.1561 thus showing a statistically significant association of ALBI score with the mortality in patients of ACLF. ALBI score was found to be better than CTP and MELD scores in predicting mortality with a statistically significant difference noted with CTP score (p-0.044) but not with MELD score (p-0.3047) (Figure 1). A combination of ALBI and MELD score was also seen which had an AUC of 0.848 which was better than all the three scores, had a sensitivity and specificity of 86.36% and 83.33% respectively with a p value of 0.0001. The difference was found to be statistically significant with CTP (p-0.0285) and MELD scores (p-0.0046) but not with ALBI score (p-0.4606). In patients of alcohol related ACLF, the AUC of ALBI, CTP and MELD scores were 0.698, 0.569, 0.534 respectively (Table 6). The sensitivity/specificity of the three scores being 65.52%/100%, 31.03%/100%, 79.31%/50% respectively, the cut offs being >-0.12 ≥ 12 and >28.4 respectively. Among the scores only ALBI was found to be statistically significant in predicting the outcome in patients of alcohol related ACLF (p- 0.0319) but the difference with the other two scores were not found to be statistically significant (Figure 2). The combination of ALBI and MELD score had an AUC of 0.716 with a specificity and sensitivity of 50% and 93.1% respectively but was not found to be statistically significant in predicting outcome (p- 0.3908). On comparison the combination of ALBI and MELD was found to be better than MELD score and the difference was statistically significant (p-0.0025). In patients of autoimmune hepatitis related ACLF, the AUC of ALBI, CTP and MELD scores were 0.833, 0.833 and 1 respectively (Table 7). The sensitivity/specificity of the three scores being 66.67%/100%, 66.67%/100%, 100%/100% respectively, the cut offs being >-0.6, >12, >28 respectively. Among the scores MELD was found to be statistically significant in predicting the outcome in patients of AIH related ACLF (p <0.0001) but the difference with the other two scores were not statistically significant (Figure 3). Similar results as MELD score were seen with the combination of ALBI and MELD with similar AUC, sensitivity and specificity and statistical significance but again the difference with other prognostic scores were not statistically significant. Subgroup analysis could not be done for rest of the subgroups due to the 100% mortality or very small study population for the analysis. ALBI score was found to be positively correlated with CTP (correlation coefficient 0.368, p value 0.0085) and MELD scores (correlation coefficient 0.504, p value 0.0002) (Figure 4).
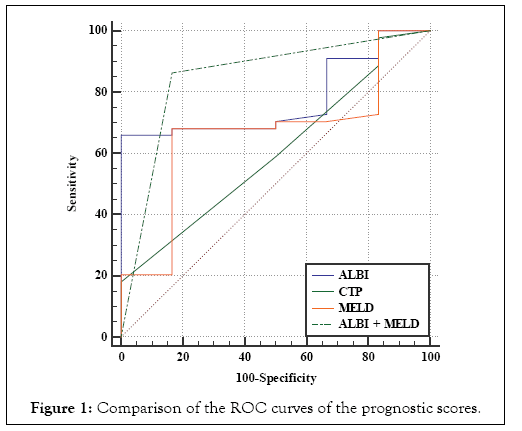
Figure 1: Comparison of the ROC curves of the prognostic scores.
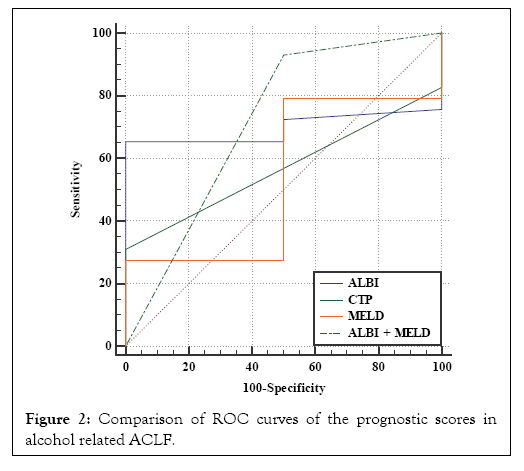
Figure 2: Comparison of ROC curves of the prognostic scores in alcohol related ACLF.
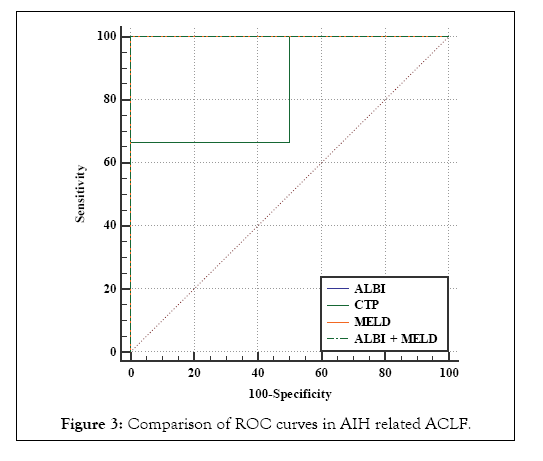
Figure 3: Comparison of ROC curves in AIH related ACLF.

Figure 4: (a, b) Positive correlation between ALBI and CTP, MELD scores.
| Area under the ROC curve (AUC) | Standard Error | 95% Confidence interval | P value | Cut off | Sensitivity | 95% CI | Specificity | 95% CI | +PV | 95% CI | -PV | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALBI | 0.775 | 0.077 | 0.634 to 0.881 | 0.0004 | >-0.12 | 65.91 | 50.1 - 79.5 | 100 | 54.1 - 100.0 | 100 | 88.1 - 100.0 | 28.6 | 11.3 - 52.2 |
| CTP | 0.604 | 0.113 | 0.456 to 0.740 | 0.3571 | >13 | 18.18 | 8.2 - 32.7 | 100 | 54.1 - 100.0 | 100 | 63.1 - 100.0 | 14.3 | 5.4 - 28.5 |
| MELD | 0.665 | 0.116 | 0.517 to 0.792 | 0.1561 | >30.27 | 68.18 | 52.4 - 81.4 | 83.33 | 35.9 - 99.6 | 96.8 | 83.3 - 99.9 | 26.3 | 9.1 - 51.2 |
| ALBI or MELD | 0.848 | 0.0873 | 0.719 to 0.934 | 0.0001 | 86.36 | 72.6 - 94.8 | 83.33 | 35.9 - 99.6 | 97.4 | 86.5 - 99.9 | 45.5 | 16.7 - 76.6 |
Table 5: Characteristics of the prognostic scores in predicting mortality of the patients.
| Area under the ROC curve (AUC) | Standard Error | 95% Confidence interval | P value | Cut off | Sensitivity | 95% CI | Specificity | 95% CI | +PV | 95% CI | -PV | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALBI | 0.698 | 0.0924 | 0.508 to 0.849 | 0.0319 | >-0.12 | 65.52 | 45.7 - 82.1 | 100 | 15.8 - 100.0 | 100 | 82.4 - 100.0 | 16.7 | 2.1 - 48.4 |
| CTP | 0.569 | 0.0643 | 0.380 to 0.745 | 0.2838 | ≤12 | 31.03 | 15.3 - 50.8 | 100 | 15.8 - 100.0 | 100 | 66.4 - 100.0 | 9.1 | 1.1 - 29.2 |
| MELD | 0.534 | 0.267 | 0.347 to 0.715 | 0.8971 | >28.4 | 79.31 | 60.3 - 92.0 | 50 | 1.3 - 98.7 | 95.8 | 78.9 - 99.9 | 14.3 | 0.4 - 57.9 |
| ALBI or MELD | 0.716 | 0.251 | 0.526 to 0.862 | 0.3908 | 93.1 | 77.2 - 99.2 | 50 | 1.3 - 98.7 | 96.4 | 81.7 - 99.9 | 33.3 | 0.8 - 90.6 |
Table 6: Comparison of prognostic scores in predicting mortality in patients of Alcohol related acute on chronic liver failure.
| Area under the ROC curve (AUC) | Standard Error | 95% Confidence interval | P value | Cut off | Sensitivity | 95% CI | Specificity | 95% CI | +PV | 95% CI | -PV | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALBI | 0.833 | 0.236 | 0.311 to 0.998 | 0.1573 | >-0.6 | 66.67 | 9.4 - 99.2 | 100 | 15.8 - 100.0 | 100 | 15.8 - 100.0 | 66.7 | 9.4 - 99.2 |
| CTP | 0.833 | 0.236 | 0.311 to 0.998 | 0.1573 | >12 | 66.67 | 9.4 - 99.2 | 100 | 15.8 - 100.0 | 100 | 15.8 - 100.0 | 66.7 | 9.4 - 99.2 |
| MELD | 1 | 0 | 0.478 to 1.000 | <0.0001 | >28 | 100 | 29.2 - 100.0 | 100 | 15.8 - 100.0 | 100 | 29.2 - 100.0 | 100 | 15.8 - 100.0 |
| ALBI or MELD | 1 | 0 | 0.478 to 1.000 | <0.0001 | 100 | 29.2 - 100.0 | 100 | 15.8 - 100.0 | 100 | 29.2 - 100.0 | 100 | 15.8 - 100.0 |
Table 7: Comparison of the prognostic scores in predicting mortality in patients of autoimmune hepatitis related acute on chronic liver failure.
Discussion
There are several scoring systems available to evaluate the severity of liver dysfunction and predict the prognosis of patients with acute on chronic liver failure with MELD and Child-Pugh scores being the commonly used ones. The Child-Pugh score contains five parameters, including the total bilirubin, serum albumin, prothrombin time, ascites and hepatic encephalopathy. However, the highly subjective evaluation of ascites and encephalopathy might reduce the accuracy of assessment. Not all variables included in CTP score have an independent influence, for instance, albumin and coagulation factors, both synthesized by the liver, are strongly correlated to each other and thus including them in a single score might result in overweighting their influence. CTP score have been found to have a ceiling effect on quantitative variables which does not exist with quantitative scores derived from regression models. For example, a patient with a bilirubin level of 55 μmol/L will be categorized in the same bilirubin class (class C) that a patient with a bilirubin level of 550 μmol/L. The MELD score incorporates 3 laboratory variables, total bilirubin, INR, creatinine, and though it eliminates the subjective factors, creatinine and bilirubin can be altered by therapeutic interventions (diuretics in particular), sepsis or hemolysis and the choice of INR is a controversial one as not all centres have used INR as a marker of coagulation in cirrhotic patients [2].
The ALBI score is a new model for assessing the severity of liver dysfunction and to predict the outcome of patients with acute on chronic liver failure which involves only 2 common laboratory parameters, albumin and total bilirubin, which is readily obtained by an easily accessible blood test and is objectively evaluated. Therefore, high bilirubin levels combined with low albumin levels may be used to predict the severity and progression of liver injury in ACLF patients [3]. The ALBI score is simpler and easier to calculate than the MELD and Child-Pugh scores eliminates the need for subjective variables such as ascites and encephalopathy and thus avoid inter-observer variation [4].
A high ALBI score measured at admission was used as a predictor for the 3-month mortality rate in patients with HBV-ACLF in a study by Chen et al. [3]. Similar to our study, ALBI was found to be positively correlated with the MELD and Child-Pugh scores. ALBI score was found to be a sensitive and specific score in predicting the 90-day mortality in patients of alcoholic ACLF in an interim analysis by Chauhan et al. where ALBI had the highest AUROC when compared with MELD, MELD-Na, CLIF C ACLF scores [6,7]. There have been studies where positive results with ALBI score as a prognostic marker have been seen in patients of liver cirrhosis, HCC, primary biliary cirrhosis [8-10]. Though there have been studies on a subset of patients of ACLF, looking for its association with ACLF as a whole lacked which we studied.
Limitations of the Study
Though our study was conducted in a tertiary care hospital it lacked the facility of liver transplantation and none of the study population had underwent liver transplantation during the follow up period which is perhaps a reason for the increased mortality in our study population. Our study included only 50 patients; therefore, further prospective studies are needed for a larger cohort of patients involving multiple centres to confirm the prognostic value of the ALBI score in Acute on chronic liver failure patients.
Conclusion
The results from our study showed that the ALBI score determined on admission indicates the likelihood of survival of an Acute on chronic liver failure patient. The fact that the ALBI score uses only two convenient parameters, being readily obtained by an easily accessible blood test, objectively evaluated and being non inferior to the existing CTP and MELD scores indicate that ALBI score could be used as a simple, reliable prognostic score to predict the mortality in patients of Acute on chronic liver failure and for liver transplant prioritization.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding
Since the study was done in a government hospital all investigations which were done and the treatment received by the patients were provided free of cost. No funding was provided by the authority for carrying out the study.
REFERENCES
- Sarin SK, Kedarisetty CK, Abbas Z, Amarapurkar D, Bihari C, Chan AC, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the study of the Liver (APASL). Hepatol Int. 2004;8:453-471.
- Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child Pugh versus MELD. J Hepatol. 2005;42:100-107.
- Chen B, Lin S. Albumin-bilirubin (ALBI) score at admission predicts possible outcomes in patients with acute-on chronic liver failure. Medicine. 2017;96:7142.
- Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin oncol. 2015;33:550-558.
- Conn HO. A peak at the child-Turcotte classification. Hepatology. 1981;1:673-676.
- Kamath PS, Weisner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;7:567-580.
- Chauhan GS, Ingle M, Chaubal A, Amonkar M, Kolhe K, Shukla A, et al. Albumin bilirubin index: a new score to predict short term mortality in alcoholic ACLF. J Clin Exp Hepatol. 2018;8:11.
- Shao L, Han B, An S, Ma J, Guo X, Romeiro FG, et al. Albumin-to-bilirubin score for assessing the in-hospital death in cirrhosis. Transl Gastroenterol Hepatol. 2017;2:88.
- Ogasawara S, Chiba T, Ooka Y, Suzuki E, Kanogawa N, Saito T, et al. Liver function assessment according to the Albumin-Bilirubin (ALBI) grade in sorafenib-treated patients with advanced hepatocellular carcinoma. Invest New Drugs. 2015;33: 1257-1262.
- Chan AW, Chan RC, Wong GL, Wong VW, Choi PC, Chan HL, et al. New simple prognostic score for primary biliary cirrhosis: Albumin-bilirubin score. J Gastroenterol Hepatol. 2015;30:1391-1396.
Citation: Chakrabarti U, Thakur MB. Albumin Bilirubin (ALBI) Score: A New and Simple Model to Predict Mortality in Patients of Acute on Chronic Liver Failure. J Clin Med Sci 2019; 3:114. doi: 10.35248/2593-9947.19.3.114
Copyright: © 2019 Chakrabarti U, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
