Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
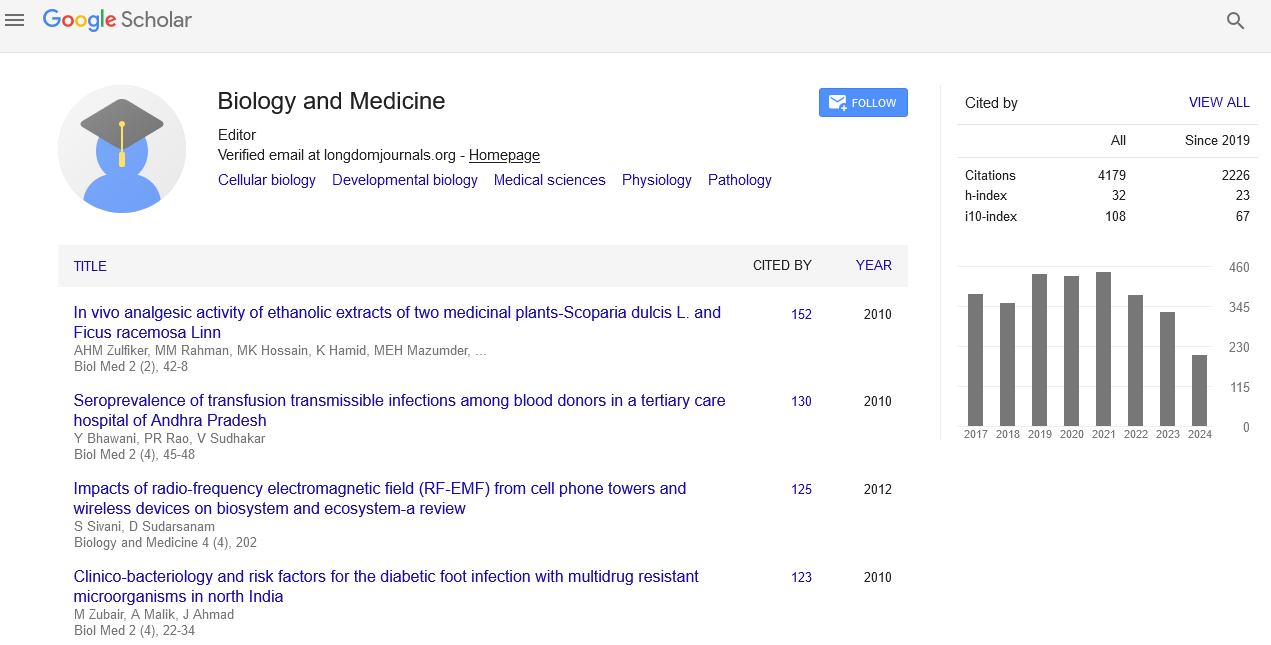
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Why Process Quality Measures may be More Valuable than Outcome Measures in Critical Care Patients
Kwadwo Kyeremanteng and Gianni D’Egidio
Background ICU is an ideal target for quality of care evaluation and initiatives because of the associated morbidity, mortality and high resource utilization of the patient population. Quality measures can be separated into structure, process and outcome. There has been longstanding debate about the ideal quality measure. Findings Structure measures are typically most valuable when good quality of care is unlikely, as it will often help illustrate glaring deficiencies. Process measures attempt to assess healthcare provider’s compliance with practices that are associated with positive outcomes. Outcome quality measures assess whether healthcare goals were realized. These measures can range from mortality, cost of care and patient satisfaction. The advantage of process measures is that data can be collected relatively quickly. Outcome measures can be rare or difficult to track; this can make the data collection process difficult. Also a larger sample size may be necessary to capture the outcome measure. Process measures frequently do not require large sample sizes and therefore allow for a quicker feedback process. Process measures also reduce the need for adjusting for severity of illness and co-morbidities, which can be time consuming and labor intensive. Conclusion It is apparent that process quality measures are the most practical, impactful and logical option for critical care patients. Outcome measures do have value but can be difficult to interpret in the critical care setting due to the heterogeneity of patients, the multiple disciplines involved in care and measures can be subjective.