Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 5, Issue 6
Addition of Clonidine in Peribulbar Anesthesia for Vitreoretinal Surgeries: Randomized, Double-Blind Clinical Trial
Livia Maria Campos Teixeira1, Catia Sousa Goveia1, Marco Aurelio Soares Amorim2, Denismar Borges de Miranda3*, Larissa Goveia Moreira4, Luis Claudio Araujo Ladeira1 and Edno Magalhaes12Department of Anesthesiology, Center for Studies and Training at Dr. Jose Quinan, Goiania, Goias, Brazil
3Department of Ophthalmology, Goias Federal University, Goias, Brazil
4Department of Anesthesiology, Hospital of Base, Brasília, Distrito Federal, Brazil
Received: 05-Nov-2021 Published: 26-Nov-2021
Abstract
Objective: The study evaluated the influence of clonidine on Intraocular Pressure (IOP), quality of the block and postoperative analgesia, as an adjunct to peribulbar block for vitreoretinal surgery.
Methods: Randomized, double-blind clinical trial, approved by the Research Ethics Committee, with 62 adults undergoing vitreoretinal surgery, under peribulbar block. They were randomly assigned to 2 groups: Control (0.875% ropivacaine) and Clonidine (0.875% ropivacaine+1 μg/kg clonidine). Ocular Anesthetic Scoring System, Ramsay sedation score, IOP and hemodynamic parameters were checked before, 5, 10 and 20 minutes after peribulbar block. Degree of akinesia (Nicoll Score) was tested 10 minutes after the block. Postoperative analgesia was assessed 30 minutes after surgery and 24 hours after block. Statistical analysis by Student’s t test or Mann-Whitney U test, according to the type of variable.
Results: Groups were similar regarding demographic variables, length of surgery, hemodynamic parameters, akinesia, sedation and analgesia 30 minutes after surgery. A lower IOP was observed in the Clonidine group compared to the Control at 5, 10 and 20 minutes. The reduction in IOP may be due to the vasoconstrictor effect of clonidine in the ciliary vessels, decreasing the production of aqueous humor. There was no arterial hypotension, which could contribute to this finding. With the addition of clonidine to the block, there was a lower frequency of pain complaints and less pain intensity, corroborating previous studies that found improvement in postoperative analgesia. There were no adverse effects.
Conclusion: Clonidine 1 μg/kg associated with 0.875% ropivacaine in peribulbar block for vitreoretinal surgeries reduces IOP, the frequency of pain complaints and pain intensity, without causing side effects.
Keywords
Regional anesthesia; Local anesthetics; Clonidine; Vitreoretinal surgery
Abbreviations
ASA: American Society of Anesthesiologists; DBP: Diastolic Blood Pressure; ECG: Electrocardiography; HR: Heart Rate; IOP: Intraocular Pressure; NIBP: Non-Invasive Blood Pressure; SBP: Systolic Blood Pressure; SpO2: Peripheral Arterial Oxygen Saturation; VAS: Visual Analogue Pain Scale.
Introduction
Peribulbar anesthesia was developed in 1986 by Davis and Mandel and has been replacing retrobulbar and general anesthesia for ophthalmologic surgeries because it has a lower incidence of adverse events [1]. The use of regional anesthesia for vitreoretinal surgeries has become an established and safe technique, and if compared to general anesthesia, it is associated with a lower incidence of respiratory and hemodynamic complications, greater postoperative analgesia and a lower incidence of nausea and vomiting [2].
Clonidine, a centrally acting α2 adrenergic receptor agonist, was synthesized in 1960. Because of its analgesic and sedative effect, it began to be used in the 1990s as a pre-anesthetic medication, in general anesthesia and spinal blocks. Its selectivity for α2/ α1 receptors is 220/1. It has the ability to decrease sympathetic activity and reduce the release of norepinephrine, decreasing perioperative myocardial ischemia and postoperative mortality in cardiac patients undergoing non-cardiac surgery. Studies have shown that when added to the local anesthetic in peripheral blocks, it improves and prolongs the duration of anesthesia [3-6].
Some studies suggest that the use of clonidine in ophthalmic blocks may reduce the intraocular pressure (IOP), the latency, increase the time of analgesia, and greater hemodynamic stability during the procedure, particularly in relation to blood pressure [7-12].
The mechanisms involved in the reduction of IOP are the vasoconstriction of efferent arterioles in the ciliary process and the increase in water drainage, secondary to the decrease in sympathetic vascular tone.
There are few studies evaluating the effect of clonidine associated with ropivacaine in peribulbar block for vitreoretinal surgery. Therefore, the present study aimed to evaluate the influence of the addition of clonidine to ropivacaine in peribulbar block on intraocular pressure, quality of the block, postoperative analgesia and the occurrence of side effects.
Methodology
This is a controlled, randomized, prospective, double-blind clinical trial, performed at the University Hospital of Brasília, with patients undergoing elective vitreoretinal surgeries, on an outpatient basis. The study only started after its approval by the Research Ethics Committee of the Faculty of Health Sciences of the University of Brasília under approval protocol No. 27099614.1.0000.0030; all participants signed the Free and Informed Consent Form and it is in line with the Declaration of Helsinki.
It was estimated that, for the study to have 80% power to test the hypothesis at a 5% significance level and considering a 50% prolongation of analgesia time in the clonidine group, at least 16 patients in each group would be needed. It helped in the calculation of the sample size previous works that used similar techniques. The patients were divided into two groups, named Clonidine and Control. Randomization was performed using a barcode generated by a telephone application, in swapped blocks of two patients. The confidential allocation was maintained by means of a sealed brown envelope.
Participants who met the following criteria were considered eligible: age between 18 and 79 years, physical status I or II according to criteria of the American Society of Anesthesiologists (ASA), and candidates for elective vitreoretinal surgery under peribulbar block who agreed to participate in the study. Patients with known allergies to local anesthetics or clonidine, orbital abnormalities, abnormal eye movement, diseases with increased IOP, chronic cough, chronic use of clonidine, anticoagulant therapy and inability to understand the study information were excluded.
After admission to the outpatient surgical center, pre-anesthetic evaluation was performed. At this stage, the participants eligible for the study and who agreed to participate were provided information such as sex, education, age, weight, height, clinical comorbidities (diabetes mellitus and systemic arterial hypertension) and physical status according to ASA.
After peripheral venipuncture with a 22 G catheter, a nasal catheter was installed to administer oxygen with a flow rate of 2 L/min and pre-anesthetic medication (midazolam 1 to 2 mg and fentanyl 20 to 30 μg). Continuously monitored electrocardiography (ECG), Heart Rate (HR), Non-Invasive Blood Pressure (NIBP) and Peripheral Arterial Oxygen Saturation (SpO2) were performed on all patients.
Sedation to perform peribulbar anesthesia was provided with propofol (0.4 mg/kg). Peribulbar block was performed, with a 20 G needle, through double puncture (inferolateral and medial), by an anesthetist who was unaware of the solution’s content. The total volume administered was 8 mL, 5 mL in the inferolateral puncture and 3 mL in the medial puncture. The solutions were prepared by a researcher not involved in the execution of the block and in the evaluation of the groups. The clonidine group received peribulbar block with 7 mL of 1% ropivacaine associated with 1 mL of a solution containing 1 μg/kg of clonidine (0.875% ropivacaine solution). The control group with a 7 mL solution of 1% ropivacaine combined with 1 mL of distilled water (0.875% ropivacaine solution). Immediately after peribulbar block, all patients received 40 mg of tenoxicam intravenously, as a complement to postoperative analgesia [13].
In this study, postoperative analgesia was assessed as the primary outcome, assessed by the visual analogue pain scale (VAS), with scores ranging from 0 to 10 (0=no pain, 1-2=mild pain, 3-7=moderate pain, 8-10=severe pain, 10=unbearable pain). The analgesia enquire was carried out 30 minutes after the end of the surgery and 24 hours after the block via telephone contact. The need for supplementary analgesia in the postoperative period was questioned during telephone contact.
Secondary outcomes were considered as sedation level using the Ramsay Sedation Scale, which ranges from level 1 (anxious or agitated patient) to level 6 (without response to stimulus); ocular motor and sensory function, using the Ocular Anesthetic Scoring System-OASS scale, which takes into account motor and sensory activity, with a score from 0 (poor) to 14 (good); Intraocular Pressure (IOP) assessed using a digital applanation tonometer (Tono Pen®); degree of akinesia was performed using the Nicoll score, in which the eyeball is schematically divided into quadrants and the motor block in each quadrant evaluated with a gradation of 0 to 2 points (0=complete movement, 1=partial movement and 2=absence of movement), the intensity of the motor block of the extrinsic musculature of the eyeball is given by the sum of the quadrants, varying from 0 to 8: the block with a score greater than 6 is appropriate. In cases of inadequate motor block after 10 minutes, the surgeon supplemented the block, and the patients were excluded from the study. In addition, the occurrence of adverse effects, such as bradycardia (decrease in heart rate greater than 20% of the values before the block), arterial hypotension (defined as a decrease in mean arterial pressure above 20% of the values before the block) and hypoxia (SpO2<90% in room air) during operation. All data were recorded in four moments: before (T0), 5 (T5), 10 (T10) and 20 (T20) minutes, respectively after peribulbar block. The surgeries were performed by medical retina specialists and the blocks were performed by anesthesiologists with expertise in the technique [14-16].
Statistical analysis was performed using a commercially available statistical software package (SPSS for MAC, V.22.0, IBM-SPSS, Chicago, Illinois, USA). To evaluate the sample distribution, a Kolmogorov-Smirnov test was used. For the analysis of quantitative variables that showed normal distribution, Student’s t test was used to compare groups, otherwise the Mann-Whitney U test was used. To compare the proportions of qualitative categorical variables, the chi-square test (χ2). Statistical significance was considered with p<0.05.
Results
Sixty-four patients were considered eligible and all agreed to participate. Two patients were excluded (one using anticoagulant and one who had abnormal eye movement). Sixty-two patients were evaluated and underwent peribulbar block for vitreoretinal surgery (Figure 1). Baseline demographic and clinical characteristics of patients are shown in Table 1.
| Features | Groups | p-value | |
|---|---|---|---|
| Control (n=31) | Clonidine (n=31) | ||
| Demographic | |||
| Sex | 0.57* | ||
| Male | 21 (34%) | 18 (29%) | |
| Female | 10 (16%) | 13 (21%) | |
| Age (years) | 54.6 ±15.1 | 53.9 ± 14.6 | 0.86 † |
| Weight (Kg) | 68.9 ± 10.5 | 68.1 ± 10.4 | 0.73 † |
| Height (cm) | 166.2 ± 6.5 | 166.1 ± 7.8 | 0.93 † |
| Clinical | |||
| Physical State (ASA) | 0.79* | ||
| I | 13 (21%) | 12 (20%) | |
| II | 18 (29%) | 19 (30%) | |
| IOP (mmHg) | 21.26 ± 9.7 | 17.35 ± 6.5 | 0.07 † |
| SBP (mmHg) | 140.65 ± 22.7 | 136.13 ± 20.7 | 0.41 † |
| DBP (mmHg) | 83.9 ± 13.4 | 81.5 ± 11.9 | 0.47 † |
| HR (bpm) | 73.6 ± 10.7 | 74.9 ± 14.6 | 0.68 † |
| SpO2 (%) | 98.9 ± 1.5 | 98.1 ± 1.9 | 0.06 † |
| Ramsay | 2 | 2 | 0.15 ‡ |
| OASS | 0 | 0 | 1.00 ‡ |
| Surgical time (min) | 133.4 ± 53.2 | 118.8 ± 59.3 | 0.31 † |
Note: Data are presented in absolute and relative frequency (%); mean ± standard deviation and median, when applicable. *Statistical analysis performed using the χ2 test; † Statistical analysis performed with the Student t test; ‡ Statistical analysis performed with the Mann-Whitney U test; ASA, physical state according to criteria of the American Society of Anesthesiologist
Abbreviations: IOP-Intraocular Pressure; SBP-Systolic Blood Pressure; DBP-Diastolic Blood Pressure; HR-Heart Rate; SpO2-Oxygen Saturation in the blood; OASS-Ocular Anesthetic Scoring System.
Table 1: Baseline characteristics of patients undergoing peribulbar block in vitreoretinal surgeries comparing the addition of clonidine with control.
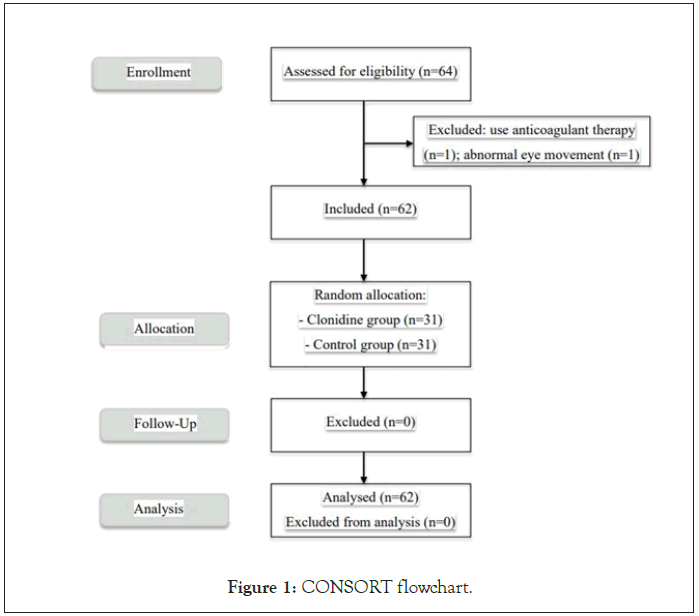
Figure 1: CONSORT flowchart.
There was no significant difference between the groups regarding sedation and the quality of the block. In all patients, the maximum degree of motor block (Nicoll=8) was reached within the first 10 minutes, regardless of the addition of clonidine to the local anesthetic. Lower IOP values were found in the Clonidine group compared to the Control group at times 5, 10, 20 minutes (p<0.05), demonstrating that the addition of clonidine to the local anesthetic promoted a significant reduction in IOP (Table 2). Still in the same table, HR, systolic (SBP) and diastolic (DBP) blood pressure, SpO2, there was no statistical difference between the groups. No patient had hemodynamic changes.
| Clinical characteristics | Groups | p-value | |
|---|---|---|---|
| Control (n=31) | Clonidini (n=31) | ||
| IOP (mmHg) | |||
| T5 | 29.4 ± 12.9 | 23.8 ± 7.3 | 0.04 † |
| T10 | 25.8 ± 11.8 | 20.2 ± 6.6 | 0.02 † |
| T20 | 25.8 ± 11.8 | 17.7 ± 5.0 | 0.01 † |
| SBP (mmHg) | |||
| T5 | 125.9 ± 23.2 | 121.94 ± 15.2 | 0.41 † |
| T10 | 125.1 ± 22.7 | 118.7 ± 14.3 | 0.19 † |
| T20 | 124.2 ± 20.5 | 118.0 ± 13.2 | 0.16 † |
| DBP (mmHg) | |||
| T5 | 77.3 ± 12.9 | 74.3 ± 11.6 | 0.34 † |
| T10 | 76.4 ± 12.2 | 72.3 ± 10.8 | 0.16 † |
| T20 | 76.7 ± 11.4 | 71.9 ± 11.9 | 0.11 † |
| HR (bpm) | |||
| T5 | 70.3 ± 10.4 | 72.8 ± 11.4 | 0.36 † |
| T10 | 69.6 ± 10.6 | 70.6 ± 12.6 | 0.74 † |
| T20 | 69.5 ± 10.2 | 70.5 ± 13.4 | 0.76 † |
| SpO2 (%) | |||
| T5 | 98.2 ± 1.7 | 98.1 ± 1.6 | 0.76 † |
| T10 | 98.8 ± 1.3 | 98.6 ± 1.4 | 0.65 † |
| T20 | 99.2 ± 1.2 | 98.7 ± 1.4 | 0.14 † |
| Ramsay | |||
| T5 | 4 | 3 | 0.18 ‡ |
| T10 | 3 | 3 | 0.20 ‡ |
| T20 | 3 | 3 | 0.91 ‡ |
| OASS | |||
| T5 | 12 | 11 | 0.49 ‡ |
| T10 | 13 | 13 | 0.74 ‡ |
| T20 | 14 | 13 | 0.56 ‡ |
Note: Data are presented in absolute and relative frequency (%); mean ± standard deviation and median (minimum-maximum), when applicable. † Statistical analysis performed with the Student t-test; ‡ Statistical analysis performed with the Mann-Whitney U test ; T5-five minutes after the block; T10-ten minutes after the block; T20-twenty minutes after the block.
Abbreviations: IOP-Intraocular Pressure; SBP-Systolic Blood Pressure; DBP-Diastolic Blood Pressure; HR-Heart Rate; SpO2-Oxygen Saturation in the blood; OASS-Ocular Anesthetic Scoring System.
Table 2: Clinical characteristics among patients undergoing peribulbar block in vitreoretinal surgeries comparing the addition of clonidine with control.
There was no difference between the groups regarding postoperative analgesia 30 minutes after the block (p=0.53). In total, 22 patients reported pain 24 hours after the block, requiring the use of analgesics. Of these, 15 (68%) belonged to the control group and 7 (32%) to the clonidine group (p=0.03). Pain intensity was considered moderate (score 3 to 7) or intense (score 8 to 10) by 9 (82%) patients in the control group and by only 2 (18%) in the clonidine group (p=0.02). Based on these data, the statistical analysis showed a higher frequency of pain complaints and higher pain scores in the control group.
Discussion
Since its creation in 1986 by Davis and Mandel, peribulbar block has become an important and safe option for performing anesthesia in ophthalmic surgeries.
Ropivacaine is a local anesthetic with characteristics suitable for use in peribulbar anesthesia. It has a short latency, promotes sensitive anesthesia and intense motor block, maintains intraocular pressure and presents a lower risk then bupivacaine for triggering toxic effects on the cardiovascular system [13].
In ophthalmic surgery, the α -agonist clonidine was initially used as an oral pre-anesthetic medication, resulting in a reduction in intraoperative stress and IOP [2].
Some studies have evaluated the action of clonidine on eye blocks. Most combined clonidine with local anesthetics for peribulbar block in cataract surgeries. Doses of clonidine between 0.5 μg/kg and 2 μg/kg were used. They found no difference between groups with regard to pain, sedation, satisfaction, akinesia, IOP and postoperative analgesia scores. However, other studies have found a reduction in IOP and latency time, prolongation of anesthesia, analgesia and akinesia, sedative effect, without increasing the frequency of adverse events. For some authors, clonidine 1 μg/ kg is the ideal dose to prolong analgesia and anesthesia, without causing side effects.
Cataract surgery is recognized as a non-painful procedure. Vitrectomy is considered a procedure of longer duration and painful stimulus and, therefore, the effectiveness of clonidine is better evaluated in this condition. There are few studies evaluating the effects of clonidine in retinal surgery.
Some studies have associated 1 mg/kg of clonidine to the solution of local anesthetics (lidocaine and bupivacaine) with adequate analgesia in 85% of patients, with only 15% of patients needing subtenonian supplementation. In another study, they added 0.5 μg/kg of clonidine to a mixture of lidocaine and bupivacaine in retrobulbar block for Vitrectomy: clonidine reduced postoperative pain and prolonged analgesia. Retrobulbar block requires less volume of local anesthetic and probably less dose of clonidine, since the medication is deposited closer to the target nerves. This may explain the effectiveness of the lowest dose of clonidine [17].
Most of the studies cited found an increase in the duration of anesthesia and postoperative analgesia. In the present study, no difference in analgesia was observed 30 minutes after surgery. The use of ropivacaine, a long-lasting local anesthetic, may have masked the effect of clonidine on prolonging the duration of analgesia right after surgery. In previous studies, combinations of local anesthetics with shorter duration of action than ropivacaine were used. In addition, the sample for this study was calculated based on previous studies that did not use active control. Complementary administration of tenoxicam for postoperative analgesia may require a larger sample to reveal the difference. In this study, there was a lower frequency of pain complaints in the group that received clonidine, which may be due to its analgesic effect. It was possible to demonstrate that among patients who reported pain, those who did not receive clonidine had higher pain scores.
Clonidine is known to decrease IOP. The reduction in IOP may be due to the vasoconstrictor effect of ciliary vessels by stimulating postsynaptic α2 receptors distributed in the eyes, decreasing IOP by reducing the production of aqueous humor and increasing uveoscleral flow. Another possibility is that arterial hypotention, which can be caused by the administration of clonidine, can contribute to the reduction of IOP. Clonidine can affect blood pressure due to its action at multiple sites in the CNS (nucleus of the solitary tract and locus coeruleus), spinal cord and peripherally. Imidazoline receptors are also involved in the hypotensive effects of clonidine [18,19].
In the present study, the addition of 1 μg/kg clonidine caused a reduction in IOP, according to what was found by other authors. However, unlike what was found by these authors, there were no undesirable side effects, perhaps due to the lower dose of clonidide used. Since no patient had hypotension, we can say that there was no influence of this factor in the reduction of IOP found in the study.
After clonidine administration, bradycardia can occur due to the central sympatholytic action or direct vagomimetic action. In the present study, no patient had hypotension or bradycardia. This suggests that, at the dose used, the action of clonidine after administration on the block was mainly limited to the local effect.
Sedation commonly accompanies the use of clonidine in regional anesthesia, with minimal effect on ventilation. Anxiolytic effect has been demonstrated regardless of sedation. In the study, no patient had hypoxia and all had minimal sedation.
As limitations of this study, it can be mentioned that the anesthesia blocks were not all performed by the same anesthesiologist and the surgeries were not performed by the same surgeon. In addition, the sample size based on previous studies may have masked the difference in analgesic effect between groups.
The study contributed to the evidence that the addition of clonidine to the local anesthetic ropivacaine in peribulbar block reduces IOP, the frequency of pain complaints and the intensity of pain. In addition, it demonstrated that with the dose of 1 μg/ kg there were no side effects.
Conclusion
In conclusion, this study shows that the addition of 1 μg/ kg clonidine to 0.875% ropivacaine in peribulbar block for vitreoretinal surgeries reduces the frequency of pain complaints, pain intensity and IOP without causing side effects.
Conflict of Interest
The authors have declared that no competing interest exists.
Contributions
LMCT, CSG and MASA worked on the conception and design of the research, the analysis and interpretation of data, the writing of the article and the approval of the version to be published. DBM, LGM, LCAL and EM worked on data analysis and interpretation, writing the article and approving the version to be published.
REFERENCES
- Davis DB, Mandel MR. Posterior peribulbar anesthesia: An alternative to retrobulbar anesthesia. J Cataract Refract Surg. 1986; 12(2): 182-184.
- Karam VGY, Sayyid SMS, Abi Nader EL, Barakat DE, Karam HS, Cherfane GM, et al. Supplementation of retrobulbar block with clonidine in vitreoretinal surgery: Effect on postoperative pain. J Clin Anesth. 2011; 23(5): 393-397.
- Oliveir CRD, Nogueira CS. Tratado de Anestesiologia, 7th edn, São Paulo. Atheneu. 2011: 401-427.
- Wallace AW, Galindez D, Salahieh A, Layug EL, Lazo EA, Haratonik KA, et al. Effect of clonidine on cardiovascular morbidity and mortality after noncardiac surgery. Anesthesiology. 2004; 101(2): 284-293.
- Nishina K, Mikawa K, Uesugi T, Obara H, Maekawa M, Kamae I, et al. Efficacy of clonidine for prevention of perioperative myocardial ischemia: A critical appraisal and meta-analysis of the literature. Anesthesiology. 2002; 96(2): 323-329.
- Pöpping DM, Elia N, Marret E, Wenk M, Tramèr MR, Warner DS, et al. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks: A meta-analysis of randomized trials. Anesthesiology. 2009; 111(2): 406-415.
- Barioni MFG, Lauretti GR, Pereira NL, Pharm B. Clonidine as Coadjuvant in Eye Surgery : Comparison of Peribulbar versus Oral Administration. J Clin Anest. 2002; 14(2): 140-145.
- Bahy Eldeen HM, Faheem MR, Sameer D. Use of clonidine in peribulbar block in patients undergoing cataract surgery. Austr J Bas & App Sci. 2011; 5:247.
- Madan R, Bharti N, Kaul HL, Shende D, Khokhar SK. A Dose Response Study of Clonidine with Local Anesthetic Mixture for Peribulbar Block: A Comparison of Three Doses. Anesth Analg. 2001; 93(6): 1593-1597.
- Mjahed K, Harrar N, Hamdani M. Lidocaine-clonidine retrobulbar block for cataract surgery in the elderly. Reg Anesth Pain Med. 1996; 21(6): 569-575.
- Bharti N, Madan R, Kaul HL, Khokhar SK, Mishra S. Effect of addition of clonidine to local anaesthetic mixture for peribulbar block. Anaesth Intensive Care. 2002; 30(4): 438-441.
- Connelly NR, Camerlenghi G, Bilodeau M, Hall S, Reuben SS, Papale J. Use of Clonidine as a Component of the Peribulbar Block in Patients Undergoing Cataract Surgery. Reg Anesth Pain Med. 1999; 24(5): 426-429.
- Govêia CS, Magalhães E. Anestesia peribulbar com ropivacaína: Estudo da ação vasoconstritora. Rev Bras Anestesiol. 2010; 60(5): 495-512.
- Consales G, Chelazzi C, Rinaldi S. Bispectral index compared to Ramsay score for sedation monitoring in intensive care units. Minerva Anestesiol. 2006; 72: 329-336.
- Bishop PN, Liyanage S, King T, Kapetanovic JC, Muldoon M, Wearne IM. A novel Ocular Anaesthetic Scoring System, OASS, tool to measure both motor and sensory function following local anaesthesia. Br J Ophthalmol. 2010; 94(1): 28-32.
- Nicoll JMV, Treuren B, Acharya AP, Ahlen K, James M. Retrobulbar anesthesia: The role of hyaluronidase. Anesth Analg. 1986; 65(12): 1324-1328.
- Calenda E, Quintyn JC, Brasseur G. Peribulbar anaesthesia using a combination of lidocaine, bupivacaine e clonidine in vitreoretinal surgery. Indian J Ophthalmol. 2002; 50: 205-208.
- Arthur S, Cantor LB. Update on the role of alpha-agonists in glaucoma management. Exp Eye Res. 2011; 93: 271-283.
- Khan ZP, Ferguson CN, Jones RM. Alfa-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role. Anaesthesia. 1999; 54(2): 146-165.
Citation: Teixeira LMC, Goveia CS, Amorim MAS, Miranda DBD, Moreira LG, Ladeira LCA, et al. (2021) Addition of Clonidine in Peribulbar Anesthesia for Vitreoretinal Surgeries: Randomized, Double-Blind Clinical Trial. J Surg Anesth. 5:161.
Copyright: © 2021 Teixeira LMC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
