Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 0, Issue 0
A Rare Case of PAF Comorbid with Epilepsy: Differential Diagnosis and Treatment of a Patient in Charge at Outpatient Home Care Clinic
Flora Zarola1* and Profeta B22Department of Nursing, Care Manager Outpatients Clinic Azienda Sanitaria Locale, Albano Laziale, Italy
Received: 17-Nov-2021 Published: 08-Dec-2021
Abstract
Objective: A home care patient who was previously on outpatient clinic care with a suspicion of Parkinson's disease was taken in charge. The clinical history reported a poor response to dopaminergic therapy that had been interrupted at the initiative of the patient and his family. Therefore, the initial aim was a better diagnostic definition of a possible extrapyramidal disease and the development of a more effective treatment.
Background: During the previous home visits, some signs suggesting a Parkinsonism such as reduced facial expression and a certain motor slowdown with a slight axial stiffness were found, while along the way an orthostatic hypotension was added to clinical observation. A first new attempt with dopaminergic therapy had given little satisfaction, but in the meantime the presence of reported episodes of a 'lipothymic' type emerged. In order to verify the nature of these episodes, the patient performed tests electroencephalogram (EEG) that showed signs compatible with epilepsy.
Case: During the observation period the patient underwent to pressure measurement in ortho- clino-statism; the patient was subjected to EEG, electromyography (EMG), blood tests (B12 dosage) brain MR scan and DAT-Scan.
Results: From the tests performed, the patient resulted affected by epilepsy, a drastic drop in pressure when standing, signs of slight peripheral polyneuropathy, and positivity of the DAT-Scan due to a reduction in the uptake of the presynaptic tracer.
Conclusion: Therefore the patient was subjected to anti-epileptic therapy which resulted in a frequency reduction of episodes of consciousness loss, dopaminergic therapy at low doses, application of elastic stockings and hydration. To date, the patient has undergone a worsening evolution of the clinical picture relating to orthostatic hypotension.
Keywords
Epilepsy; Seizures; Orthostatic hypotension; Paf; Vascular epilepsy; Therapy; Parkinson disease; Atypical parkinsonism; Aging
Introduction
A home care patient who was previously on outpatient clinic care with a suspicion of Parkinson's disease was taken in charge. The clinical history reported a poor response to dopaminergic therapy that had been interrupted at the initiative of the patient and his family. Therefore, the initial aim was a better diagnostic definition of a possible extrapyramidal disease and the development of a more effective treatment. During the previous home visits, some signs suggesting a Parkinsonism such as reduced facial expression and a certain motor slowdown with a slight axial stiffness were found, while along the way an orthostatic hypotension was added to clinical observation. A first new attempt with dopaminergic therapy had given little satisfaction, but in the meantime the presence of reported episodes of a 'lipothymic' type emerged. In order to verify the nature of these episodes, the patient performed tests electroencephalogram (EEG) that showed signs compatible with epilepsy.
Case Representation
A male patient, 78 yrs aged, was examined for the first time in July 2018 for walking impairment and frequent falls, some of which with loss of awareness. In the past he was diagnosed with Parkinson's disease in other clinical centers and treated with dopaminergic therapy which was subsequently discontinued due to poor efficacy. At the time of our examination, the patient showed: slight hypomimia, axial stiffness, unstable walking, and poor pendular movement at upper limbs, slight plastic hypertonus, and no cognitive impairment. A low-dose and softly-increasing of dopaminergic therapy was tried again, according to the response of DAT-scan result, which showed presynaptic dopaminergic impairment of basal ganglia, but was interrupted due to poor efficacy and early presence of side effects (hallucinations) (Figure 1).
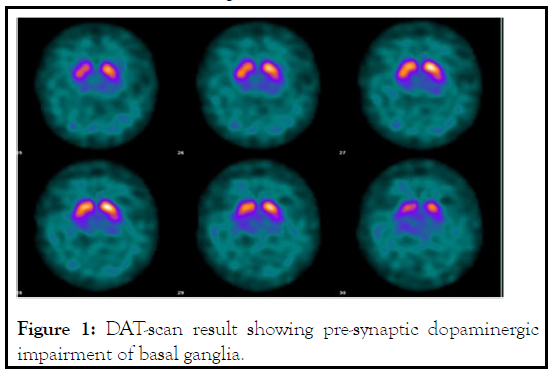
Figure 1: DAT-scan result showing pre-synaptic dopaminergic impairment of basal ganglia.
Subsequently, due to the increase in the frequency of falls, some of which associated with loss of consciousness or slight confusion, the patient was subjected to blood pressure measurement in the sitting position and in orthostatism, which highlighted a severe fall of the values (from 140/80 mmHg to 80/n.r. mm Hg in 10 seconds with compensatory tachycardia) of blood pressure and which clinically corresponded to intense paleness and impairment of standing position. However, some of the reported episodes were characterized by elements of suspected epileptic nature consisting of tonic-clonic shaking, screaming and urine loss. This data were matched with the brain MR scan carried out which showed signs of temporal-occipital atrophy and diffuse vascular brain suffering. Consequently we suspected the coexistence of epilepsy. Therefore, an EEG was performed which documented slow frontal-temporal dysrhythmias. As a consequence the patient underwent therapy with anti-crisis drugs with an improvement in the frequency of the episodes described in anamnesis by the family members, i.e. a reduction in the frequency of falls with loss of awareness preceded or not by confusional state. Moreover a control recording two months subsequent to antiepileptic drugs medication showed also an improvement of organization of the EEG.
Results and Discussion
Pure Autonomic Failure (PAF) is a well-known disorder of α- synuclein deposition that results in neurogenic orthostatic hypotension and other features of autonomic failure, without signs of central nervous system involvement. Neurological examination of a patient with PAF is not usually accompanied by signs of movement impairment. Autonomic failure may also manifest other dysfunctions of genitourinary, gastroenteric and thermoregulatory systems. The difficulty to make a diagnosis in such patients consists in the non-specificity of many symptoms that when in suspicion of a cognitive disorder or an extrapyramidal pathology can be underestimated even for a long time and therefore escape the correct diagnostic necessary maneuvers such as the simple measurement of blood pressure in various positions, or the request for tests such as EEG [1]. Furthermore, the evaluation of this pathological condition requires a multidisciplinary approach which is often made difficult in the patient's home care. The interest of this clinical case consists in the difficulty of discriminating the nature of the critical episodes in a patient suffering from this rare disease, which had not previously been diagnosed despite the relevant anamnestic data of frequent and severe falls, some of which with significant trauma. In fact it is known in clinical practice that in Parkinson's disease, but especially in some atypical parkinsonism, falls are a frequent and relevant symptom; however, the patient studied presented other signs, such as intense paleness and mental confusion when standing, which have not previously been sufficiently stressed. It is interesting to note that, although the DAT-scan which was performed during the diagnostic procedure had a suggestive outcome for presynaptic dopaminergic damage, the dopaminergic therapy was not effective and gave severe side effects even at low doses such as to make it impossible to use. The second element of interest consists in the difficulty of identifying the coexistence of epilepsy [2]. It is known that an epileptic seizure can rise even if rarely during hypotension with loss of consciousness: in fact an epileptic seizure can be due to acute cerebral hypoxia. However, in this case, the high frequency of such episodes, associated with real seizures of Grande Male type, or focal seizures with bilateral evolution, improved with the antiepileptic treatment, which at the same time allowed discriminating the epileptic seizures from 'simple' hypotensive seizures or lipothymias. The nature of the epilepsy in this patient is uncertain: in the absence of a familiarity, a secondary nature due to the atrophy or chronic hypoxic brain damage documented by the brain RM-scan remains probable.
This patient is affected by a severe form of PAF with rapid worsening progression with a severe drop in standing blood pressure and current impossibility to maintain the upright and sitting position even for a few seconds. Moreover, since the patient is on antiepileptic drug treatment, the phenomena of loss of consciousness have no longer been associated with tonicclonic seizures or other characteristics attributable to epileptic seizures. PAF is commonly believed to be characterized by normal EEG and MRI; in this patient, on the other hand, abnormalities in both EEG and MRI of the brain compatible with cerebrovascular disease (CVD) have been observed. Our previous studies have shown that CVD is often the cause of secondary epileptic disease [3-7].
Conclusion
Therefore it is reasonable to assume that this case represents a particular comorbidity between PAF, CVD and epilepsy. The possible correlation between the autonomic disorder and the other pathologies described in this patient remains uncertain. The importance of always making a differential diagnosis in cases presenting syncopal symptoms on a dysautonomic basis remains interesting.
Acknowledgement
The author wishes to thank the Nurse Coordinator Francesco Pepe and the staff, the Coordinator of Outpatient Clinic Dr Rita Bartolomei, and Director of the district 2 RM6 Dr Pierluigi Vassallo, for their supporting and organizing work.
REFERENCES
- Kaufmann H, Norcliffe-Kaufmann L, Palma JA, Biaggioni I, Low PA, Singer W, et al. The natural history of pure autonomic failure: a United States prospective cohort. Ann Neurol. 2017;81(2): 287-297.
- Isonaka R, Holmes C, Cook GA, Sullivan P, Sharabi Y, Goldstein DS. Pure autonomic failure without synucleinopathy. Clin Auton Res. 2017;27(2): 97-101.
- Zarola F, Middei B. Occurrence of epileptic complications in patients with cerebrovascular disease in charge to the home care center: a clinical experience. J Biomed Res Environ Sci. 2021;2(3): 213-215.
- Zarola F. Efficacy of Lacosamide on an aged patient with behavioural impairment consisting in impulse dyscontrol, aggressiveness and insomnia. J Neurosci Neurosurg. 2019;2(4): 139.
- Zarola F. Incidence of brain vascular damage in a population with parkinson's disease: statistical comparison by age subassemblies with age homogeneous control groups cureus. 2020;12(6): e8778.
- Zarola F. Incidence of vascular brain damage in a population with Parkinson Disease: a clinical statistic study in comparison with a control group of patients afferent to neurological movement disorder outpatients clinic. Acta Biomed. 2017;88(1): 95-96.
- The portal for rare diseases and orphan drugs. 2021.
Citation: Zarola F, Profeta B (2021) A Rare Case of PAF Comorbid with Epilepsy: Differential Diagnosis and Treatment of a Patient in Charge at Outpatient Home Care Clinic. J Aging Sci. S9: 001.
Copyright: © 2021 Zarola F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

