Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 9, Issue 3
Aging and the Science
Ali H. Rajput*Received: 29-Mar-2021 Published: 21-Apr-2021, DOI: 10.35248/2329-8847.21.9.253
Abstract
Human body evolves continuously from infancy to old age. Life expectancy has been increasing for several decades. Consequently, we now have the largest proportion of the elderly in the population, than at any time before. As in all age categories, some diseases are more common in the elderly. Additionally, normal age related changes may resemble some well-known treatable diseases. Most of the current medical knowledge is based on studies of young/middle aged individuals, some of which is not applicable to the elderly. The response to certain drugs is different in the elderly than in the younger persons. Distinguishing between “normal” aging and disease is therefore important. This article provides an example of Parkinson’s disease in the elderly. As the number of the elderly in the population is increasing there is greater need to provide proper health service for the population. The Father of modern treatment of Parkinson’s disease, Professor Hornykiewicz was making major discoveries at age 90. Age based retirement is being phased out at many institutions. That would help use the valuable skills which the older individuals have acquired in life. Research in the elderly is needed to provide the best services for this growing segment of population.
Keywords
Elderly; Aging population; Incidence; Healthcare; Parkinson’s disease; Parkinsonism
Introduction
All biological organisms evolve with age. Such changes in the human beings may be evident to the naked eye. They occur from head to toe and skin to bone deep. All body organs have some changes with age. The wrinkled skin is well known in the elderly as is the fragile bones in this age group. The anatomy and physiology of a 13 year old is different from that of a three year old. Similarly, a 74 year old is different from a 34 year old individual. Much of scientific information on human beings is based on the studies of young/middle age adults. Some of that knowledge is not applicable to the elderly.
Literature Review
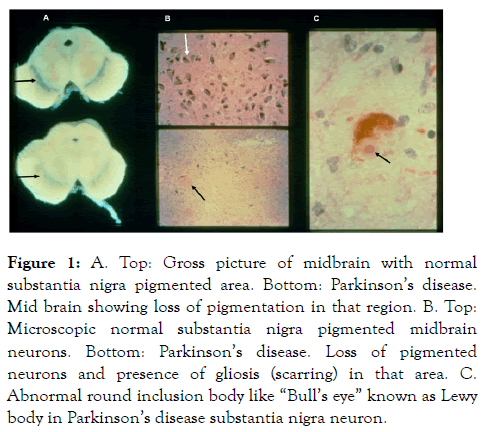
The knowledge of neonatology has advanced significantly in recent years, but the science of geriatrics is just being recognized as a distinct field of medicine. As the proportion of elderly in the population increases, there is growing need for sound scientific information to deal with the normal aging and the specific issues related to the disorders that are concentrated in the old age. It is not possible to discuss the issue of aging in any one organ let alone all body organs in one paper. Therefore, I will focus on one disease Parkinson’s Disease (PD) which is concentrated in the old age, as an example. In the population between age 80 and 99, the incidence (new cases) of PD is six times higher than in the population between age 50 to 54 [1]. One study which covered a 30-year time period, found that the incidence of PD increased by 20% in the general population, but the incidence in the elderly increased by 80% [2]. Another study reported 0.3 per 1000 incidence of PD in age 55 to 60 but 5.3 per 1000 (18 x higher) in those between age 75 to 80 years [3]. It has been projected that between 2010 and 2030 the number of PD patients will increase by 65% [4]. Higher number of new cases and the increased life expectancy in PD, since the widespread use of levodopa [5], has led to higher prevalence (number of cases at any given time) in the population. Thus, there is growing need for better scientific studies of normal aging and the diseases that are concentrated in the old age. In 1817, James Parkinson, a family physician from London, England, described six cases of “Shaking Palsy”. These patients had shaking and slowed movements. This disorder was later named in his honor as “Parkinson’s disease”. Subsequent studies, revealed characteristic brain pathology in PD. Figure 1 shows typical brain pathology changes in PD.
Figure 1: A. Top: Gross picture of midbrain with normal substantia nigra pigmented area. Bottom: Parkinson’s disease. Mid brain showing loss of pigmentation in that region. B. Top: Microscopic normal substantia nigra pigmented midbrain neurons. Bottom: Parkinson’s disease. Loss of pigmented neurons and presence of gliosis (scarring) in that area. C. Abnormal round inclusion body like “Bull’s eye” known as Lewy body in Parkinson’s disease substantia nigra neuron.
There is loss of pigmented (dopaminergic) neurons in the substantia Nigra (SN). That is visible to naked eye in crosssection of midbrain (Figure 1A). Microscopically, there is loss of normal pigmented neurons in the SN neurons and scarring (gliosis) (Figure 1B). There are abnormal round inclusions in the SN neurons known as Lewy Body (LB) (Figure 1C). The advances in PD histopathology reached the peak by 1919 when it was established that damage to SN cells was the typical feature of PD and LB inclusions described in 1913 was characteristic. After 1919, there were no major new histological developments in PD but other pathological conditions which had some similar clinical features were identified in small number of patients. Collectively PD and other conditions with similar clinical features are known as Parkinson syndrome or Parkinsonism.The next major development in PD occurred in 1960. Professor O. Hornykiewicz and his team studied fresh frozen autopsied brains from normal elderly, infants, PD and other neurological diseases [6]. They detected marked loss of Dopamine (DA) in the striatum (putamen and caudate) in the PD brains, but not in other neurological diseases or the normal elderly brains. There is some decline of striatal DA of the elderly as well. Professor Hornykiewicz along with his team studied that issue and reported that different brain regions had specific pattern of DA loss in PD which is different from pattern of loss in normal aging. As well, the severity of DA loss in the PD is more pronounced than seen in old age. It was thus established that PD represented a distinct pathological entity rather than a manifestation of normal aging, as was once thought to be the case. One year later, that observation resulted in discovery of Levodopa (LD) as the drug of choice for PD treatment. Clinically, PD is characterized by the presence of at least two of the three major motor features bradykinesia (motor slowing down), rigidity (increased muscle tone) and tremor (mostly at rest). Later in the course of PD, the patients develop postural instability resulting in falls and related complications. There is currently no reliable laboratory test for the diagnosis of PD. The diagnosis is based on clinical observations alone. However definite diagnosis of PD is only possible on pathology study of brain showing the typical changes noted above [7]. Because there is some similarity in clinical features of PD and normal elderly, notably the motor function slowing, joint stiffness, gait and balance problems, and there is no laboratory test to distinguish between them, we rely on clinical features to make that distinction. Table 1 shows major clinical features that distinguish PD from normal aging [8,9].
| Normal elderly | Parkinson’s disease | |
|---|---|---|
| Motor slowing/Neurological findings | ||
| Symmetry of findings | Symmetrical | Often asymmetrical |
| Focal examination | Normal | Normal |
| Tone | Normal | Increased rigidity |
| Sensory function | Normal (except vibration reduction in feet may be decreased | As in normal aging |
| Reflexes | Normal symmetrical (ankle jerks may be hypoactive) Plantars flexor | As in normal aging |
| Muscle strength | Normal | Normal |
| Rest tremor | Absent | Usually present |
| Facial expression | Normal | Reduced |
| Handwriting | Normal | Micrographia |
| Speech | Normal | Low volume |
| Tone | ||
| Characteristic | Equal and normal resistance in all directions of movement | Resistance increased and sustained and equal in opposite directions. Passive movement Reproducible |
| Symmetry | Symmetrical | Usually asymmetrical |
| Reinforcement – related tone change | No significant change and is symmetrical | Usually asymmetrical increases |
| Gait | ||
| Base (distance between feet while standing/walking) | Slightly wider than at younger age | Narrow base |
| Functions in the involved lower limb | Normal and symmetrical | Impaired regardless of weight-bearing or not (no dissociation) |
| Upper-limb motor function | Normal | Impaired on the involved side |
| Armswing | Normal | Reduced on involved side |
| Posture | Erect or neck and trunk flexion | Generalized flexion – neck, trunk, hip, knee, elbow |
| Postural reflexes (pull test) | May be normal or impaired | Impaired in moderately advanced disease |
| Foot tapping in sitting or lying position | Normal | Affected side slow and progressively slower and decline in amplitude |
| Gait abnormality | Uncommon – increases with age | Late manifestation usually |
| Visual and auditory cue effect | No change in gait | Improves gait |
| Dementia | Rare | Present in about one-third of cases |
| Levodopa response | No benefit | Improvement |
Table 1: Clinical features.
Discussion
I will note some additional considerations for that purpose. When evaluating postural reflexes (balance), pull the patient towards you to make sure that the patient does not fall – do not push the patient away as that may result in a fall. It should be noted that resting tremor in a fully supported part of the body, such as lying on the examining table is not a feature of normal aging, it always represents some disorder the most common being the PD. Tone is tested with the examiner moving the body part passively when the patient is fully relaxed, notably the part being tested.
There may be focal pathology such as arthritis, which restricts passive movement or the movement produces pain, making it appear that the tone is increased. That problem can be identified by examining the local joint area, for mechanically restricted movement and for pain with passive movement. Another consideration for rigidity is the involuntary resistance by the patient, who is unable to comprehend and cooperate for assessing the tone. This is called paratonia, also known as gegenhalten. In paratonia, the resistance to the passive movements is irregular, intermittent, may change from increased tone to decreased tone or may manifest as progressively greater resistance if the passive movement is continued. The main feature is the unpredictability and variability. Typically, the paratonia is evident symmetrically on two sides of body. The increased tone in PD is often known as “cogwheel rigidity”, due to the ratchety quality of the resistance during passive movement. Another phenomena, to keep in mind, is known as the Froment’s phenomena. It is characterized by interruption of passive movements by tremor. It is usually evident on reinforcement – asking the patient to exert with the contralateral limb. If you are testing the arm, have the patient exert with the contralateral foot and vice versa. If during the passive movement, such as at the wrists, there is intermittent interruption, giving cogwheeling character, stopping the passive movement when the ratchety resistance is observed is valuable to determine the cause of intermittent resistance. In the case of Froment’s sign, the abnormal movement (tremor) will continue when you stop moving the part e.g. wrist. On the other hand, in the cogwheel rigidity of PD, the cogwheeling will stop when you stop the passive movement. In some cases with subtle PD manifestation even the detailed clinical assessment may not differentiate between PD and normal aging. In that situation, a trial on LD is warranted. Levodopa plus dopa decarboxylase inhibitor, carbidopa (Sinemet) 300 to 600 mg/day in three divided doses for two consecutive months trial is needed to determine the effect of the drug [10]. There would be no improvement in age related motor deficit. The PD patient may report subjective and/or objective improvement. Where that is not possible to ascertain, ask the patient if there is something that he/she can do now after the treatment which was not possible previously. Some individuals may have subjective benefit without the objective evidence. Another method to determine the subtle drug efficacy is to discontinue (withdraw gradually) LD for at least two weeks – in some cases the drug has a long duration effect. If upon discontinuing LD, there is worsening of the symptoms that would indicate the patient has PD. Another indicator of LD efficacy and diagnosis of PD is the emergence of abnormal movements, which is combination of chorea/dystonia, known as dyskinesia [11].
Normal elderly do not develop dyskinesia on LD [12]. Professor Hornykiewicz and his colleagues demonstrated that LD effectively relieved PD symptoms [13]. Because they had access to only two grams of LD, they used the drug intravenously [13] to prove the efficacy of the drug, in many cases. They also reported that the LD benefit was dose-dependent [13]. Long-term intravenous use of LD is not feasible for treating PD, as the drug needs to be taken several times daily. Cotzias and co-workers 14 followed the observations by Hornykiewicz’s group [13]. They used large oral dose up to 16 grams/day of D-L-DOPA in 1967, and observed dramatic improvement of PD [14]. Subsequent investigators modified the LD dose, showing that a much lower dose (equivalent of 3 grams LD/day) has slower initial benefit but in the longer term is more beneficial to the patients [15]. At one time, there was some concern that LD is toxic to human substantia nigra. The SN neuronal loss is characteristic of PD. If toxic, LD would accelerate the disease process. Subsequent studies including autopsy findings of the brain, found that LD is not toxic to human SN12 [16]. Therefore, LD should be used when needed in the elderly without concern of toxicity. There is another class of drugs known as dopamine agonists. In general, these drugs are not recommended for the elderly as they produce more side effects. Similarly, the 8 older anticholinergic drugs are not recommended for the elderly PD cases. Another drug called amantadine may be helpful in some elderly but must be used with caution as it has some anticholinergic effect. Druginduced parkinsonism is more common in the elderly [17]. It is consequent to dopamine receptor blockage. There are however no anatomical changes in the brain in drug-induced parkinsonism [17].
These cases are best treated with amantadine. There are some other pathological disorders which produce Parkinson-like motor picture [18]. It has been suggested that the elderly parkinsonian patients have different variety of Parkinson pathology than the younger individuals. An autopsy study [19], found that the elderly have the same type of pathology which produces parkinsonism in the younger people. Therefore, the elderly parkinsonian cases should be treated as the younger persons with the precautions noted above.
There was once an active debate that PD may be contagious and could be transmitted from person-to-person. The closest personal contact in society is between married couples. An autopsy study [20] where both spouses had parkinsonism revealed that neither PD nor other Parkinson variants are transmitted from one spouse to the other. The wife and husband develop the disease by coincidence [20]. Science and the older scientists “The pace of medical research has accelerated, resulting in large number of publications”. There is pressure on the younger scientists to publish for their employment and promotion. Therefore, some of these authors publish in undue hurry. They review the literature of the last 5 to 10 years. Understandably, every development has not occurred in the last 5 or 10 years. A new scientist may observe something and conclude that to be a novel finding, not knowing that the same has been known for a long time. The senior scientists, particularly the clinicians, have an advantage. They have seen such cases before and can very quickly distinguish between something new from what has been known previously. Time and the use of financial resources are major considerations in research. Therefore, input from senior scientists during early stage of planned research is valuable to devise more focused and economical research.
The invitation to me for this paper was triggered by the articles that I wrote about Professor Oleh Hornykiewicz [21,22]. Professor Hornykiewicz was a pioneer and he had many “firsts” in the field of PD. He should have received a Nobel Prize for that. He pioneered a new method to dissect fresh frozen autopsied human brain to precisely identify brain areas needed for focused studies. He and his colleagues analyzed such areas of special interest in PD. They discovered a marked striatal DA loss to be specific for PD6. He combined his outstanding skills of neuroanatomy, biochemistry and neuropharmacology to further advance this discipline. After the initial findings of DA loss in PD6, he concluded that DA deficiency was the biochemical basis of parkinsonian clinical manifestations. He had already determined in animal studies that DA given intravenously, by mouth or any other route does not cross the blood brain barrier and hence would not benefit PD cases. Therefore, he used LD, which is the precursor of DA and can cross the blood-brain barrier, and proved that LD was the most effective drug for PD. As noted above, the intravenous LD use was necessary as they had a very small amount of the drug available and wanted to prove the efficacy of the drug in as many patients as possible. His discovery was followed by Cotzias, et al. [14] using large D-LDOPA dose in 1967. Professor Hornykiewicz remained active in research and wrote major scientific papers while in his 90’s [22]. Thus, the old age by itself did not stop him from doing major scientific work. The impact of Professor Hornykiewicz’s work and the discovery in 1961 that PD, a progressive neurological disease can be satisfactorily controlled with LD has lived on. Even today, LD remains the gold standard for PD treatment. There are currently more than 7 million PD patients in the world.
Most of these cases are treated with LD. If only 5 million of those were treated with the drug which produces major symptomatic benefit, 250 million person years of human life has been markedly improved over the past 50 years. All other PD drugs are compared with LD efficacy. Professor Hornykiewicz’s work also attracted other scientists to copy the methodology he pioneered to study other chronic neurological diseases such as Alzheimer’s disease. His influence on PD and other chronic neurological diseases is immeasurable. He has therefore been called Father of Modern Treatment of Parkinson’s disease [22].
Conclusion
In conclusion, the science of old age continues to advance but the pace needs to accelerate to meet the needs of growing elderly population. I have provided an example of one disease in the old age.
REFERENCES
- Elbaz A, Bower JH, Maraganore D, McDonnell S, Peterson B, Ahlskog E, et al. Risk tables for parkinsonism and Parkinson's disease. J Clin Epidemiol. 2002;55(1): 25-31.
- Savica R, Grossardt BR, Bower JH, Ahlskog JE, Rocca WA. Time trends in the incidence of Parkinson disease. JAMA Neurol. 2016;73(8): 981-989.
- de Lau LML, Giesbergen PCLM, de Rijk MC, Hofman A, Koudstaal PJ, Breteler MMB. Incidence of parkinsonism and Parkinson disease in a general population: The Rotterdam Study. Neurology. 2004;63(7): 1240-1244.
- Wanneveich M, Moisan F, Jacqmin-Gadda H, Elbaz A, Joly P. Projections of prevalence, lifetime risk, and life expectancy of Parkinson's disease (2010-2030) in France. Mov Disord. 2018;33(9): 1449-1455.
- Rajput AH, Uitti RJ, Rajput A, Offord KP. Timely levodopa (LD) administration prolongs survival in Parkinson's disease. Parkinsonism Relat Disord. 1997;3(3): 159-165.
- Ehringer H, Hornykiewicz O. Distribution of noradrenaline and dopamine (3-hydroxytyramine) in human brain: their behaviour in extrapyramidal system diseases. Klin Wochenschr. 1998;4(2): 53-57.
- Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999;56(1): 33-39.
- Rajput AH. Movement Disorders and Aging. In: Watts RL, Koller WC (Eds) Movement Disorders: Neurologic Principles and Practice. McGraw-Hill pUblisher, New York, USA. 1996; Pp:673-686.
- Rajput A, Rajput AH. Old age and Parkinson's disease. In: Koller WC, Melamed E (Eds), Handbook of Clinical Neurology. 2003; Pp: 427-444.
- Rajput AH, Rozdilsky B, Rajput A, Ang L. Levodopa efficacy and pathological basis of Parkinson syndrome. Clin Neuropharmacol. 1990;13(6): 553-558.
- Rajput AH, Fenton ME, Birdi S, Macaulay R, George D. Clinicalpathological study of levodopa complications. Mov Disord. 2002;17(2): 289-296.
- Rajput AH, Rajput ML, Robinson CA, Rajput A. Normal substantia nigra patients treated with levodopa - Clinical, therapeutic and pathological observations. Parkinsonism Relat Disord. 2015;21(10): 1232-1237.
- Birkmayer W, Hornykiewicz O. The effect of L-3,4-dihydroxyphenylalanine (=L-DOPA) on akinesia in Parkinsonism. Wien Klin Wochenschr. 1961;73: 787-788.
- Cotzias GC, Van Woert MH, Schiffer LM. Aromatic amino acids and modification of Parkinsonism. N Engl J Med. 1967;276(7): 374-379.
- Rajput AH, Stern W, Laverty WH. Chronic low dose therapy in Parkinson's disease: An argument for delaying levodopa therapy. Neurology. 1984;34(8): 991-996.
- Rajput AH, Fenton ME, Birdi S, Macaulay R. Is levodopa toxic to human substantia nigra? Mov Disord. 1997;12(5): 634-638.
- Shuaib UA, Rajput AH, Robinson CA, Rajput A. Neuroleptic induced parkinsonism: Clinicopathological study. Mov Disord. 2016;31(3): 360-365.
- Jellinger K. The Pathology of Parkinsonism. 1987.
- Rajput AH, Rajput EF. Octogenarian parkinsonism – Clinicopthological observations. Parkinsonism Relat Disord. 2017;37: 50-57.
- Rajput AH, Ferguson LW, Robinson CA, Guella I, Farrer MJ, Rajput A. Conjugal parkinsonism - Clinical, pathology and genetic study. No evidence of person-to-person transmission. Parkinsonism Relat Disord. 2016;31: 87-90.
- Rajput AH. In memoriam - Professor Oleh Hornykiewicz, MD (1926-2020): An outstanding scientist and human being. Parkinsonism Relat Disord. 2020;78: 195-197.
- Rajput AH, Kish SJ. Professor Oleh Hornykiewicz, MD (1926-2020): Remembering the Father of the Modern Treatment of Parkinson's Disease and the Man. Mov Disord. 2020;l35: 1916-1921.
Citation: Rajput AH (2021) Aging and the Science. J Aging Sci. 9:253.
Copyright: © 2021 Rajput AH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.