Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2024) Volume 12, Issue 3
A Case of Female Osteoporosis: A 50-Year-Old Postmenopausal Woman with Zoledronic Acid-Induced Uveitis
Sophy S*Received: 07-Jan-2021, Manuscript No. JP-24-7868; Editor assigned: 12-Jan-2021, Pre QC No. JP-24-7868 (PQ); Reviewed: 26-Jan-2021, QC No. JP-24-7868; Revised: 19-Aug-2024, Manuscript No. JP-24-7868 (R); Published: 16-Sep-2024, DOI: 10.35248/2329-6887.24.12.485
Abstract
Zoledronic Acid (ZA) is a third-generation bisphosphonate, most commonly used for the treatment of several conditions like postmenopausal osteoporosis, metastatic disease to the bone, hypercalcemia, Paget’s disease and multiple myeloma. In this study, we describe a 50-year-old lady who developed eye pain and redness after zoledronic acid infusion, given for controlling hypercalcemia, when she presented with hypercalcemia induced pancreatitis.
Keywords
Zoledronic acid; Bisphosphonate; Postmenopausal osteoporosis; Hypercalcemia
Introduction
Uveitis is a sight-threatening disease with intraocular inflammation that arises from various causes. Uveitis is a rare complication of zoledronic acid. Proinflammatory cytokines such as TNF alpha and IL-6 may play a role in the pathogenesis of zoledronic acid-related uveitis. Zoledronic acid is a wellestablished and well-tolerated therapy [1]. Though a flu-like syndrome is well described in the literature, there aren't too many reports of this drug causing an ophthalmic ADR. Here we present a case report of zoledronate induced acute anterior uveitis.
Case Presentation
A 50-year-old post-menopausal lady, homemaker, married and has two children was admitted with complaints of abdominal distension and pain radiating to the back for 4 days [2]. She had multiple episodes of vomiting 4 days back which was managed conservatively in a nearby hospital. She had associated breathlessness on the day of admission. She had a history of a similar episode 6 months prior and was diagnosed to have acute severe pancreatitis. She was evaluated then and was found to have hypercalcemia. However, this was not investigated further. There was a history of renal calculi in the past. There was no history of fractures, however. She had remained asymptomatic till the recent episode. Her biochemistry confirmed parathyroid hormone-dependent hypercalcemia (Table 1) [3].
| Laboratory investigations | Lab reports | Normal range |
|---|---|---|
| Parathyroid Hormone (PTH) | 412.5 pg/dl | 6-80 pg/dl |
| Calcium | 11.2 mg/dl | 8.70-10.70 mg/dl |
| Albumin | 4.02 | 3.50-4.80 |
| Vitamin D | 20 ng/ml | 30.0-100.0 ng/ml |
| Creatinine | 0.34 mg/dl | 0.50-1.20 mg/dl |
Table 1: Lab report.
Acute pancreatitis was managed conservatively and she was started on calcium lowering measures. She was hydrated well and was given the first dose of zoledronic acid 4 mg in 100 ml saline as a slow intravenous infusion. She tolerated the same well. She was then discharged, with the warning to expect a flu-like syndrome.
She did develop fever, myalgia and headache 24 hours later, suggesting a flu-like syndrome related to the drug. This was managed with paracetamol. Next day symptoms worsened and she developed redness of both eyes along with pain and photophobia. Her symptoms did not improve with topical measures and on day 5 of symptoms, she was evaluated by an ophthalmologist (Figure 1).
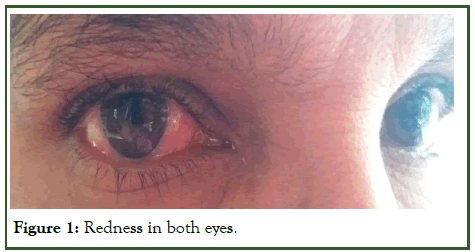
Figure 1: Redness in both eyes.
Ophthalmology examination showed a best-corrected visual acuity of 6/6 both eyes. Conjunctival and circumcorneal congestion were seen in both eyes, along with 1-2+ cells and 3+ flare in the anterior chamber. Posterior synechiae were also seen. Her intraocular pressure was 13 mm of Hg in the right eye and 12 mm of Hg in the left eye. Fundus examination was normal in both eyes (Figure 2) [4].

Figure 2: Resolution of uveitis.
A diagnosis of bisphosphonate induced acute B/L uveitis was presumed and she was started on topical steroids and cycloplegics. Gradually her symptoms improved. On review, on the 10th day of starting steroids, she was symptomatically much better. Her cornea was clear, the anterior chamber had a minimal flare, occasional cells, suggesting a resolution of uveitis [5].
Results and Discussion
Bisphosphonates are the agents in the current pharmacological arsenal against osteoclast-mediated bone loss due to osteoporosis, Paget’s disease of bone, malignancies metastatic to bone, multiple myeloma and hypercalcemia of malignancy. Bisphosphonates are structurally stable derivatives of inorganic Pyrophosphates (PPi). Zoledronic acid is a potent inhibitor of bone resorption.
Zoledronic acid inhibits osteoclast proliferation and induces osteoclast apoptotic cell death. Its potency results from its affinity for mineralized bone and especially for sites of high bone turnover. Zoledronic acid inhibits Farnesyl di-Phosphate (FPP) synthase-mediated mevalonate pathway. In the absence of FPP synthase, FPP and geranylgeranyl diphosphate are not produced, which result in inhibition of GTP binding proteins prenylation in osteoclast activity and induce osteoclast apoptosis. Furthermore osteoclast differentiation and increase bone mineralization [6].
Uveitis is the term used to describe most intraocular inflammations. The classification of uveitis into anterior, posterior and diffuse is based on the physical appearance of an inflamed eye. Diagnosis is usually on the basis of a thorough history, a review of the systemic disease known to be associated with uveitis and complete eye examination.
The adverse event of zoledronic acid-induced uveitis is very rare. Only 0.2% of patients treated with zoledronic acid developed uveitis according to Black, et al. A case report on the incidence of acute anterior uveitis after the IV administration of Zoledronate showed that 0.8% of participants exhibited mild to severe AAU after 7 days of treatment. According to Yiming Tian et al, there have been 15 cases reported since 2005. Hypocalcemia is the most common side effect of zoledronic acid. The other frequently reported adverse events include bone pain, emesis, constipation, headache, fluctuations in serum electrolyte (magnesium, calcium, phosphorous) levels, elevation in serum creatinine, Osteonecrosis of the Jaw (ONJ) and transient flu-like symptoms such as nausea, myalgia, arthralgia and low-grade fever. Acute anterior uveitis induced by zoledronic acid is a rare adverse reaction of bisphosphonate infusion. However, as the use of bisphosphonates is increasing, it should be recognized that anterior uveitis might occur because of an acute-phase reaction caused by these drugs [7].
Non-infectious uveitis is usually initiated by an inflammatory stimulus in which cytokines play a central role. Inflammatory ocular diseases including uveitis are thought to have an imbalance among pro-inflammatory cytokines such as tumour necrosis factor-a (TNF-a), interferon-c (IFN-c), interleukin-1 (IL-1) and interleukin-6 (IL-6), which regulate the immune system to maintain inflammatory response. Uveitis is also characterized by a CD4 (+) T-helper 1 cells-mediated inflammation with elevations in IL-2, IFN-a and lymphotoxin and has a distinctive cytokine pattern of IL-6, IL-8, IL-13, TNF-a and IL-2 in aqueous humour.
Bisphosphonates are inhibitors of osteoclastic bone resorption. The proposed mechanism of ocular inflammation is an idiosyncratic γΔ T cell cytokine release involving IL-1 and IL-6 caused by bisphosphonates similar in structure to pyrophosphate molecules.
There are case reports where patients presented with decreased vision, periorbital swelling and hyperemia of an eye after 24 hours of zoledronic acid given for vertebral metastasis from carcinoma breast. Biomicroscopic anterior segment examination in this patient showed corneal keratic precipitates, ciliary injection and a moderate amount of cells in the anterior chamber and right anterior uveitis was diagnosed. She had improved with topical prednisolone acetate [8].
Conclusion
In conclusion, we present a case of acute bilateral uveitis after intravenous infusion of zoledronic acid for osteoporosis. Use of the Naranjo probability scale indicated a probable relation between uveitis and zoledronic acid therapy in our study. In conclusion, zoledronic acid may be associated with an inflammatory eye disease which can be successfully treated with appropriate management, if recognized early. Clinicians should be aware of this important side effect and refer these patients to an ophthalmologist. Bisphosphonate rechallenge is not fully contraindicated and prior steroid administration may be a more reasonable treatment choice according to the available evidence.
However there are a few incidents where zoledronate has caused conjunctivitis, ocular pain, scleritis, photophobia, episcleritis, blurred vision and uveitis.
The pharmacokinetic of zoledronic acid suggest that the concentration in plasma after the infusion decreases rapidly due to the increased absorption of the drug by the bone. However, small amounts of zoledronic acid can be detected in plasma several days after the infusion, representing the drug released gradually from the bone during bone turnover.
References
- Drake MT, Clarke BL, Khosla S. Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83(9):1032-1045.
[Crossref] [Google Scholar] [PubMed]
- Jacques RM, Boonen S, Cosman F, Reid IR, Bauer DC, Black DM, et al. Relationship of changes in total hip bone mineral density to vertebral and nonvertebral fracture risk in women with postmenopausal osteoporosis treated with once‐yearly zoledronic acid 5 mg: The horizon‐Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27(8):1627-1634.
[Crossref] [Google Scholar] [PubMed]
- Freitas-Neto CA, de Oliveira Fagundes WB, Ribeiro Jr M, Pacheco KD, Freitas LG, Avila MP. Unilateral uveitis with vitreous haze following zoledronic acid therapy for osteoporosis. Semin Ophthalmol. 2015;30(3):232-234. Informa Healthcare.
[Crossref] [Google Scholar] [PubMed]
- Jun JH. Acute bilateral anterior uveitis after a single intravenous infusion of zoledronic acid in metastatic breast cancer. Korean J Ophthalmol. 2017;31(4):368-369.
[Crossref] [Google Scholar] [PubMed]
- Kennedy T, Sellar PW, Vaideanu-Collins D, Ng J. Two case reports of zoledronic acid-induced uveitis. Age Ageing. 2018;47(5):754-755.
[Crossref] [Google Scholar] [PubMed]
- Tian Y, Wang R, Liu L, Ma C, Lu Q, Yin F. Acute bilateral uveitis and right macular edema induced by a single infusion of zoledronic acid for the treatment of postmenopausal osteoporosis as a substitution for oral alendronate: A case report. BMC Musculoskelet Disord. 2016;17:1-5.
[Crossref] [Google Scholar] [PubMed]
- Anandasayanan K, Malaravan M, Suganthan N. Acute unilateral anterior uveitis following zoledronic acid infusion: A case report. SAGE Open Med Case Rep. 2020;8:2050313X20944305.
[Crossref] [Google Scholar] [PubMed]
- Songur K, Bascıllar D, El O. Case report: Acute unilateral uveitis induced by infusion of zoledronic acid. Turk J Osteoporos. 2022;28(2):166-168.
Citation: Sophy S (2024) A Case of Female Osteoporosis: A 50-Year-Old Postmenopausal Woman with Zoledronic Acid-Induced Uveitis. J Pharmacovigil. 12:485.
Copyright: © 2024 Sophy S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

