Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2024) Volume 14, Issue 3
A Case Study on Plummer Vinson Syndrome and MNT
Ushakiran Sisodia*, Rohit Malde and Bharat ChauhanReceived: 09-Sep-2020, Manuscript No. JNDT-24-6422; Editor assigned: 14-Sep-2020, Pre QC No. JNDT-24-6422 (PQ); Reviewed: 28-Sep-2020, QC No. JNDT-24-6422; Revised: 01-Aug-2024, Manuscript No. JNDT-24-6422 (R); Published: 29-Aug-2024, DOI: 10.35248/2161-0509.24.14.299
Abstract
Plummer-Vinson Syndrome (PVS) is a rare disorder characterized by a triad of iron-deficiency anemia, dysphagia due to esophageal webs and glossitis. This case study explores the clinical presentation, diagnosis and management of PVS in a middle-aged female patient, with a particular focus on Medical Nutrition Therapy (MNT) as a key component of treatment. The patient presented with symptoms of fatigue, difficulty swallowing and a burning sensation in the tongue. Laboratory tests confirmed severe iron-deficiency anemia and an endoscopic examination revealed the presence of esophageal webs, consistent with PVS.
The management approach included iron supplementation and dietary modifications aimed at increasing iron intake and enhancing its absorption. MNT played a crucial role in addressing the nutritional deficiencies associated with PVS, emphasizing the importance of a diet rich in heme iron, vitamin C and other nutrients that promote hematopoiesis. The patient’s condition improved significantly with a combination of medical treatment and nutritional support, highlighting the importance of a multidisciplinary approach in managing PVS. This case underscores the need for early diagnosis and the role of personalized MNT in improving patient outcomes in plummer-vinson syndrome.
Keywords
Plummer-Vinson syndrome; Glossitis; Medical nutrition therapy; Hematopoiesis
Introduction
A 31 year old newly married lady who was known to have been diagnosed with plummer vinson syndrome in August 2019, was detected to have iron deficiency anemia and an esophageal web occupying half of esophageal circumference [1]. She complained of progressively worsening dysphagia in March 2020 and a repeat endoscopy showed an ulceroproliferative friable growth in post cricoid region extending inferiorly into the cervical esophagus. Biopsy confirmed squamous cell carcinoma. CT-PET scan showed a large mass in the cervical esophagus and postcricoid region measuring 2.1 × 3.6 × 6 cms length compressing the trachea and abutting the internal carotid artery with volume of 46 cc and SUV MAX=26.1. There were enlarged necrotic lymph nodes on both sides neck which were metabolically active and appeared involved. There were no other FDG avid lesions seen elsewhere. We staged her to have a locally advanced post cricoid/ upper cervical esophagus cancer cT3 N2 Mo (stage IIIB) as per AJCC 8th edition [2].
She appears to be underweight (36 Kg) with ECOG PS=1 with frail physique but had no medical co-morbidities. She underwent definitve concomitant chemoradiation with 6 cycles of weekly chemotherapy with carboplatin and paclitaxel along with Intensity Modulated Radiotherapy Treatment (IMRT) to the primary and neck node regions to total dose of 58 Gy/29 #/6 weeks. She tolerated this treatment initially quite well and since we anticipated detriment in her borderline nutritional status, she was referred to dietician early in course of treatment for expert advice to increase weight as well to maintain good intensity of this diet treatment to achieve optimum outcomes and also had a nasogastric tube inserted early in course of her treatment [3].
Case Presentation
Nutrition care plan
Mode of feeding: Ryles tube feefing was planned: Proteins: 2.5 gm to 3 gm per kg bodyweight total protein 90 gm-100 gm was well tolerated by her calorie: 40-50 calories per kg bodyweight was advised and she has tolerated very well so gradually was added medium chain triglyceride powder/oil as per tolerance to increase calorie intake fat macro nutrient fat also 40 gm-50 gm patient was monitored every week for the compliance of diet. Nutrition supplement was also advised to fulfil additional requirement of macro as well as micro nutrients. Every month weight gain was 2.5 kg to 4 kg.
In addition, the consumption and requirements for micronutrients needs to be increased by the adverse effects of chemo-or radiotherapy (e.g., vomiting, diarrhea, alterations in taste and inflammatory processes). Loss of appetite and a version to particular foods as a result of anorexia also contribute to a micronutrient deficiency, was also taken care [4].
This lady was treated upto maximum tolerance and completed her treatment in May 2020. We continued with her diet plan for the next 6 weeks and repeat endoscopy was performed in July 2020 which showed onloy superficial ulceration with no evidence of disease. Up-to-date CT-PET scan imaging done in August 2020 showed complete metabolic response with no evidence of any residual disease. Her nasogastric tube was removed towards end of August and this lady will soon restart her job in IT company.
According to the European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines on enteral nutrition, it can be assumed that all patients with cancer who consume less than 60% of their daily energy requirements for more than 7-10 days have an inadequate supply of micronutrients malnutrition affects not only the macronutrients that supply energy (carbohydrates, proteins and fats) but also the biocatalytic and immunomodulating micronutrients. As macronutrients are the natural carriers of micronutrients, malnutrition is one of the main reasons that cancer patients have an inadequate micronutrient status [5]. An inadequate diet has detrimental effects on the immune status and tolerance of treatment, as well as on various organ and metabolic functions up to 50% of cancer patients suffer from a progressive atrophy of adipose tissue and skeletal muscle, called cachexia, resulting in weight loss, a reduced quality of life and a shortened survival time nutritional supplements are widely used among patients with cancer who perceive them to be anticancer and antitoxicity agents recent studies, however, have provided increasing evidence that treatment is tolerated better-with an increase in patient compliance and a lower rate of treatment discontinuations-when micronutrients, such as selenium, are added as appropriate to the patient’s medication. Nutritional supplementation tailored to an individual’s background diet, genetics, tumor histology and treatments may yield benefits in subsets of patients [6].
Micronutrient deficiencies have, basically, a negative effect on the course of malignant disease and the efficiency of treatment intended to destroy tumors, as it impairs immunocompetence, increases the risk of complications and impacts on the patient’s physical and mental quality of life.
Results and Discussion
The success of treatment and healing processes in people with cancer are greatly influenced by the nutritional status of the patient. This is particularly relevant in clinical practice since, depending on the nature, site and stage of the malignancy. Malnutrition affects not only the macronutrients that supply energy (carbohydrates, proteins and fats) but also the biocatalytic and immunomodulating micronutrients. As macronutrients are the natural carriers of micronutrients, malnutrition is one of the main reasons that cancer patients have an inadequate micronutrient status (Figure 1) [7].
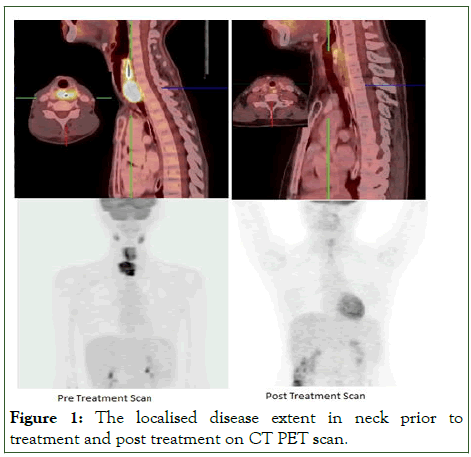
Figure 1: The localised disease extent in neck prior to treatment and post treatment on CT PET scan.
Micronutrient status in patients with cancer play very crucial role in fighting the disease even at the time of diagnosis and before there are any clinically-relevant changes in the nutritional status, but certainly after the start of treatment, the supply of various vitamins (e.g., vitamin D, vitamin C and B-group vitamins) and trace elements (e.g., selenium, zinc) is worse in patients with cancer than in healthy people.
Bleeding has also been reported in association with severe zinc deficiency in cancer patients with a poor nutritional status (Figure 2) [8].
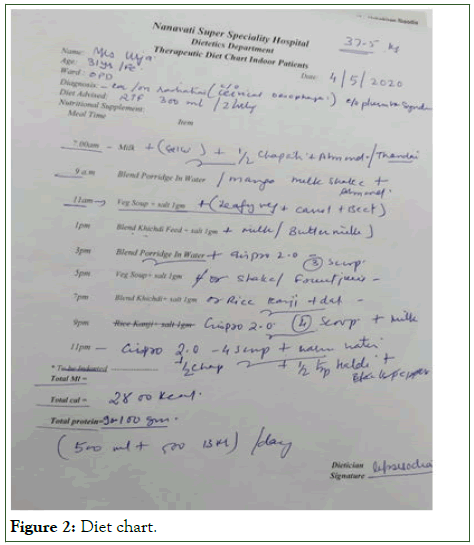
Figure 2: Diet chart.
Conclusion
This case study on Plummer-Vinson Syndrome (PVS) highlights the critical role of Medical Nutrition Therapy (MNT) in managing and improving patient outcomes. PVS, characterized by iron deficiency anemia, dysphagia and esophageal webs, is a condition that requires a multidisciplinary approach for effective treatment.
MNT is crucial in addressing the iron deficiency that underlies PVS. By providing a diet rich in iron, along with the appropriate supplementation, it is possible to correct the anemia and alleviate symptoms such as fatigue and difficulty swallowing. This, in turn, can improve the patient's overall nutritional status and quality of life.
Moreover, MNT also involves the management of dysphagia through texture-modified diets, ensuring that patients can meet their nutritional needs without exacerbating symptoms. Regular monitoring and adjustments in dietary interventions are essential to adapt to the changing needs of the patient.
References
- Sieja K, Talerczyk M. Selenium as an element in the treatment of ovarian cancer in women receiving chemotherapy. Gynecol Oncol. 2004;93(2):320-327.
[Crossref] [Google Scholar] [PubMed]
- Jaakkola K, Lahteenmaki P, Laakso J, Harju E, Tykka H, Mahlberg K. Treatment with antioxidant and other nutrients in combination with chemotherapy and irradiation in patients with small-cell lung cancer. Anticancer Res. 1992;12(3):599-606.
[Google Scholar] [PubMed]
- Stefanini M. Cutaneous bleeding related to zinc deficiency in two cases of advanced cancer. Interdis Int J Am Cancer Soc. 1999;86(5):866-870.
- Barker LA, Gout BS, Crowe TC. Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8(2):514-527.
[Crossref] [Google Scholar] [PubMed]
- Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, et al. Prognostic effect of weight loss prior tochemotherapy in cancer patients. Am J Med. 1980;69(4):491-497.
[Crossref] [Google Scholar] [PubMed]
- Strohle A, Zanker K, Hahn A. Nutrition in oncology: The case of micronutrients. Oncol Rep. 2010;24(4):815-828.
[Crossref] [Google Scholar] [PubMed]
- Zirpoli GR, Brennan PM, Hong CC, McCann SE, Ciupak G, Davis W, et al. Supplement use during an intergroup clinical trial for breast cancer (S0221). Breast Cancer Res Treat. 2013;137:903-913.
[Crossref] [Google Scholar] [PubMed]
- Micke O, Bruns F, Glatzel M, Schonekaes K, Micke P, Mucke R, et al. Predictive factors for the use of Complementary and Alternative Medicine (CAM) in radiation oncology. Eu J Int Med. 2009;1(1):19-25.
Citation: Sisodia U, Malde R, Chauhan B (2024) A Case Study on Plummer Vinson Syndrome and MNT. J Nutr Disord Ther. 14:299.
Copyright: © 2024 Sisodia U, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

