Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
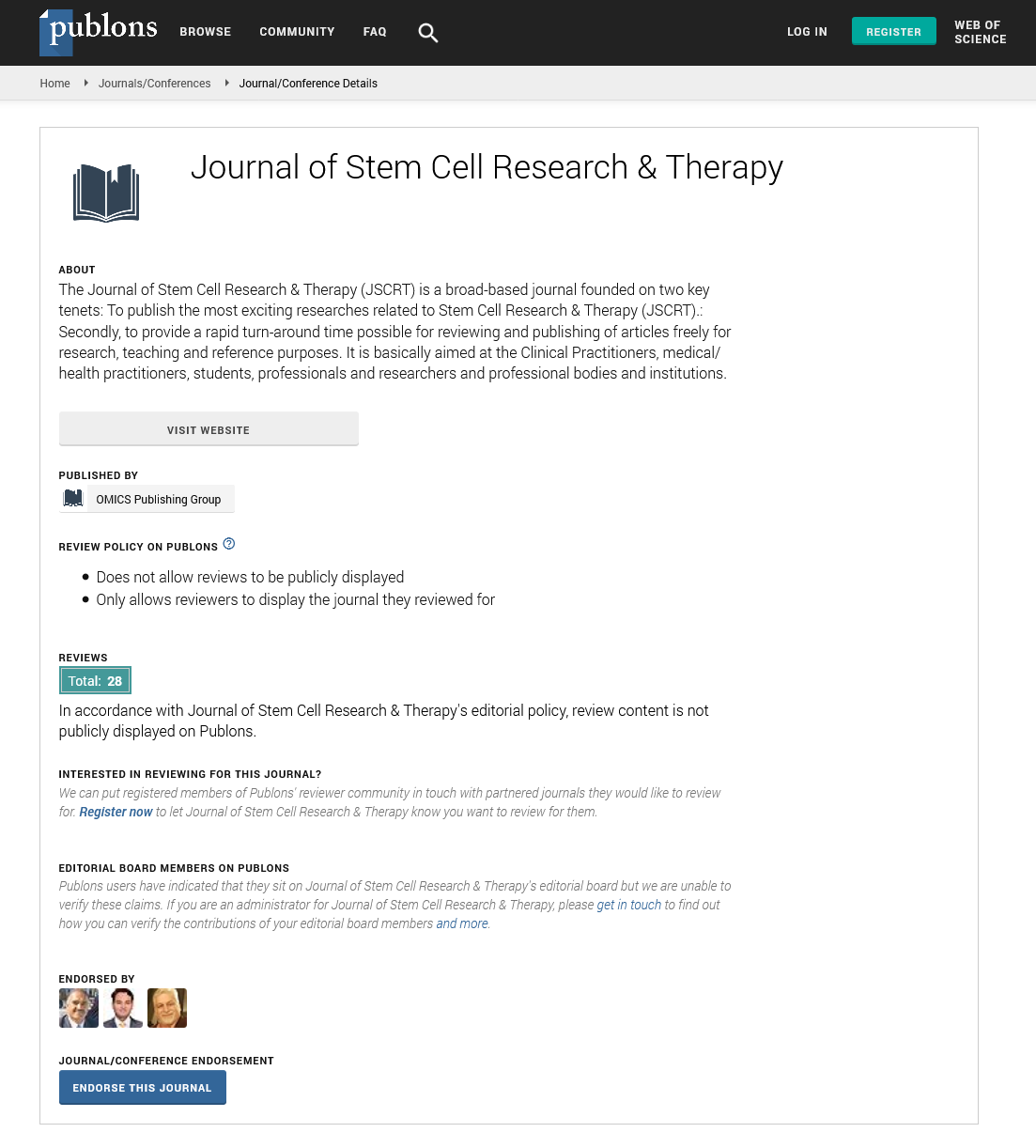
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 13, Issue 2
A Case Report: The First Show Phenomenon in the Treatment of Spinal Cord Injury with Regentime Procedure using Autologous Bone Marrow Derived Stem Cells
Rita T. Boulos1, Vanessa J. Mansour2, Lea I. Nemer3, Cynthia F. Najjoum4, Elsa A. Asmar5 and Nassim H. Abi Chahine6*2Department of Infectious Disease, ACE Cells Lab Ltd, Rotherham, United Kingdom
3Department of Molecular Biology, ACE Cells Lab Ltd, Rotherham, United Kingdom
4Department of Immunology, ACE Cells Lab Ltd, Rotherham, United Kingdom
5Department of Genomics and Proteomics, ACE Cells Lab Ltd, Rotherham, United Kingdom
6Department of Neurological Surgeon, ACE Cells Lab Ltd, Rotherham, United Kingdom
Received: 23-Sep-2022, Manuscript No. JSCRT-22-18158; Editor assigned: 27-Sep-2022, Pre QC No. JSCRT-22-18158 (PQ); Reviewed: 11-Oct-2022, QC No. JSCRT-22-18158; Revised: 27-Jan-2023, Manuscript No. JSCRT-22-18158 (R); Published: 03-Feb-2023, DOI: 10.35248/2157-7633.23.13.577
Abstract
This case report demonstrates ‘the first show phenomenon’ following regentime stem cell therapy applied to a spinal cord injury patient. A 40 years old gentleman sustained a ballistic injury at the level of T9, resulting in complete bilateral motor and sensory loss from T9 and below. He was treated with autologous bone marrow derived mononuclear stem cells injected into his spinal canal 2.5 years after his injury. Follow up during the first week post transplantation showed early symptom improvement termed “the first show post phenomenon”. He regained sensation to light touch in his lower limbs by the end of week 1 and reported no serious implications or complications.
Keywords
Spinal cord injury; Regentime therapy; Stem cell therapy; First show phenomenon; Autologous bone marrow derived mononuclear stem cells
INTRODUCTION
Spinal Cord Injury (SCI) is a critical health condition that can result in substantial morbidity and long term disability. The disruption of the electrical influx running through the spinal cord leads to sensory motor loss of function below the injury level [1]. The leading causes of SCI include motor vehicle accidents, violence (especially gunshot wounds), sports accidents, and falls among others [2]. The pathophysiology of SCI consists of primary and secondary phases of injury. The primary phase relates to the early stage immediately after the injury and includes neural parenchyma destruction, axonal network disruption, glial membrane disruption, and hemorrhage. The secondary phase follows and is manifested by early vascular damage, free radical formation, inflammation, necrosis, neuronal apoptosis, wallerian degeneration, axonal demyelination and remodeling, and late glial scar formation and maturation [3].
Despite significant advances in new therapeutic and rehabilitation approaches, there is no treatment for SCI yet. However, several clinical trials were conducted to assess the long term therapeutic efficacy of bone marrow derived stem cell transplantation on SCI patients and found promising results [4,5]. We report the case of a 40 years old gentleman with a past medical history of SCI at the level of T9 two and a half years ago, with an American Spinal Injury Association (ASIA) impairment scale grade A, who underwent the regentime procedure [6]. The patient gained lower limb sensation and improved to ASIA impairment scale grade B as early as one week post stem cell transplantation, a manifestation that we call ‘the first show phenomenon’. The major focus of this case report is the role of Regentime therapy in optimizing neuro regeneration by administering autologous Bone Marrow derived Mononuclear Cells (BM-MNCs).
Case Presentation
A 40 years old man was presented to our hospital outpatient clinic for a SCI stem cell treatment trial. He had a 2.5 year history of a ballistic injury that resulted in a spinal cord thoracic lesion at the level of T9, for which he underwent posterior decompression and fusion after 24 hours (Figure 1). The patient presented with paralysis, loss of sensation in the lower extremities, and loss of bladder and bowel control since the injury. On physical examination, he had a bilateral loss of sensation (pain, temperature, touch, vibration, and proprioception) below the level of injury and a motor power of 0/5 in his lower limbs.

Figure 1: The thoracic injury at the level of T9.
The patient decided to attempt the regentime procedure. Before therapy, written consent was obtained from the patient, and a day by day follow up was done during the first weeks. A periodic 1 month follow up was scheduled for later assessment of safety and improvement.
The regentime procedure
Pre-lab stage: During the first 2 days, the patient was injected with a total of 4 doses of 300 mcg of granulocyte colony stimulating factor intramuscularly separated by 12 hours each. Eight hours after the last dose, an increase in the white blood cell count was registered 28000 cells/mL.
The bone marrow collection stage: Bone marrow aspiration was done, in which 100 mL were collected from each posterior superior iliac crest, using 4 aspiration syringes filled with 25,000 units of 10% heparin sodium each. The aspirate was transferred to a transfusion bag after the removal of sodium citrate under sterile conditions. The bag was held at 22°C on a slow three dimensional laboratory shaker.
Laboratory stage: The cellular buffy coat containing stem cells was collected after centrifugation.
Transplantation stage: After 24 hours of incubation, the patient received progenitor stem cells via direct injection in the operating room after the hardware removal. Following the surgery, the patient also had an intravenous administration of around 100 million stem cells (1 mL) in 100 mL of normal saline solution.
Post-transplantation stage: The patient stayed in his hospital room for several days to monitor vital signs and record any undesirable effects.
Results
Postoperatively, the patient was recovering smoothly with no significant complaints. He started to regain sensation in his right lower limb upon touch on day 1 after stem cell transplantation. Towards the end of the first week, he was able to detect touch in both of his lower limbs. However, two to three weeks after transplantation, the early improvements declined. Moreover, he could not distinguish between two points applied simultaneously to his legs bilaterally, did not feel changes of temperature applied on his lower limbs, and maintained an absent joint position sense bilaterally.
Discussion
Every year, around 1 million persons suffer from SCI, causing significant morbidity and permanent motor, sensory, and autonomic dysfunction [7]. Stem cell therapy for SCI success rate depends on when the injury first occurred and on its grade due to the heterogeneity of SCI pathophysiology. Our patient sustained a SCI that resulted in a total bilateral loss of sensory and motor function below the injury level. He underwent the regentime procedure via both direct injections in the operating room and intravenous routes 2.5 years after injury. Regentime therapy first show phenomenon was evident during the first days post transplantation when the patient regained sensation to touch in his lower limbs. However, this phenomenon has shown to be transient few weeks post transplantation. Noting that he did not complain of any undesirable effects during this follow up period. Our results suggest that the regentime procedure seems to be safe and effective for patients suffering from SCI.
The first cells utilized for treating SCI in both experimental and clinical trials were Bone Marrow derived Mesenchymal Stem Cells (BM-MSCs) [8]. Motor, sensory, and autonomic functions were partially improved in primary studies involving thoracic spinal cord contusion and BM-MSCs transplantation. Similar improvements were recorded in other studies whether BM-MSCs were given via direct injection into the spinal canal during a surgical act intrathecally or intravenously. Also, stem cell treatment was shown to result in improvement in the ASIA score and recovery of motor evoked potentials and somatosensory evoked potentials in a trial conducted on 20 adults with chronic SCI. Autologous stem cell therapy administered intrathecally was shown to participate in neuro restoration via several pathways as suggested by the non-identical effects recorded on different neurophysiological tests concerning safety, phases I/II clinical trials using autologous BM-MSCs in patients with acute, sub-acute, and chronic SCI showed no long term side effects and seemed to be safe [9-13].
SCI can be caused by various conditions, possibly resulting in permanent impairment. On the other hand, MSCs and their associated cellular products are readily available therapeutic tools for regenerative medicine, including central nervous system diseases and conditions. The ability of autologous BMMSCs to release a range of antiapoptotic, neurotrophic, and anti-inflammatory molecules is thought to be the cause of their therapeutic effects. These cells can differentiate into neural cells, express neuronal markers, and secrete neuroprotective growth factors that play a key role in neural restoration and regeneration such as glia derived, brain derived, nerve, and ciliary neurotrophic growth factors, and neurotropin-3. On the other hand, cavitation prompted by tissue necrosis, axonal degeneration, and neural cell death is frequently present with damaged neural tissue. This invariably produces scars, which are made up of inflammatory immune cells, fibroblasts, Extra Cellular Matrix (ECM) deposits, and astrocytes. MSCs exhibit anti-inflammatory, anti-apoptotic, and ECM modulatory properties, leading to neural rejuvenation [14]. All these properties suggest that MSCs can be beneficial for spinal cord repair and have provided an outline of strategies that scientists are taking toward rejuvenation and restoration.
This case report shows promising improvement of SCI symptoms in our patient. The regentime therapy first show phenomenon was manifested through the patient’s early regain of sensation to touch progressively during the first week following therapy. However, a longer follow up duration is yet to be undergone for further assessment of improvement and any undesirable effects related to stem cell therapy.
Conclusion
SCI is a serious public health problem with a high morbidity rate. Stem cell transplantation for SCI treatment has been conducted in several studies showing promising results. Regentime therapy involves administering autologous BMMNCs to a target population. The administration of this therapy to our SCI patient demonstrated the ‘first show phenomenon’ where he had improved symptoms as early as during the first few days after therapy.
References
- Devivo MJ. Epidemiology of traumatic spinal cord injury: Trends and future implications. Spinal Cord. 2012;50(5):365-372.
- Anjum A, Yazid MD, Fauzi Daud M, Idris J, Ismail O, NaickerAS, et al. Spinal Cord Injury: Pathophysiology, Multimolecular Interactions, and Underlying Recovery Mechanisms. Int J Mol Sci. 2020;21(20):7533.
- Honmou O, Yamashita T, Morita T, Oshigiri T, Hirota R, Iyama S, et al. Intravenous infusion of auto serum-expanded autologous mesenchymal stem cells in spinal cord injury patients: 13 case series. Clin Neurol Neurosurg. 2021;203:106565.
- Sykova E, Jendelova P, Urdzikova L, Lesny P, Hejcl A. Bone marrow stem cells and polymer hydrogels–two strategies for spinal cord injury repair. Cell Mol Neurobiol. 2006;26(7-8):1113–1129.
- Boulos RT, Nemer LI, Mansour VJ, Abi Chahine NH. Treatment of a Chronic Obstructive Pulmonary Disease Case with Regentime Procedure. EPRA-IJRD. 2022;7(7):57-60.
- James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):56–87.
- Sykova E, Homola A, Mazanec R, Lachmann H, Kobylka P, Kobylka P, et al. Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant. 2006;15(8-9):675–687.
- Nandoe RDS, Hurtado A, Levi ADO, Grotenhuis A, Oudega M. Bone marrow stromal cells for repair of the spinal cord: Towards clinical application. Cell Transplant. 2006;15(7):563–577.
- Cizkova D, Novotna I, Slovinska L, Vanicky I, Jergova S, Rosocha J, et al. Repetitive intrathecal catheter delivery of bone marrow mesenchymal stromal cells improves functional recovery in a rat model of contusive spinal cord injury. J Neurotrauma. 2011;28(9):1951-1961.
- Osaka M, Honmou O, Murakami T, Nonaka T, Houkin K, Hamada H, et al. Intravenous administration of mesenchymal stem cells derived from bone marrow after contusive spinal cord injury improves functional outcomes. Brain Res. 2010;1343:226-235.
- Frolov AA, Bryukhovetskiy AS. Effects of hematopoietic autologous stem cell transplantation to the chronically injured human spinal cord evaluated by motor and somatosensory evoked potentials methods. Cell Transplant. 2012;21(Suppl 1):49–55.
- Sykova E, Cizkova D, Kubinova S. Mesenchymal Stem Cells in Treatment of Spinal Cord Injury and Amyotrophic Lateral Sclerosis. Front Cell Dev Biol. 2021;9:695900.
- Ullah I, Subbarao RB, RhoGJ. Human mesenchymal stem cells-Current trends and future prospective. Biosci Rep. 2015;35(2): 00191.
- Marconi S, Castiglione G, Turano E, Bissolotti G, Angiari S, Farinazz A, et al. Human adipose derived Mesenchymal Stem Cells systemically injected promote peripheral nerve regeneration in the mouse model of sciatic crush. Tissue Eng Part A. 2012;18(11-12):1264-1272.
Citation: Boulos RT, Mansour VJ, Nemer LI, Najjoum CF, Asmar EA, Chahine NHA (2023) A Case Report: The First Show Phenomenon in the Treatment of Spinal Cord Injury with Regentime Procedure Using Autologous Bone Marrow Derived Stem Cells. J Stem Cell Res Ther. 13:577.
Copyright: © 2023 Boulos RT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.