Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 5, Issue 6
A Case Report of Malrotation with LADD’s Band Accompanying Intrinsic Duodenal Stenosis in Middle Aged Children
Raba’a Alghalayini1*, Bana Sabbagh1, Mazen Almoubarak1, Mohammad Kheir Diab1 and Lina Khouri22Department of Pediatrics, University of Damascus, Damascus, Syrian Arab Republic
Received: 22-Oct-2021 Published: 12-Nov-2021
Abstract
Malrotation is a congenital anomaly that mainly manifests in newborns, it usually presents with bowel obstruction secondary to LADD’s band and rarely presents with chronic abdominal discomfort. We present a case of an 11 year old girl who was diagnosed after exploratory laparotomy with midgut malrotation accompanying intrinsic duodenal stenosis.
Keywords
Bilious vomiting; Intestinal obstruction; Ladd’s Procedure; Midgut malrotation; Duodenal stenosis care
Introduction
Rotational anomalies are one of the most frequent of embryonic malformations related to the digestive tract. The incidence of malrotation is ~1:500 births and the symptomatic incidence is 1:6000 [1,2]. Intestinal malrotation refers to incomplete midgut rotation and fixation in early fetal life and can consist of complete absence of rotation, incomplete rotation-less than 270-or inverse rotation. In most cases malrotation can present with other congenital anomalies and it is typically diagnosed during the first year. We report a rare case of malrotation with LADD’s band presenting in an 11 year old girl accompanying intrinsic duodenal stenosis and annual stenosis.
Case Study
An 11-year-old-girl presented to the hospital with the chief complaints of abdominal pain, epigastric fullness, bilious vomiting, severe constipation and prolonged fatigue for 15 days. The abdominal pain was epigastric continuous discomfort with repeated colicky attacks and tends to ease after vomiting. Oral feeding cause bilious vomiting 10 to 15 times a day leading to anorexia. She was born through normal full term vaginal delivery with no complications except chronic constipation since birth diagnosed as anal stenosis and treated surgically causing normal defecating. She was diagnosed with pancreatitis two years ago and afterwards, she didn’t suffer any symptoms, normal appetite with preference small quantities of food specially yoghurt, normal motor skill development without gaining any weight. On physical examination, the patient was conscious; her vital signs were pulse 90, blood pressure 100/60, temperature 1010 F, and respirations 16. There were severe cachexia, fatigue, paleness, dehydration, generalized muscle atrophy, chest malformation, webbed neck, thoracic kyphosis, and scaphoid soft abdomen. On Per abdomen examination there was Mild tenderness around the umbilicus. The intestinal sounds were Low but hearable. Her rectal examination was normal. There was evidence of free fluid in the peritoneal cavity.
Results and Discussion
Malrotation is a congenital anomaly referring to either lack of or incomplete rotation of the fetal intestines around the axis of the superior mesenteric artery during fetal development. It is typically diagnosed in the first few months of life, and 90% of cases are diagnosed during the first year [3-5].
Our patient is diagnosed lately in age of 11 years. Although malrotation presents usually with bowel obstruction secondary to Ladd’s band or volvulus, many may live without any complaint, and the anomaly is discovered only at autopsy and some may present with chronic and unexplained abdominal discomfort, and even fewer may report acute episodes of agonizing abdominal pain, in our case the patient had chronic epigastric pain after each meal, bilious vomiting, lack of appetite with weight loss and tendency to certain food like yoghurt. Plain X-ray is often the first step in the imaging evaluation of pediatric patients with suspected malrotation, the classic “double bubble” sign of duodenal obstruction (dilated stomach and duodenum) was seen with lack of bowel gas distal to the duodenum (Figure 1) [6]. This findings are concerning enough to prompt the surgeon to consider operative exploration. Abdominal MRI was performed 2 months previously during a visit to another center was again reviewed, severe gastric distention with no evidence of small or large bowel dilation, duodenal wrap or narrowing of aortic- mesenteric window (Figure 2). After stabilizing the fluid and electrolyte imbalance, the surgery was performed. Exploratory laparotomy showed extended stomach and first two parts of the duodenum, free cecum in the upper part of the abdomen, malrotation with Ladd’s band extending from the colon to the liver pressing the second part of the duodenum. The bands were cut freeing the duodenum. Interior duodenal stenosis also was found so Duodenoduodenostomy (diamond) was performed with Ladd’s procedure after Gastro-jejunostomy (Omega) was made. From 30 to 60% of patients with malrotation or malfixation can have other associated congenital anomalies, either inside or outside the abdominal cavity [7]. Our patient was also diagnosed with duodenal stenosis and anal stenosis. Anal stenosis caused her constipation early in life and was fixed with surgery. We are not sure whether the duodenal stenosis or the malrotation with Ladd’s band or both of them were the main cause of the symptoms. A study suggests that the diagnosis of duodenal stenosis may be delayed because these infants are able to tolerate small feedings due to the incomplete nature of obstruction [8]. Postoperatively, the girl recovered well, and liquid oral feeds were started 6 days after surgery. The child was discharged 20 days after surgery and is thriving well at a follow-up of 4 months. In our case, we report a rare association between intrinsic and extrinsic stenosis of the duodenum in an 11-year-old girl due to the contemporary presence of Ladd’s band and incomplete web. Patients who have malrotation without symptoms or with chronic symptoms are in danger of developing intestinal obstruction, with or without intestinal ischemia at any moment. A previous review of nine cases of intestinal malrotation reported eight cases had symptoms of intermittent abdominal pain for long duration, with or without vomiting before the production of a volvulus, obstruction, or other serious complication.
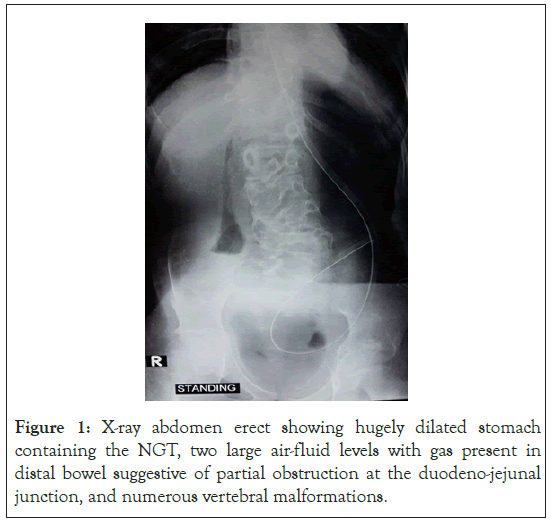
Figure 1: X-ray abdomen erect showing hugely dilated stomach containing the NGT, two large air-fluid levels with gas present in distal bowel suggestive of partial obstruction at the duodeno-jejunal junction, and numerous vertebral malformations.
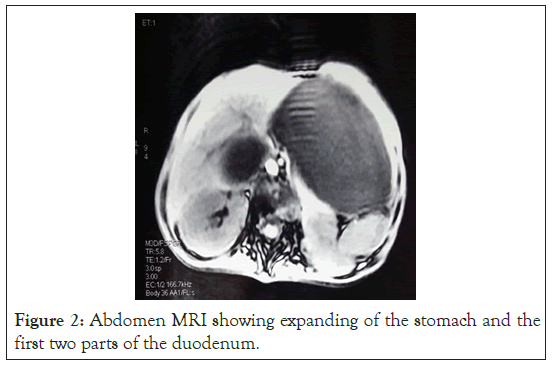
Figure 2: Abdomen MRI showing expanding of the stomach and the first two parts of the duodenum.
Conclusion
We report this case due to its rarity and varied delayed mode of presentation in order to propose making duodenal stenosis and malrotation an important differential diagnosis in the mind of surgeons tackling intestinal obstruction-like symptoms in middle aged children. Negligent diagnosis of such cases leads to undesirable consequences.
Conflicts of Interest
No.
Funding Statement
None.
Acknowledgements
None.
REFERENCES
- Ingoe R, P Lange. The Ladd's procedure for correction of intestinal malrotation with volvulus in children. AORN J. 2007; 85(2): 300-308.
- Williams H. Green for danger! Intestinal malrotation and volvulus. Arch Dis Child Educ Pract Ed. 2007; 92(3): 87-91.
- Zissin R, Rathaus V, Oscadchy A, Kots E, Gayer G, Shapiro FM. Intestinal malrotation as an incidental finding on CT in adults. Abdom Imaging. 1999; 24(6): 550-555.
- Wang CA, Welch CE. Anomalies of intestinal rotation in adolescents and adults. Surgery. 1963; 54: 839-855.
- Flue MV, Herzog U, Ackermann C, Tondelli P, and Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum. 1994; 37(2): 192-198.
- Tackett JJ, Muise ED, Cowles RA. Malrotation: Current strategies navigating the radiologic diagnosis of a surgical emergency. World J Radiol. 2014; 6(9): 730-736.
- Warner BW. Malrotation. In: Oldham KT, Colombani PM, Foglia RP (eds) Surgery of infants and children: scientific principles and practice: Lippincott-Raven, Philadelphia. BJS. 2005; 84(8): 1181-1181.
- Kshirsagar AY. Duodenal stenosis in a child. Afr J Paediatr Surg. 2011; 8(1): 92-94.
Citation: Alghalayini R, Sabbagh B, Almoubarak M, Diab MK, Khouri L (2021) A Case Report of Malrotation with LADD's Band Accompanying Intrinsic Duodenal Stenosis in Middle Aged Children. J Surg Anesth. 5:160.
Copyright: © 2021 Alghalayini R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
