Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 10, Issue 3
A case of uterine adenomyosis that led to the rapid development of blood coagulation disorder two days after an induced abortion
Nishimoto M1, Fujioka T2*, Saito M1, Saito S1, Kurakata M1, Sugawara J1, Yaegashi N1 and Sugiyama T22Department of Obstetrics and Gynecology, Ehime University Graduate School of Medicine, Shitsukawa, Toon City, Ehime, Japan
Received: 04-May-2019 Published: 27-May-2019
Abstract
Cases of uterine adenomyosis in which disseminated intravascular coagulation is rapidly induced by infection, surgery, fertility treatment, abortion, or delivery are occasionally reported, but little is known about these conditions. We encountered a case of uterine adenomyosis in which the patient developed a rapid blood coagulation disorder 2 days after curettage for a missed abortion. A 39-year-old Japanese woman visited a private clinic with secondary amenorrhea, and was found to be 11 weeks pregnant. Three days later, she was diagnosed with missed abortion, and was transferred to our hospital with severe abdominal pain the day after the curettage. She complained of lower abdominal pain and pains from the hips to both lower extremities. Transvaginal ultrasonography revealed a diffuse uterine adenomyosis in the posterior uterine wall, and no remaining fetal tissue was visible in the uterine cavity. Laboratory findings at admission showed only mild elevation of WBC count, however, D-dimer and fibrin degradation product levels were abnormally high. After hospitalization the symptoms improved with nonsteroidal anti-inflammatory drugs, and the laboratory findings obtained the next day revealed a marked blood coagulation disorder, deteriorating renal function, decreased platelet count, and increased Lactate Dehydrogenase (LDH) concentration. No apparent thrombosis was observed on CT, and MRI revealed diffuse uterine adenomyosis in the posterior uterine wall with an irregular high intensity area. She was diagnosed with microthrombosis in uterine adenomyosis, and a total hysterectomy was performed. Surgical findings showed mild endometriosis adhesion in the dorsal uterus. Villous components were confirmed in the uterine cavity. Histopathology showed diffuse hemorrhage in the interstitium of the uterine adenomyosis and fibrin thrombus formation. The patient was diagnosed with intratumoral thrombosis caused by uterine adenomyosis. The patient’s blood coagulation disorder and deteriorating renal function improved gradually after surgery. The patient made steady progress, and was discharged 10 days after surgery.
Keywords
Uterine adenomyosis; Endometrial curettage; Abortion; DIC
Introduction
It is well known that Disseminated Intravascular Coagulation (DIC) rapidly exacerbates systemic conditions and is associated with a poor prognosis. We encountered a case of uterine adenomyosis that developed a rapid and marked blood coagulation disorder 2 days after curettage for a missed abortion, despite the patient’s overall good condition. This case had a favorable outcome. Herein, we report this case and include a discussion of the relevant literature.
Case Presentation
A 39-year-old Japanese woman (G2P2) visited a private clinic, presenting with secondary amenorrhea for 11 weeks. She had no remarkable family or medical history. Upon examination, she was found to be 11 weeks pregnant. Three days later, she visited the private clinic again because she was experiencing lower abdominal pain with vaginal bleeding, and she was diagnosed as having a missed abortion. At that time, curettage was performed. The day after the curettage, her lower abdominal pain increased and the symptoms were not resolved. Finally, she was transferred to our hospital with severe abdominal pain. At the time of admission to our hospital, the patient was fully conscious. Her heart rate was 80 bpm, blood pressure was 155/89 mmHg, and body temperature was 37.90°C. Her subjective symptoms included lower abdominal pain and pains from the hips to both lower extremities. Transvaginal ultrasonography revealed an enlarged uterus, approximately 11 cm in diameter, and diffuses uterine adenomyosis in the posterior uterine wall. No remaining fetal tissue was visible in the uterine cavity, and the bilateral adnexa were normal. Laboratory findings at admission showed only mild elevation of WBC count that could be expected post curettage. However, D-dimer and fibrin degradation product levels were abnormally high (Table 1).
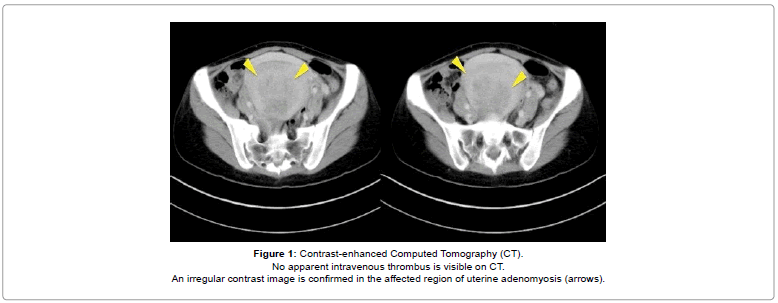
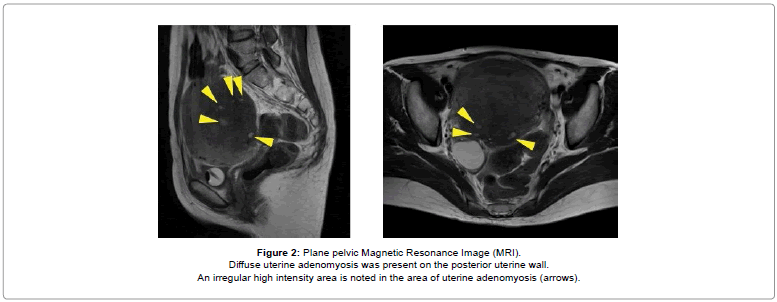
After hospitalization, the symptoms improved with nonsteroidal anti-inflammatory drugs; however, the laboratory findings obtained the next day (2 days after curettage by the previous clinic) revealed a marked blood coagulation disorder, deteriorating renal function, decreased platelet count, and increased Lactate Dehydrogenase (LDH) concentration compared to those observed the day before (Table 1). These data did not change upon reexamination. No apparent thrombosis was visible on contrast-enhanced computed tomography. Irregular contrast image was observed in the affected region of uterine adenomyosis (Figure 1). Plain pelvic magnetic resonance imaging (selected because of the patient’s deteriorating renal function) revealed diffuse uterine adenomyosis in the posterior uterine wall and an irregular high intensity area in the area of uterine adenomyosis (Figure 2).
| At the time of hospitalization | 8 hours after hospitalization (before operation) | Postoperative 3 hours | Postoperative 1 day | Postoperative 5 days | |
|---|---|---|---|---|---|
| WBC (×102/µL) | 134 | 153 | 115 | 83 | 83 |
| Hb (g/dL) | 11 | 10.8 | 9.1 | 8.5 | 8.9 |
| Plt (×104/µL) | 235 | 104 | 123 | 137 | 316 |
| LDH (IU/L) | 177 | 332 | 267 | ||
| Cre (mg/dL) | 0.43 | 0.96 | 0.85 | 0.72 | 0.46 |
| CRP (mg/dL) | 1.8 | 3.2 | 9.6 | 12.4 | 2.1 |
| FBG (mg/dL) | 394 | 57 | 211 | 313 | 388 |
| FDP (µg/mL) | 83 | <1200 | 375 | 119 | 6.8 |
| D-dimer (µg/mL) | 124.6 | <300 | 126.4 | 22.9 | 2.3 |
| CA125 (IU/mL) | 1514 | 212 |
Table 1: Laboratory findings.
No apparent intravenous thrombus is visible on CT.
An irregular contrast image is confirmed in the affected region of uterine adenomyosis (arrows).
Figure 1: Contrast-enhanced Computed Tomography (CT).
Diffuse uterine adenomyosis was present on the posterior uterine wall.
An irregular high intensity area is noted in the area of uterine adenomyosis (arrows).
Figure 2: Plane pelvic Magnetic Resonance Image (MRI).
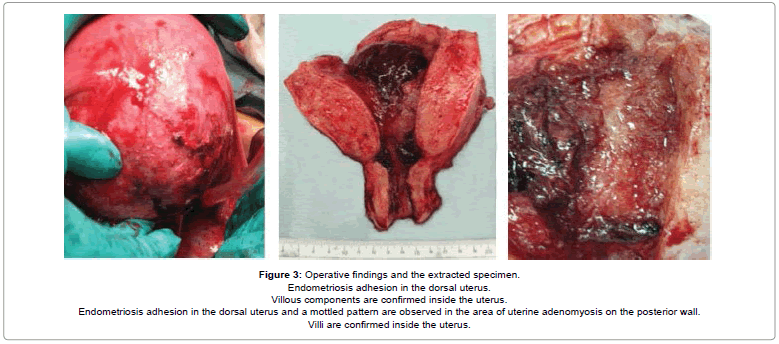
The patient’s clinical course and laboratory data were consistent with a diagnosis of microthrombosis in uterine adenomyosis and acute renal failure. A total hysterectomy was performed immediately after obtaining informed consent from the patient and her husband. She received six units of fresh frozen plasma. Surgical findings showed mild endometriosis adhesion in the dorsal uterus. Villous components were confirmed inside the operatively extracted specimen (Figure 3). The surgery itself was completed without serious complications. Operating time was 93 min, and the intraoperative blooding volume was 328 g.
Endometriosis adhesion in the dorsal uterus.
Villous components are confirmed inside the uterus.
Endometriosis adhesion in the dorsal uterus and a mottled pattern are observed in the area of uterine adenomyosis on the posterior wall.
Villi are confirmed inside the uterus.
Figure 3: Operative findings and the extracted specimen.
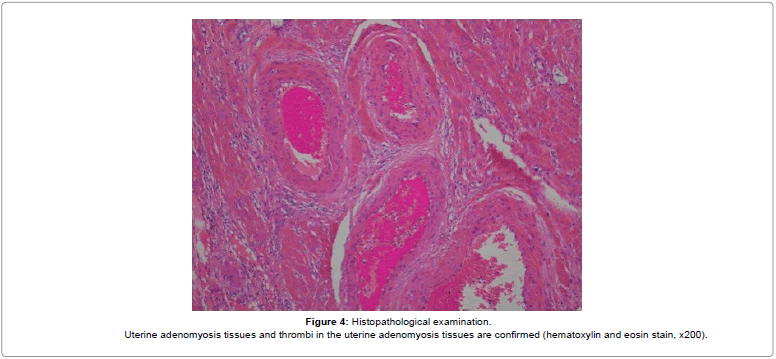
The patient’s blood coagulation disorder and deteriorating renal function improved gradually after surgery (Table 1). The patient made steady progress and was discharged 10 days after surgery. Histopathology showed diffuse hemorrhage in the interstitium of the uterine adenomyosis and fibrin thrombus formation (Figure 4). The patient was diagnosed with intra-tumoral thrombosis caused by uterine adenomyosis.
Uterine adenomyosis tissues and thrombi in the uterine adenomyosis tissues are confirmed (hematoxylin and eosin stain, x200).
Figure 4: Histopathological examination.
Discussion
Uterine adenomyosis was previously considered endometriosis internal, but the disease is now described as a condition in which the endometrium diffusely infiltrates the myometrium, and is not treated as an endometriosis [1]. A few cases of DIC associated with uterine adenomyosis have been reported. Some of these were related to pregnancy [2] and others were not (e.g., menses and treatment with ovulation-inducing agents) [3,4]. One mechanism of DIC development includes intrauterine infections that can lead to systemic inflammatory response syndrome and sepsis. A second mechanism suggests that DIC may be induced by a sequential process that begins with the induction of local thrombosis by intramyometrial bleeding from the ectopic endometrium or bleeding from abortion-associated decidualike tissues or congestion, followed by the development of myometrial ischemia, and finally a large release of tissue factor [4]. By a third mechanism, high hormone levels appear to be involved in tissue factor release in adenomyosis [5]. Supporting these theories, the tissue factor concentration in the endometrium is higher in adenomyosis than in immuno-histologically normal endometrium [6]. A further mechanism reported for DIC development is that cell disruption due to myometrium necrosis tends to cause increased levels of LDH 4 and 5, and this suggests that these markers could be used as an index of the condition [3]. The serum CA125 concentrations in our case were abnormally high (>1000 units/mL), although the cause is unknown, and this marker might be used as an index if DIC is suspected.
Notably, when uterine adenomyosis was induced by pregnancy, in this case and others, conservative, non-surgical treatment became difficult and prolonged, and ultimately resulted in a hysterectomy in all cases. In some cases of uterine adenomyosis without pregnancy, conservative treatment was associated with the need for dialysis due to progression of renal failure. Although uterine conservation should be considered for patients who desire to have children, the likelihood of systemic conditions worsening if a hysterectomy is not promptly performed should also be considered. Because the patient’s overall condition was quite good in this case, uterus conservation was examined as an alternative therapeutic strategy. However, the outcome of uterus conservation may be poor, and the patient’s thorough understanding of the treatment options allowed a prompt intervention. Therefore, we could treat her without any increase in disease severity. On the day after admission, mild elevation of WBC, thrombosis and a bloodcoagulation disorder were observed. The diagnosis of thrombosis was unexpected; thus, we note that the physician should be attentive to the possibility of these complications at all times.
Conclusion
In conclusion, we have presented a case of uterine adenomyosis after an induced abortion that involved the rapid development of a serious blood coagulation disorder. In the case of uterine adenomyosis, DIC may rapidly arise from various causes and may increase the severity of the disease. When DIC develops, prompt diagnosis and appropriate intervention can greatly affect the outcome.
Conflict of Interest
The authors have no conflict of interests to disclose.
REFERENCES
- Bird CC, McElin TW, Manalo-Estrella P. The elusive adenomyosis of the uterus-revisited. Am J Obstet Gynecol. 1972;112:583-593.
- Zhang J, Xiao X, Luo F, Shi G, He Y, Yao Y, et al. Acute disseminated intravascular coagulation developed after dilation and curettage in an adenomyosis patient: a case report. Blood Coagul Fibrinolysis. 2013;24:771-773.
- Nakamura Y, Kawamura N, Ishiko O, Ogita S. Acute disseminated intravascular coagulation developed during menstruation in an adenomyosis patient. Arch Gynecol Obstet. 2002;267:110-112.
- Son J, Lee DW, Seong EY, Song SH, Lee SB, Choi JR, et al. Acute kidney injury due to menstruation-related disseminated intravascular coagulation in an adenomyosis patient : A case report. Nephrology 2010;25:1372-1374.
- Lockwood CJ, Nemerson Y, Krikun G, Hausknecht V, Markiewicz L, Alvarez M, et al. Steroid-modulated stromal cell tissue factor expression : A model for the regulation of endometrial hemostasis and menstruation. JCEM 1993;77:1014-1019.
- Liu X, Nie J, Guo SW. Elevated immunoreactivity to tissue factor and its association with dysmenorrhea severity and the amount of menses in adenomyosis. Hum Reprod. 2011;26:337-345.
Citation: Nishimoto M, Fujioka T, Saito M, Saito S, Kurakata M, Sugawara J, et al. (2019) A Case of Uterine Adenomyosis that Led to the Rapid Development of Blood Coagulation Disorder Two Days after an Induced Abortion. J Blood Disord Transfus 10:425.
Copyright: © 2019 Nishimoto M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.