Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 11, Issue 5
A Rare Case of Haemangioma around Common Carotid Artery
Anismita Das*, Ajay Dayma and Ashwini Kumar SeelamReceived: 31-Aug-2023, Manuscript No. JVMS-23-22808; Editor assigned: 04-Sep-2023, Pre QC No. JVMS-23-22808 (PQ); Reviewed: 25-Sep-2023, QC No. JVMS-23-22808; Revised: 02-Oct-2023, Manuscript No. JVMS-23-22808 (R); Published: 09-Oct-2023, DOI: 10.35248/2329-6925.23.11.537
Abstract
Background: Haemangioma are benign neoplasms derived from blood vessels which multiply at an abnormal rate and form a mass or lump. Most Haemangioma common in infant and also common in female than male. They can occur throughout the body, including in skin, muscle, bone, and internal organs. It mostly occur on the surface of the skin or just beneath it. They often develop on the face and neck, and can vary greatly in colour, shape, and size. Deep Haemangioma tends to grow later and longer than superficial ones. Patients often remain asymptomatic or present with nonspecific symptoms, such as headache. This is the first Haemangioma to be reported as encircled the common carotid artery. Carotid sheath Haemangioma may be easily misdiagnosed as arterial aneurysms, neurogenic tumors, paragangliomas, or lymphatic masses.
Case presentation: We report a case of Haemangioma in a 33 years female, who presented with gradually progressive swelling at lateral side of left neck for 7 years. She also complained of pain in the left side of face, neck and hand for 15 days. Mass presented from the carotid bifurcation to superior mediastinum. The diagnosis couldn’t be stated on the basis of history, clinical and radiological examination findings.
Results: Successful surgical excision of the Haemangioma is performed with precise dissection which engulfed common carotid artery. Histopathological examination confirms the diagnosis of haemangioma.
Conclusion: A rare case of haemangioma presented with circumferentially encased common carotid artery from carotid bifurcation to superior mediastinum. Haemangioma was successfully excised without any surgical complication.
Keywords
Haemangioma; Common carotid; Arterial; Tumor
Introduction
Hemangioma is benign neoplasm derived from blood vessels which multiply at an abnormal rate and form a mass or lump. They can occur throughout the body, including in skin, muscle, bone, and internal organs. Most hemangioma occurs on the surface of the skin or just beneath it. They often develop on the face and neck, and can vary greatly in color, shape, and size. Hemangioma is more common in infant and also common in female than male [1-3].
Types of hemangiomas
There are several types of Hemangiomas. Some of them are described below:
• Capillary hemangioma: This is the most common type of Hemangioma. It is made up of small capillaries that are normal in size and diameter, but high in number. It develops in the skin and often superficial. They are typically bright red in color. They can be small or large in size and may be flat to the skin, raised, or protrude out as a nodule.
• Cavernous hemangioma: It made up of larger blood vessels that are dilated. When they develop in the skin, cavernous Hemangioma is often referred to as deep, and sometimes first appear as a bluish swelling underneath the skin. This type also varies greatly in size and can occur throughout the body.
• Compound hemangioma: Some hemangioma is a mix of the capillary and cavernous types.
• Lobular capillary hemangioma: They are small, red often appear on the hands, face, and arms. Because they contain so many blood vessels, they bleed easily with trauma. This type of Hemangioma is also sometimes referred to as a pregnancy tumor because they often appear during pregnancy, typically in the nose and mouth.
Deep hemangioma tends to grows later and larger than superficial ones. Patients often remain asymptomatic. This is the first case of Hemangioma to be reported as encircled the common carotid artery. Carotid sheath Hemangioma may be easily misdiagnosed as arterial aneurysms, neurogenic tumors, para gangliomas, or lymphatic masses [4].
Case Presentation
A 33 years female presented to the surgery Out Patient Department (OPD) with a chief complaint of a painless swelling in the left side of the neck. The swelling had been present for the past 7 years and had a gradual progressive course. Over the past 2 months, the patient complained of numbness over the neck, face, and radiating to the hand. The patient experienced pain over the neck while sleeping on the left side of the face. There was no history of trauma, difficulty in breathing, facial puffiness, flushing of face, difficulty in deglutition, hoarseness of voice, or palpitations. In the patient's past history, she had tuberculosis during her first pregnancy in 2009 and received Anti-Tuberculosis Therapy (ATT) for 12 months. There was no history of hypertension, diabetes, asthma, or any other comorbid illness. The patient had a history of tubal ligation performed in 2015 under spinal anesthesia. Menstrual cycle was regular, with the Last Menstrual Period (LMP) on 18/5/2023.
Results
Physical examination findings
• General examination revealed the patient is normal build, weighing 39 kg, with a height of 156 cm.
• No pallor, icterus, lymphadenopathy, edema, or clubbing was noted.
Vital signs
• Pulse rate: 98/min, regular rhythm on left radial artery.
• Blood pressure: 110/80 mmHg. On left upper limb.
• Respiratory rate: 16/min. thoraco-abdominal.
• Oxygen saturation (SpO2): 98% on room air.
Systemic examination
• Chest examination revealed bilaterally equal air entry with no added sounds.
• Cardiovascular examination detected the presence of normal S1 and S2 heart sounds.
Physical examination
Presence of a single non-pulsatile, non-tender mass on the left side of the neck from carotid bifurcation to supra sternal notch, which is 7 × 4 cm² cylindrical shaped with regular margins and firm in consistency without associated tenderness or skin changes. There is no engorged veins or tracheal deviation. No Fluctuation and trans-illumination.
These physical examination findings provide valuable information for further evaluation. Additional investigations done to determine the nature of the neck swelling and establish an appropriate diagnosis and treatment (Figure 1).
Figure 1: Physical examination of hemangioma around common carotid artery.
Preoperative investigations
Present the results of relevant preoperative investigations, including:
Haemogram:
• Hemoglobin: 12.3 g/dl
• Total leukocyte count (TLC): 5.65 × 10^3/μl
• Platelets: 206 × 10^3/μl
PT/INR:
• Prothrombin Time (PT): 12.8 seconds
• International normalized ratio (INR): 0.94
Random blood sugar: 86 mg/dl
T3–1.5
T4–8.6
TSH–3.4
Special investigation
X-ray neck: Examination of the tumor on the neck by using X-ray (Figure 2).
Figure 2: X-ray of the neck of hemangioma around common carotid artery.
USG neck: Large well defined heteroechoic lesion measuring approx. 4.3 × 2.7 × 3.2 cm seen on the left side of neck. Peripheral and internal vascularity is seen. The lesion encased the left common carotid artery within it in entire extent. The lower extent of lesion invisualized, retrosternal extent could not be ruled out suggestive of carotid body tumor, schwanoma (Figure 3).
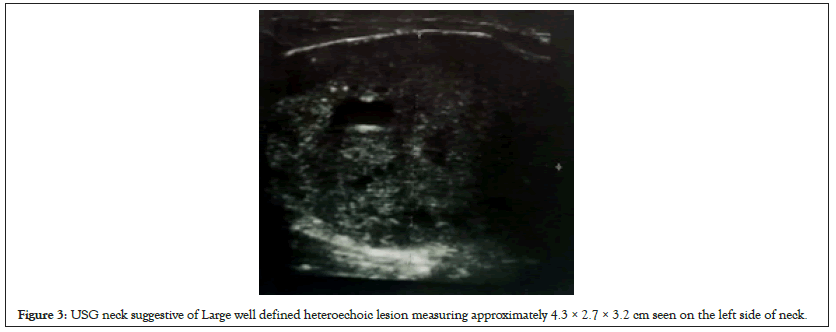
Figure 3: USG neck suggestive of Large well defined heteroechoic lesion measuring approximately 4.3 × 2.7 × 3.2 cm seen on the left side of neck.
Colour doppler of carotid ateries study: A heterogeneously lesion with internal vascularity and cystic areas measuring 80 × 33 × 38 mm noted along the length of left common carotid artery, encircling it upto the bifurcation. Suggestive of carotid body tumor, paraganglioma.
CECT neck: revealing a large vascular mass in the left side of the neck with encasement of the left common carotid artery, consistent with a carotid body tumor (Figure 4).
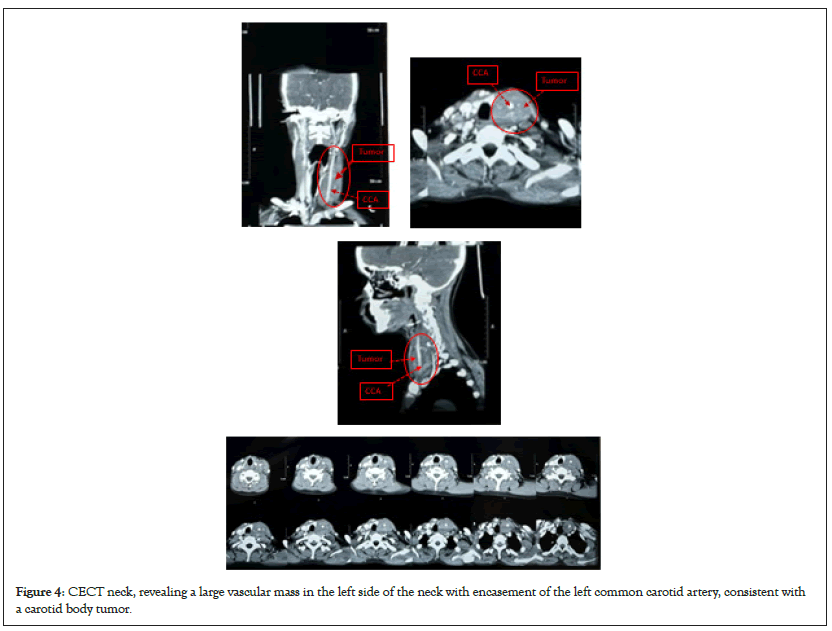
Figure 4: CECT neck, revealing a large vascular mass in the left side of the neck with encasement of the left common carotid artery, consistent with a carotid body tumor.
USG guided FNAC: Done which suggestive of Hemangio-vascular tumor.
Operative finding
• A horizontal incision of 10 cm made above the swelling and deepened through the platysma.
• 7 cm vascular, firm mass present encircling the common carotid artery from sternal notch up to bifurcation of it.
• Took the proximal and distal control of common carotid artery below and above the tumor.
• Then we have created the plane between hemangioma and common carotid artery.
• Cut the tumor above to downwards anterior side with the help of ligasior.
• Once the whole of the tumor dissected and separated from common carotid artery then separate from the other part.
• Rest of the tumor separate from posterior tissues and send for histopathy.
• Romovac placed and closed layer by layer.
• Postoperative care and follow-up continued for the patient's recovery and monitoring of any potential complications (Figure 5).
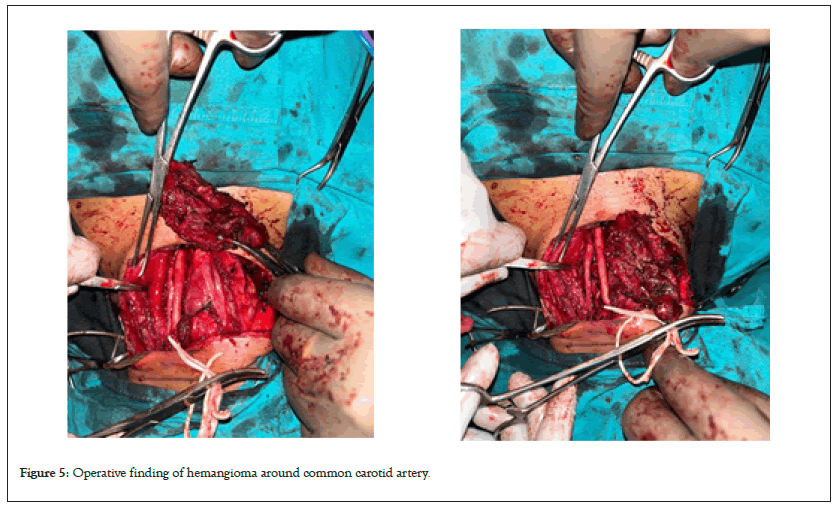
Figure 5: Operative finding of hemangioma around common carotid artery.
Histopathology report
Histopathological report of the specimen is shown in Figure 6.
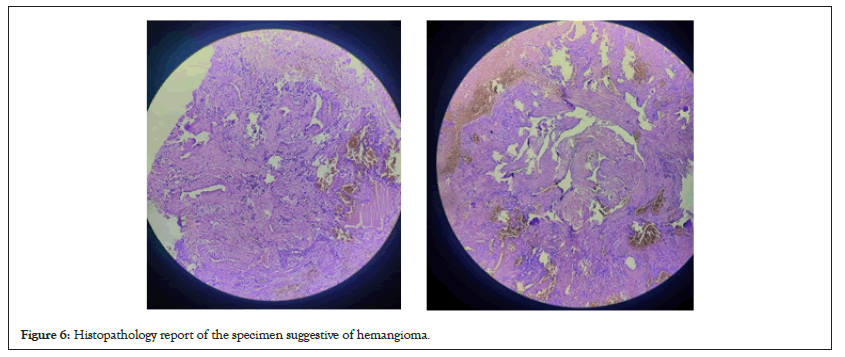
Figure 6: Histopathology report of the specimen suggestive of hemangioma.
Discussion
The data that examines Haemangioma which localized encircled the common carotid artery are extremely rare . They are very often asymptomatic and incidentally discovered. Cavernous Haemangioma is a congenital venous malformation that occurs throughout the entire body but it is rarely localized in the common carotid artery. Histologically, Haemangioma originates from residual embryonic vascular cells and is caused by abnormal vascular development at the embryonic stage. So far, to the best of our knowledge, our case is the first case of cavernous haemangioma encircled common carotid artery reported in the literature [5]. Haemangioma grow by endothelial cell hyperplasia and should be differentiated from vascular malformations, which are not true neoplasms but are localized defects of vascular morphogenesis. Their confirmation always needs a surgical approach followed by histologic evaluations. In our case, neither the ultrasound nor the scanner made the diagnosis [6]. The choice of treatment is dependent on the related organ and can include sclerotherapy, embolization, and surgical resection. Reviewing previously reported cases in the literature and complete surgical resection is generally accepted as the definitive and effective treatment of choice [7,8].
Conclusion
In conclusion, the case presented a 33 years female with a painless swelling in the left side of the neck, which had been progressively growing over a period of 7 years. The patient also reported numbness in the neck, face, and hand, along with pain while sleeping on the left side of the face. Physical examination revealed a non-pulsatile mass on the left side of the neck, measuring approximately 7 × 3 cm.
Preoperative investigations, including hemogram, PT/INR, random blood sugar, Doppler study, and Contrast Enhanced Computed Tomography (CECT) neck, USG guided Fine Needle Aspiration Cytology (FNAC) confirmed the presence of a Hemangioma. The tumor was found to be encircling the left common carotid artery, indicating its involvement with the vasculature. Surgical intervention was performed with the patient under general anesthesia. A horizontal incision was made above the swelling, and the tumour was meticulously dissected, separating its margins from the surrounding tissues and preserving vital structures such as the common carotid artery, internal jugular vein, and vagus nerve. Complete tumor excision was achieved, and hemostasis was ensured. A Romovac drain was placed below the sternocleidomastoid plane for postoperative drainage.
The successful excision of the Hemangioma not only provided relief from symptoms but also addressed the potential risks associated with the tumor's growth and its encasement of the common carotid artery. Postoperative care and regular follow-up will be crucial for monitoring the patient's recovery and evaluating any potential complications.
Overall, the surgical intervention aimed to eliminate the Haemangioma, restore normal vascular flow, and improve the patient's quality of life. The successful management of this case highlights the importance of prompt diagnosis, careful surgical planning, and skilled execution in the field of general surgery.
References
- Anajar S, Nawal B, Amal H, Fouad B. Internal jugular vein cavernous hemangioma occurring as lateral neck mass: Case report. Int J Surg Case Rep. 2021;85:106205.
[Crossref] [Google Scholar] [PubMed]
- Murphy T, Ramai D, Lai J, Sullivan K, Grimes C. Adult neck hemangiolymphangioma: A case and review of its etiology, diagnosis and management. J Surg Case Rep. 2017;2017(8):rjx168.
[Crossref] [Google Scholar] [PubMed]
- Abrahim MJ, Gregory ND, Chennupati SK. Epithelioid hemangioma of the internal carotid artery: a case report supporting the reactive pathogenesis hypothesis of this vascular tumor. Int J Pediatr Otorhinolaryngol. 2014;78(7):1186-1189.
[Crossref] [Google Scholar] [PubMed]
- Al-Muharraqi MA, Faqi MK, Uddin F, Ladak K, Darwish A. Angiolymphoid hyperplasia with eosinophilia (epithelioid hemangioma) of the face: an unusual presentation. Int J Surg Case Rep. 2011;2(8):258-260.
[Crossref] [Google Scholar] [PubMed]
- Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16(5):405-418.
[Crossref] [Google Scholar] [PubMed]
- Kiymaz N, Yilmaz N, Suleyman OZ, Demir I, Gudu BO, Kozan A. Cavernous hemangioma presenting as a giant cervical mass: A case report. Turk Neurosurg. 2010;20(1).
[Google Scholar] [PubMed]
- Antonopoulos C, Karagianni M, Zolindaki C, Anagnostou E, Vagianos C. Cavernous hemangioma of infrahyoid carotid sheath and review of the literature on carotid sheath tumors. Head Nec. 2009;31(10):1381-1386.
[Crossref] [Google Scholar] [PubMed]
- Zagzag J, Morris LG, DeLacure MD. Cavernous hemangioma of the carotid sheath. Otolaryngol Head Neck Surg. 2009;140(4):608-609.
[Crossref] [Google Scholar] [PubMed]
Citation: Das A, Dayma A, Seelam AK (2023) A Rare Case of Haemangioma around Common Carotid Artery. J Vasc Surg. 11:537.
Copyright: © 2023 Das A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

