Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
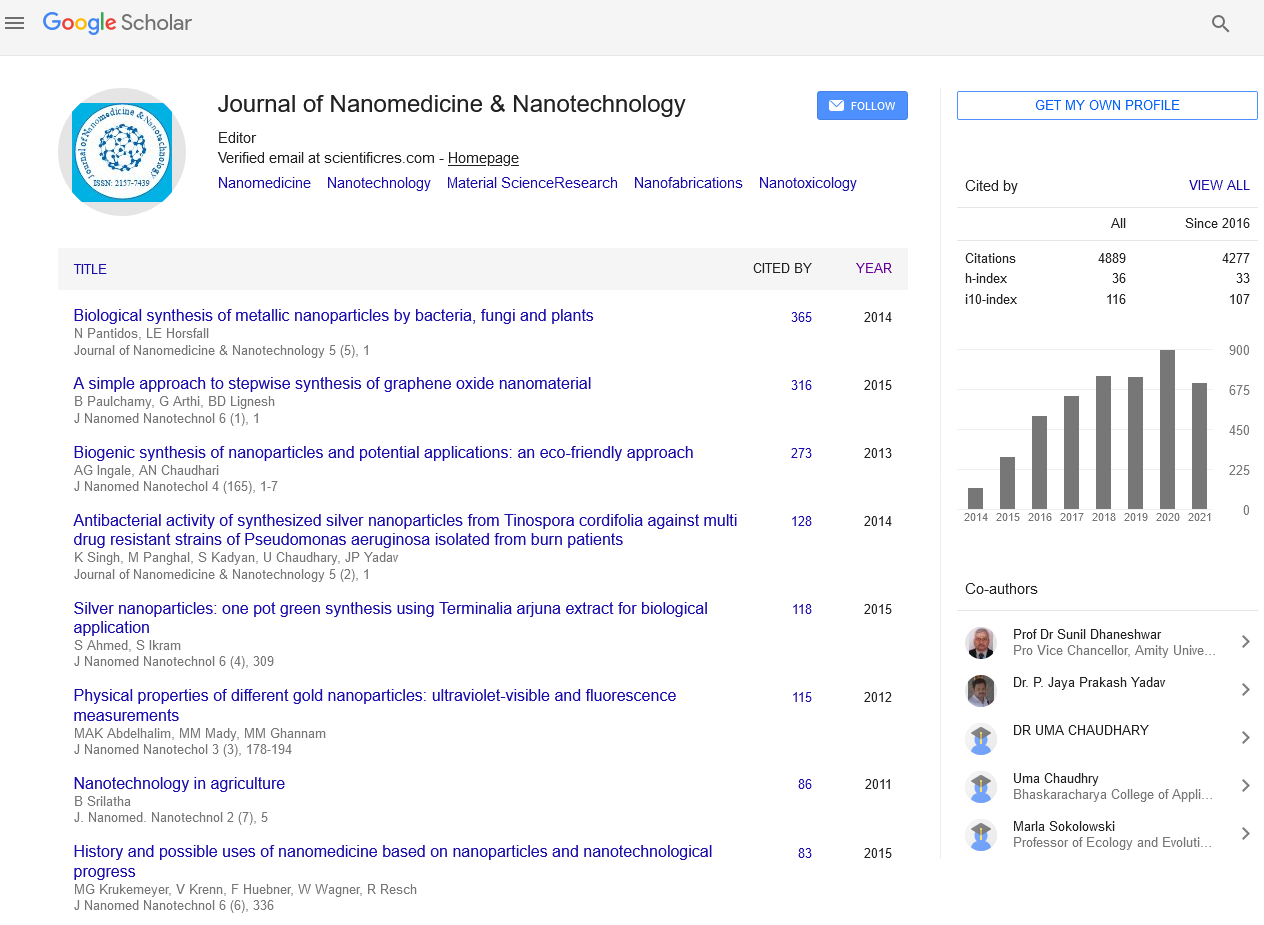
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2022) Volume 13, Issue 12
Acquiring to Cancer Stem-Like Cells with Targeted Nano Medicine has Potential for Use in Medicine
Vamshi P*Received: 03-Dec-2022, Manuscript No. jnmnt-22-19448; Editor assigned: 05-Dec-2022, Pre QC No. jnmnt-22-19448 (PQ); Reviewed: 19-Dec-2022, QC No. jnmnt-22-19448; Revised: 21-Dec-2022, Manuscript No. jnmnt-22-19448 (R); Published: 28-Dec-2022, DOI: 10.35248/2157-7439.22.13.654.
Abstract
Multiple drug resistance (MDR) to chemotherapeutic medicines, both inherited and acquired, is a significant barrier to effective cancer treatment. P-glycoprotein and multidrug-resistance-associated proteins are examples of the ATP Binding Cassettes (ABC) transporter super family, which function as extrusion pumps. Blocking the pump proteins physically can tilt the balance between drug input and efflux toward an accumulation of the drug inside the cell, which eventually leads to cell death [1]. This is one of the most effective ways to control the active drug's efflux from the cells. Drugs approved for uses other than treating cancer included MDR modulators, commonly referred to as Chemosensitizers. However, their clinical use is limited by their toxicity, side effects, and low solubility at levels needed to reverse MDR. Prior studies have demonstrated that medications from the selective serotonin reuptake inhibitor (SSRI) family, which are routinely utilised as antidepressants, can function as efficient Chemosensitizers both in vitro and in vivo in tumor-bearing animal models [2]. In this study, we investigated the potential of sertraline (Zoloft®), a member of the SSRI family of drugs, to act as an MDR modulator. Using another FDA-approved medication in combination with sertraline.
Keywords
Chemosensitizers; Drug ResistanceIntroduction
Even while contemporary anticancer medicines work well in the early stages of treatment, recurrences happen frequently. Such recurrences are frequently metastatic and unresponsive to standard treatments. Cancer stem-like cells (CSCs), a tiny subpopulation of cells within tumours, have stem cell-like characteristics that enable them to start and support tumour growth [3]. The start and metastasis of tumours, as well as cancer recurrence following traditional therapies, are assumed to be caused by CSCs. Leukemia, breast, brain, colon, lung, and prostate cancer are just a few of the cancers in which CSCs have been found. The bulk of standard cancer treatments, including hormonal, radiation, and chemotherapy, might not completely eradicate CSCs, though [4]. Even though the specifics of CSC biology still need to be better understood, a lot of work is presently being put into therapeutic targeting of CSCs as a novel approach for drug discovery for the treatment of cancer and the prevention of recurrence. The creation of efficient ways to deliver the treatments to the CSCs particularly poses the biggest barrier to CSC-specific therapies, nevertheless [5]. Specifically targeting primary and metastatic tumour cells is a requirement before focusing on CSCs. Affinity ligands, such as RGD, iRGD, NGR peptide, folate, antibodies against human epidermal growth factor receptor transferrin receptor (TfR), or aptamers that bind the prostate-specific membrane antigen, can be added to delivery systems to enable tumor-specific targeting. Each ligand or antibody is designed to engage with its corresponding receptor or antigen to target malignancies [6]. We have demonstrated that the scL nanocomplex is capable of efficiently and selectively delivering a variety of payloads into primary and metastatic cancers in vivo, while showing high selectivity for abnormal cells such liver hepatocytes. The self-assembled, biodegradable, scL nanocomplex has been demonstrated to have deep tumour penetration when systemically administered in both primary and metastatic disease, leading to long-term tumour elimination (often without recurrences) and life extension in numerous animal models of human cancer [7]. Here, we present evidence demonstrating the ability of scL to effectively target and deliver payloads to both CSCs and differentiated non- CSCs in vitro and in a number of mouse cancer models, including xenografts of human brain and colorectal cancer, syngeneic mouse breast tumour and melanoma, and chemically induced mouse lung and liver cancers. In a mouse model of human colorectal cancer xenografts, we also report that systemically administered scL-p53 inhibited tumour development and caused apoptosis in both CSCs and non-CSCs, demonstrating a strong anticancer effect [8].
Cscs Are Targeted In Vitro by Scl
We anticipated that scL might target CSCs if CSCs also overexpress TfR as the scL nanocomplex targets TfR overexpressed on the surface of cancer cells. To remedy this, we examined the degree of TfR expression in human colorectal cancer CSCs (HT-29, HCT- 116) utilising CSC markers (CD133, CD166, CD44, EpCAM, Msi1, and Nanog). All of the human colorectal cancer cell lines were found to express elevated levels of TfR, which were similar in CSCs (CD133+CD166+CD44+, EpCAMhighCD166+CD44+, Msi+Nanog+, or CD133+), unselected populations, and noncancerous human lung fibroblasts, IMR-90. This is in contrast to the low TfR expression found in non-cancerous human lung fibroblasts. The higher expression of TfR in both populations of HT-29 cells than that observed in non-cancerous IMR-90 cells was validated by Western blot analysis of immunomagnetically sorted CD133+ and CD133 populations. Using various CSC markers, the expression of TfR in CSCs of human brain cancer cells (U251, U87, LN-18, and T98G) was also examined (CD133, Nestin, SSEA- 1, Nanog, and Msi1). The upregulation of TfR was seen in both CSCs (CD133+Nestin+, CD133+Msi1+, or SSEA-1+Nanog+) and unselected populations, as was the case with the colorectal cancer cells. All brain cancer cell lines had a similar shift to that seen in the colorectal cancer cells [9].
Scl-Mediated Transgene
We transfected HT-29, HCT-116, U251 and U87 cells with scL containing GFP plasmid DNA to measure transfection efficiency and assess functioning of the delivered payload in CSCs (scLGFP). We identified CSCs 48 hours after transfection using Texas Red-labeled anti-CD133 antibodies. HT-29, U251, and U87 cells showed localization of GFP in the cytoplasm of Texas Red-labeled cells. The most important factor from a therapeutic perspective is the capacity to distribute and express wtp53 in CSCs and non- CSCs. In order to show that the scL nanocomplex can successfully deliver p53 to both CSCs and non-CSCs, we transfected HT-29 cells with the scL nanocomplex and a GFP-tagged wtp53 expression plasmid that encodes a GFP-p53 fusion protein as the payload. Using antibodies against CSC markers, the cells were collected and FACS-sorted 24 hours after transfection (CD133, CD166, and CD44). Additionally, untransfected cells were sorted to be used as a control [10]. The GFP-p53 fusion protein was expressed in both CSCs and non-CSCs, according to a Western blot examination of both sorted CSCs (CD133+CD166+CD44+) and non-CSCs (flow through cells) [11].
Effect of Scl-Delivered
the efficiency of scL-mediated therapeutic drug delivery on CSCs. Using the XTT cell survival assay, we investigated in vitro how scL-delivered wtp53 DNA affected CD133+ CSCs and CD133 non-CSCs from colorectal (HT-29, HCT-116) and brain (U251, U87) cancer cells. The graphs show the average of three duplicate samples [12]. Controls were treatment with liposome alone (Lip) and scL containing an empty plasmid vector (scL-vector). In all of the investigated cell lines, scL-p53 transfection led to a statistically significant rise in cell mortality. More significantly, scL-p53 produced comparable effects (identical IC50 values) in CD133+ CSCs and CD133 non-CSCs [13-15].
CONCLUSION
Western blot analysis was done to ascertain the TfR expression level. Twenty micrograms of total cellular protein were separated by 8% SDS-polyacrylamide gel electrophoresis, transferred to nylon membrane, and hybridised with anti-human TfR antibody from non-cancerous normal human fibroblast cell line IMR-90 and immunomagnetically sorted CD133+ and CD133 population of HT-29 cells. In the western blots, an antibody recognizing glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was utilized as an internal control for equal protein loading.
REFERENCES
- Furtek SL, Backos DS, Matheson CJ, Reigan P. Strategies and Approaches of Targeting STAT3 for Cancer Treatment. ACS Chem Biol. 2016; 11:308-318.
- WHO. Cancer Fact Sheet; WHO: Geneva, Switzerland, 2021.
- Ferlay J, Ervik M, Lam F, Colombet M, Mery L. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020.
- Brown JM, Wilson WR. Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer. 2004; 4:437-447.
- Pennya LK, Wallace HM. The challenges for cancer chemoprevention. Chem Soc Rev. 2020; 44: 8836-8847.
- Rahim NFC, Hussin Y, Aziz MNM, Mohamad NE, Yeap SK. Cytotoxicity and Apoptosis Effects of Curcumin Analogue (2E,6E)-2,6-Bis(2,3-Dimethoxybenzylidine) Cyclohexanone (DMCH) on Human Colon Cancer Cells HT29 and SW620 In Vitro. Molecules. 2021; 26:1261.
- Naksuriya O, Okonogi S, Schiffelers RM, Hennink WE. Curcumin nanoformulations: A review of pharmaceutical properties and preclinical studies and clinical data related to cancer treatment. Biomaterials. 2014; 35:3365-3383.
- American Cancer Society. Cancer Treatment & Survivorship Facts & Figures; American Cancer Society: Atlanta, GA, USA, 2019–2021.
- Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR. Cancer treatment and survivorship statistics. J Clin. 2019; 69:363-385.
- Hsu RS, Fang JH, Shen WT, Sheu YC, Su CK. Injectable DNA-architected nano raspberry depot-mediated on-demand programmable refilling and release drug delivery. Nanoscale. 2020; 12:11153-11164.
- Ismail NI, Othman I, Abas F, Lajis NH, Naidu R. The Curcumin Analogue, MS13 (1,5-Bis(4-hydroxy-3-methoxyphenyl)-1,4-pentadiene-3-one), Inhibits Cell Proliferation and Induces Apoptosis in Primary and Metastatic Human Colon Cancer Cells. Molecules. 2020; 25:3798.
- Fardjahromi MA, Nazari H, Tafti SMA, Razmjou A, Mukhopadhyay S. Metal-organic framework-based nanomaterials for bone tissue engineering and wound healing. Mater Today Chem. 2021; 23:100670.
- Thomas A. Functional Materials: From Hard to Soft Porous Frameworks. Angew Chem Int Ed. 2010; 49:8328-8344.
- Das S, Heasman P, Ben T, Qiu S. Porous Organic Materials: Strategic Design and Structure–Function Correlation. Chem Rev. 2017; 117:1515-1563.
- Xu ZY, Xu YL, Basuthakur P, Patra CR, Ramakrishna S. Fibro-porous PLLA/gelatin composite membrane doped with cerium oxide nanoparticles as bioactive scaffolds for future angiogenesis. J Mater Chem. 2020; 8:9110-9120.
Google Scholar, Crossref, Indexed at
Citation: Vamshi P (2022) Acquiring to Cancer Stem-Like Cells with Targeted Nano Medicine has Potential for Use in Medicine. J Nanomed Nanotech. 13: 654.
Copyright: ©2022 Vamshi P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.